This article has been
cited by other articles in ScienceCentral.
Abstract
Background
We aimed to analyze the risk factors for sudden death after diagnosis of coronavirus disease 2019 (COVID-19) in South Korea and to provide evidence for informing prevention and control interventions for patients at risk of sudden death.
Methods
We included 30,302 COVID-19 related deaths registered in the patient management information system (Central Disease Control Headquarters) between January 1, 2021, and December 15, 2022. We collected their epidemiological data recorded by the reporting city, province, or country. We performed multivariate logistic regression analysis to identify risk factors for sudden death after diagnosis of COVID-19.
Results
Among the 30,302 deaths, there were 7,258 (24.0%) and 23,044 (76.0%) sudden and non-sudden deaths, respectively. Sudden death means a person who died within 2 days of diagnosis and who did not receive inpatient treatment. Underlying condition, vaccination status, and place of death were significantly associated with the survival period in all age groups. Moreover, region, sex, and prescription were significantly associated with the survival period only in certain age groups. However, reinfection was not significantly associated with the survival period in any age group.
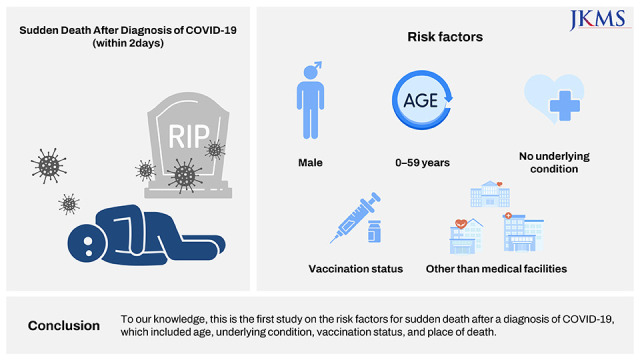
Conclusion
To our knowledge, this is the first study on the risk factors for sudden death after a diagnosis of COVID-19, which included age, underlying condition, vaccination status, and place of death. Additionally, individuals aged < 60 years without an underlying condition were at high risk for sudden death. However, this group has relatively low interest in health, as can be seen from the high non-vaccination rate (16.1% of the general population vs. 61.6% of the corresponding group). Therefore, there is a possibility for the presence of an uncontrolled underlying disease in this population. In addition, many sudden deaths occurred due to delayed hospital visits to continue economic activities even after the onset of COVID-19 symptoms (7 days overall vs. 10 days average for the group). In conclusion, ‘continued interest in health’ is a key factor in avoiding sudden death in the economically active group (under 60 years of age).
Keywords: COVID-19, Epidemiological Investigation, Sudden Death, Male, Underlying Condition, Unvaccinated, Hospitalization
INTRODUCTION
In January 2020, the World Health Organization (WHO) declared the spread of coronavirus disease 2019 (COVID-19) a Public Health Emergency of International Concern; subsequently, it was declared a global pandemic on March 11, 2020.
1 Worldwide, there have been 661,545,258 cases (as of January 1, 2023) and 6,700,519 deaths.
2 To prevent the spread of the COVID-19 virus and minimize its impact, countries have implemented various infectious disease prevention and control policies, including vaccination.
3
Several risk factors for death from COVID-19 have been reported, including underlying diseases such as chronic obstructive pulmonary disease, lung disease, cardiovascular diseases, and neurological diseases
456 as well as male sex and age ≥ 65 years.
57 Furthermore, studies have demonstrated the effectiveness of COVID-19 vaccination in preventing death.
89
In response to the COVID-19 pandemic, the South Korean government implemented infectious disease prevention and control policies, including social distancing and vaccination for COVID-19, which have been notably successful.
10 In South Korea, the response to COVID-19 response can be typically classified into five stages—test, diagnosis, quarantine, treatment, and survival/death. Generally, the treatment stage is reached 2 days after a diagnosis. There has been a decrease in the incidence of severe COVID-19 and the corresponding mortality rate with the introduction of vaccines and treatments as well as stabilization of the COVID-19 response structure. However, deaths from COVID-19 continue to occur, with some occurring even before the patient enters the treatment stage.
There have been no studies on characteristic differences between patients who die ≤ 2 days (“sudden death”) and > 2 days (“non-sudden death”) after diagnosis of COVID-19. Accordingly, we aimed to analyze risk factors for sudden death by age group, which could inform the establishment of prevention and control interventions for patients with COVID-19 at risk of sudden death.
METHODS
Data sources
Under the Infectious Disease Control and Prevention Act, this study used current information regarding confirmed cases and deaths reported on the Korea Disease Control and Prevention Agency (KDCA) COVID-19 patient management information system.
Data collection
COVID-19 death reports are reported through the patient management information system (Central Disease Control Headquarters) and go through approval process according to the steps by medical institutions, public health centers, public health department of cities/provinces, and the KDCA. According to the information of the deceased reported in the death report system, additional investigations are conducted at KDCA regional centers. During further investigation, missing information such as underlying disease, date of confirmation, place of death, and vaccination history are collected and reconfirmed through medical facilities and public health centers. The data for which the investigation has been completed are finally counted after confirming that they are COVID-19-related deaths in consideration of the medical staffs’ judgment.
Definition
“COVID-19 confirmed case” refers to a patient diagnosed by a doctor as exhibiting COVID-19 symptoms and having a positive result on the rapid antigen test (performed by medical professionals) or polymerase chain test (emergency use authorized product) in accordance with the COVID-19 response guidelines.
11
“COVID-19 death” refers to a death of a patient diagnosed with COVID-19 that is by the health center or medical facility to the patient management information system (Central Disease Control Headquarters), with the exclusion of unnatural deaths. Specifically, it includes people who 1) died during the quarantine period after testing positive for COVID-19, 2) tested positive for COVID-19 after death, and 3) died after the quarantine period but were considered to die from COVID-19 based on medical opinion.
11
Participants
We included 30,302 cases of death from COVID-19 that were registered in the patient management information system between January 1, 2021, to December 15, 2022. Since there were only 930 deaths related to COVID-19 in 2020, they were excluded from this study.
Explanation of variables
Based on the duration from diagnosis to treatment, sudden and non-sudden death were defined as deaths within and after 2 days of a test, respectively. In this study, sudden death means a person who died within 2 days of diagnosis. It was considered to take 24 hours from diagnosis to confirmation, and 24 hours from confirmation to bed allocation. Sudden death, which died within 2 days of diagnosis, means a death who did not receive inpatient treatment.
Subsequently, we collected demographic characteristics such as sex, age, and region. As of January 7, 2023, the number of deaths per every 100,000 according to age group were as follows: < 6 (2.3%) deaths in the in 0–49 years age group, 15 (4.1%) deaths in the 50–59 years age group, 51 (11.3%) deaths in the 60–69 years age group, 198 (22.7%) deaths in the 70–79 years age group, and 921 (59.6%) deaths in the ≥ 80 years age group.
12 Accordingly, among our cases, we classified cases within the ages of 0–59 years (6.4%), 60–79 years (34.0%), and > 80 years (59.6%) as the low-, mid-, and high-risk groups, respectively. The region was determined based on the reporting location at the time of diagnosis and coded, where Seoul, Gyeonggi-do, and Incheon were considered metropolitan and other locations were considered non-metropolitan. The year of death was determined based on the time of occurrence and dichotomized into before (2021) and after (2022) the drastic rise in confirmed cases.
Potential health-related factors associated with mortality included underlying conditions, vaccinations, reinfections, and prescriptions; further, location of death was included as an environment-related variable. Underlying conditions were categorized based on the number of underlying conditions at death while vaccinations were categorized based on the number of vaccinations administered prior to date of diagnosis. Reinfections were defined as more than two positive tests within 45 days. The location of death was defined as medical facilities capable of treating patients with COVID-19; further, given the distinctiveness of bed-ridden patients with dementia, medical facilities were considered as designated care hospitals capable for care-giving. Non-designated care hospitals, nursing homes, emergency rooms, homes, and other locations were categorized as non-medical facilities. Prescriptions were defined as J-code prescriptions (according to the International Classification of Diseases 10th Revision) for respiratory system symptoms within 14 days before the positive test for COVID-19.
Statistical analysis
Multiple logistic regression was used to compute the odds ratios (ORs) and corresponding 95% confidence intervals (CIs) for the association between the patients’ characteristics (socio-demographic characteristics, health-related variables, and medical environment variables) and death (sudden death vs. non-sudden death). Initially, the unadjusted OR was calculated for each of the patients’ characteristics. Subsequently, we selected variables for inclusion in the multivariable model with adjusted OR (aOR) based on their clinical relevance and statistical significance in the unadjusted analyses (P < 0.05). All statistical analyses were completed using R, version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria). Statistical significance was set at P < 0.05.
Ethics statement
This research was approved by the KDCA Bioethics Committee, which waived the requirement for informed consent (2023-01-04-PE-A).
RESULTS
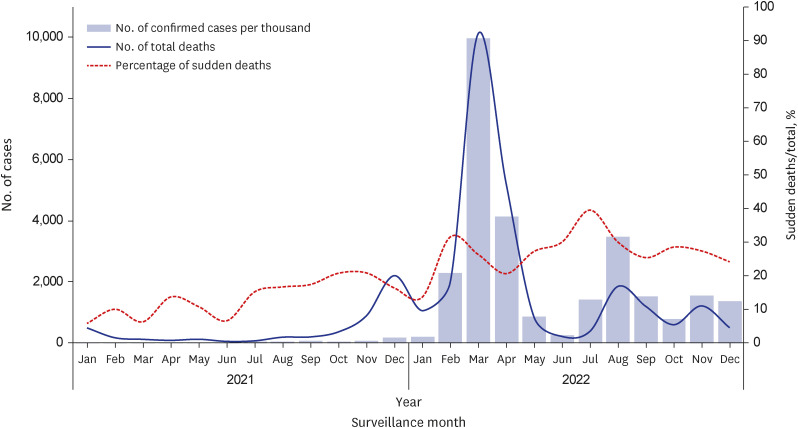
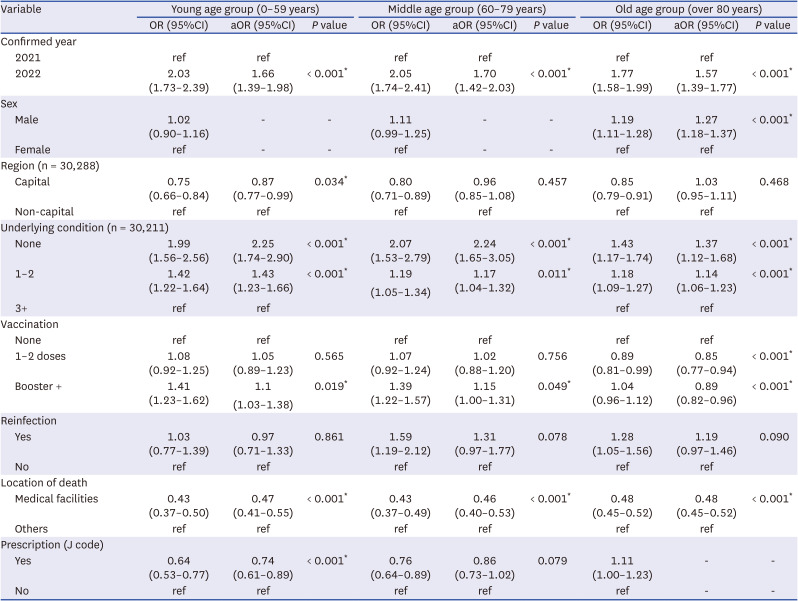
Throughout the study period, there was a consistent rate in the number of confirmed COVID-19 cases and deaths in South Korea (
Fig. 1), while the sudden mortality rate had an upward slope trend. Of the total deaths in 2021, the rate of sudden death was the highest in October and November, while it was the highest in July in 2022. Although we analyzed incidence rate of sudden death by month, we could not find month tendency of sudden death (
Fig. 1).
Fig. 1
Proportion of sudden deaths according to month.
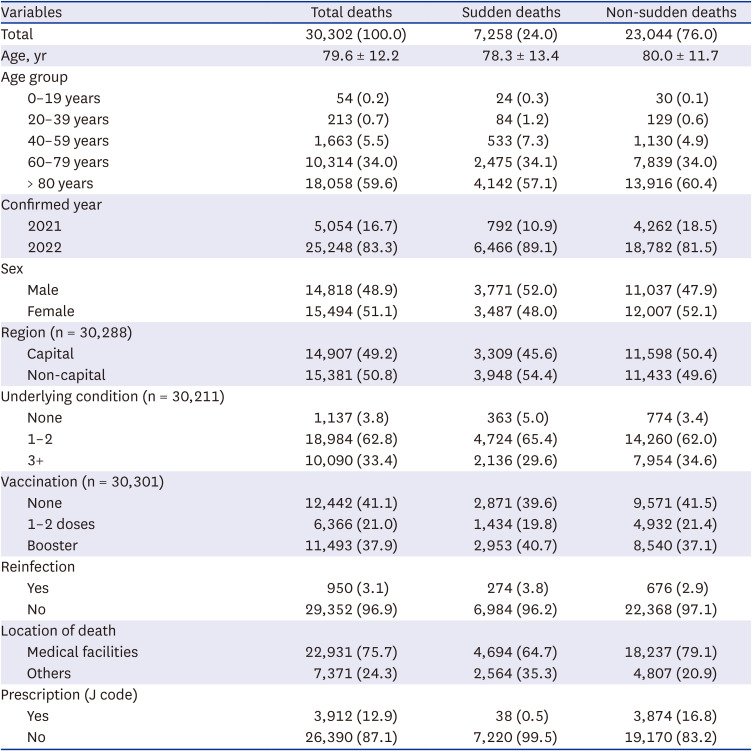
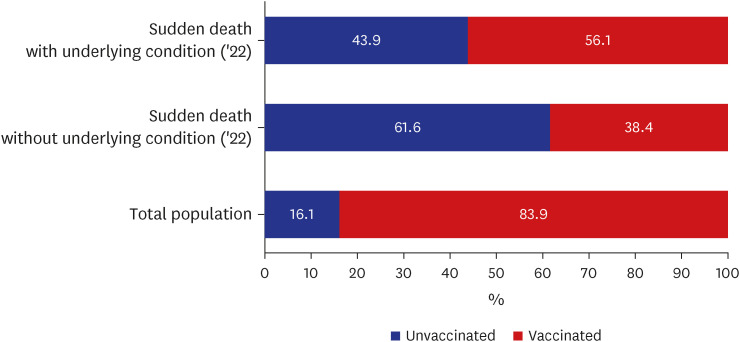
The average age at diagnosis in the total population (n = 30,302), sudden death group (n = 7,258; 24.0%), and non-sudden death group (n = 23,044; 76.0%) were 79.6, 78.4, and 80.1 years, respectively. In the sudden death group, the highest proportion of deaths occurred in the ≥ 80 years age group (n = 4,142; 57.1%), followed by the 60–79 years age group (n = 2,475; 34.1%) and 0–59 years age group (n = 641; 8.8%). (
Table 1).
Table 1
Between-group comparisons of the patients’ characteristics
|
Variables |
Total deaths |
Sudden deaths |
Non-sudden deaths |
|
Total |
30,302 (100.0) |
7,258 (24.0) |
23,044 (76.0) |
|
Age, yr |
79.6 ± 12.2 |
78.3 ± 13.4 |
80.0 ± 11.7 |
|
Age group |
|
|
|
|
0–19 years |
54 (0.2) |
24 (0.3) |
30 (0.1) |
|
20–39 years |
213 (0.7) |
84 (1.2) |
129 (0.6) |
|
40–59 years |
1,663 (5.5) |
533 (7.3) |
1,130 (4.9) |
|
60–79 years |
10,314 (34.0) |
2,475 (34.1) |
7,839 (34.0) |
|
> 80 years |
18,058 (59.6) |
4,142 (57.1) |
13,916 (60.4) |
|
Confirmed year |
|
|
|
|
2021 |
5,054 (16.7) |
792 (10.9) |
4,262 (18.5) |
|
2022 |
25,248 (83.3) |
6,466 (89.1) |
18,782 (81.5) |
|
Sex |
|
|
|
|
Male |
14,818 (48.9) |
3,771 (52.0) |
11,037 (47.9) |
|
Female |
15,494 (51.1) |
3,487 (48.0) |
12,007 (52.1) |
|
Region (n = 30,288) |
|
|
|
|
Capital |
14,907 (49.2) |
3,309 (45.6) |
11,598 (50.4) |
|
Non-capital |
15,381 (50.8) |
3,948 (54.4) |
11,433 (49.6) |
|
Underlying condition (n = 30,211) |
|
|
|
|
None |
1,137 (3.8) |
363 (5.0) |
774 (3.4) |
|
1–2 |
18,984 (62.8) |
4,724 (65.4) |
14,260 (62.0) |
|
3+ |
10,090 (33.4) |
2,136 (29.6) |
7,954 (34.6) |
|
Vaccination (n = 30,301) |
|
|
|
|
None |
12,442 (41.1) |
2,871 (39.6) |
9,571 (41.5) |
|
1–2 doses |
6,366 (21.0) |
1,434 (19.8) |
4,932 (21.4) |
|
Booster |
11,493 (37.9) |
2,953 (40.7) |
8,540 (37.1) |
|
Reinfection |
|
|
|
|
Yes |
950 (3.1) |
274 (3.8) |
676 (2.9) |
|
No |
29,352 (96.9) |
6,984 (96.2) |
22,368 (97.1) |
|
Location of death |
|
|
|
|
Medical facilities |
22,931 (75.7) |
4,694 (64.7) |
18,237 (79.1) |
|
Others |
7,371 (24.3) |
2,564 (35.3) |
4,807 (20.9) |
|
Prescription (J code) |
|
|
|
|
Yes |
3,912 (12.9) |
38 (0.5) |
3,874 (16.8) |
|
No |
26,390 (87.1) |
7,220 (99.5) |
19,170 (83.2) |
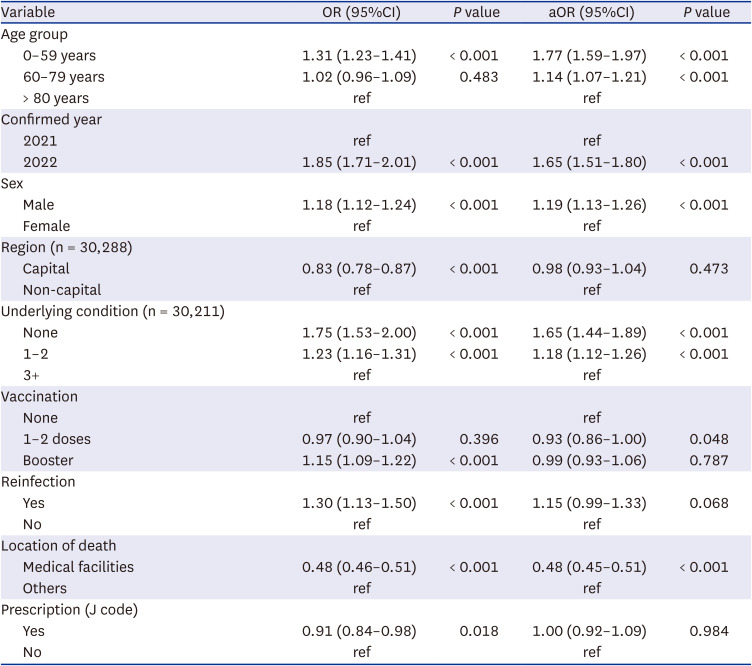
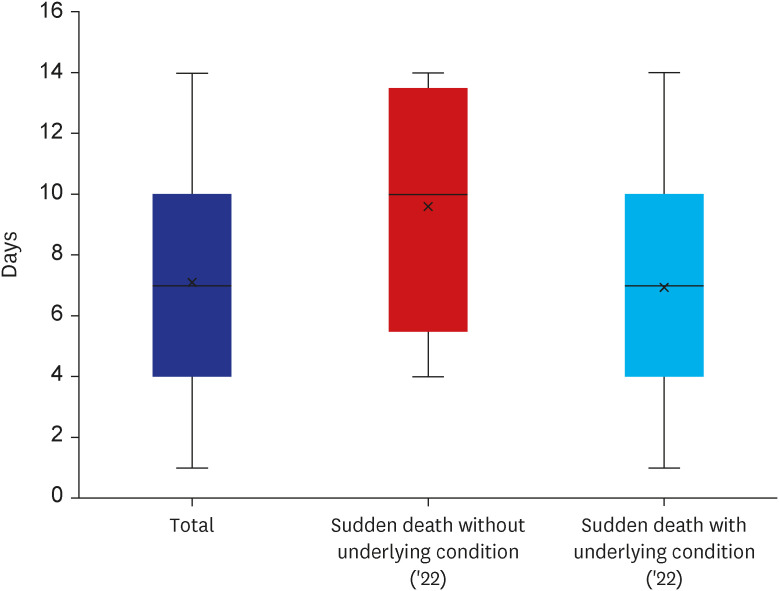
The results of the multivariable analysis are summarized in
Table 2. The risk of sudden mortality was higher in the young age group (0–59 years) (aOR, 1.41; 95% CI, 1.31–1.52) and middle age group (60–79 years) (aOR, 1.10; 95% CI, 1.02–1.17) than in the old age group (≥ 80 years). In the total population, death occurrence in 2022 (aOR, 1.65; 95% CI, 1.51–1.80) and male sex (aOR, 1.19; 95% CI, 1.13–1.26) were associated with an increased risk of sudden mortality. However, patients in medical facilities had a lower risk of sudden mortality than patients in other facilities (aOR, 0.48; 95% CI, 0.45–0.51).
Table 2
The OR for sudden death among patients who died from COVID-19 between 2021 and 2022 in South Korea
|
Variable |
OR (95%CI) |
P value |
aOR (95%CI) |
P value |
|
Age group |
|
|
|
|
|
0–59 years |
1.31 (1.23–1.41) |
< 0.001 |
1.77 (1.59–1.97) |
< 0.001 |
|
60–79 years |
1.02 (0.96–1.09) |
0.483 |
1.14 (1.07–1.21) |
< 0.001 |
|
> 80 years |
ref |
|
ref |
|
|
Confirmed year |
|
|
|
|
|
2021 |
ref |
|
ref |
|
|
2022 |
1.85 (1.71–2.01) |
< 0.001 |
1.65 (1.51–1.80) |
< 0.001 |
|
Sex |
|
|
|
|
|
Male |
1.18 (1.12–1.24) |
< 0.001 |
1.19 (1.13–1.26) |
< 0.001 |
|
Female |
ref |
|
ref |
|
|
Region (n = 30,288) |
|
|
|
|
|
Capital |
0.83 (0.78–0.87) |
< 0.001 |
0.98 (0.93–1.04) |
0.473 |
|
Non-capital |
ref |
|
ref |
|
|
Underlying condition (n = 30,211) |
|
|
|
|
|
None |
1.75 (1.53–2.00) |
< 0.001 |
1.65 (1.44–1.89) |
< 0.001 |
|
1–2 |
1.23 (1.16–1.31) |
< 0.001 |
1.18 (1.12–1.26) |
< 0.001 |
|
3+ |
ref |
|
ref |
|
|
Vaccination |
|
|
|
|
|
None |
ref |
|
ref |
|
|
1–2 doses |
0.97 (0.90–1.04) |
0.396 |
0.93 (0.86–1.00) |
0.048 |
|
Booster |
1.15 (1.09–1.22) |
< 0.001 |
0.99 (0.93–1.06) |
0.787 |
|
Reinfection |
|
|
|
|
|
Yes |
1.30 (1.13–1.50) |
< 0.001 |
1.15 (0.99–1.33) |
0.068 |
|
No |
ref |
|
ref |
|
|
Location of death |
|
|
|
|
|
Medical facilities |
0.48 (0.46–0.51) |
< 0.001 |
0.48 (0.45–0.51) |
< 0.001 |
|
Others |
ref |
|
ref |
|
|
Prescription (J code) |
|
|
|
|
|
Yes |
0.91 (0.84–0.98) |
0.018 |
1.00 (0.92–1.09) |
0.984 |
|
No |
ref |
|
ref |
|
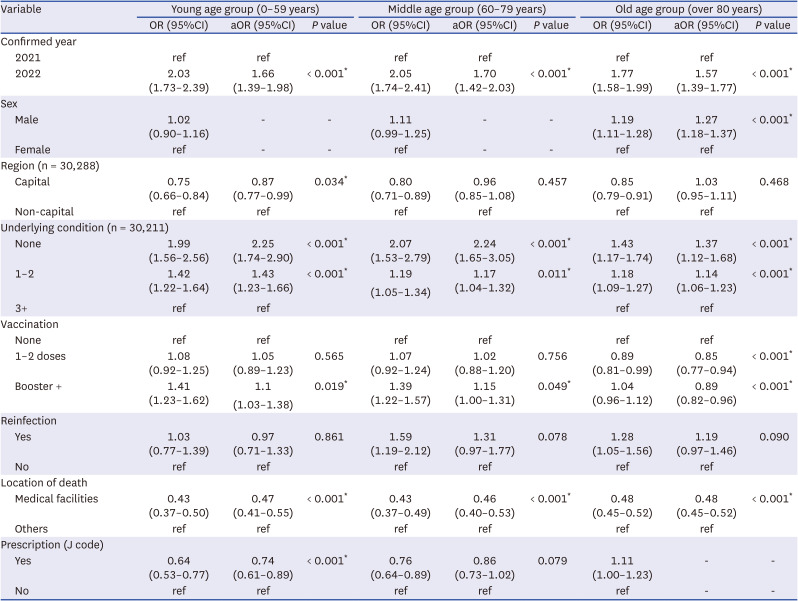
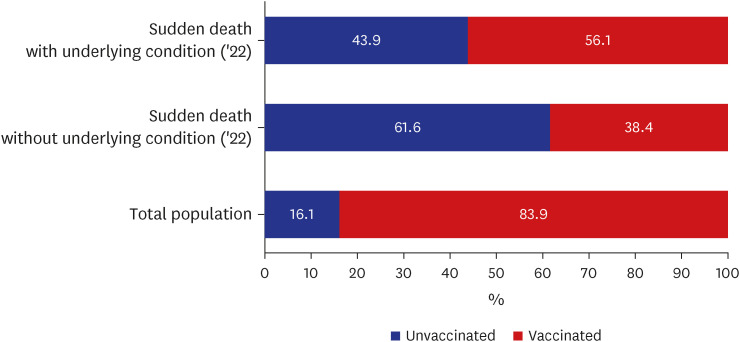
Table 3 summarizes the results of the multivariable analysis according to age group. In the 0–59 years age group, death in 2022 (aOR, 1.66; 95% CI, 1.39–1.98) was associated with an increased risk of sudden death. Patients with no underlying condition (aOR, 2.25; 95% CI, 1.74–2.90) and one or two underlying conditions (aOR, 1.43; 95% CI, 1.23–1.66) had a higher risk of sudden death than individuals with more than three underlying conditions. People who received one or more booster shots (aOR, 1.19; 95% CI, 1.03–1.38) had a higher risk of sudden death than unvaccinated individuals. However, patients with a history of J-code prescriptions (aOR, 0.74; 95% CI, 0.61–0.89) had a lower risk of sudden death than those without.
Table 3
The OR for sudden death among patients who died from COVID-19 by age group
|
Variable |
Young age group (0–59 years) |
Middle age group (60–79 years) |
Old age group (over 80 years) |
|
OR (95%CI) |
aOR (95%CI) |
P value |
OR (95%CI) |
aOR (95%CI) |
P value |
OR (95%CI) |
aOR (95%CI) |
P value |
|
Confirmed year |
|
|
|
|
|
|
|
|
|
|
2021 |
ref |
ref |
|
ref |
ref |
|
ref |
ref |
|
|
2022 |
2.03 (1.73–2.39) |
1.66 (1.39–1.98) |
< 0.001*
|
2.05 (1.74–2.41) |
1.70 (1.42–2.03) |
< 0.001*
|
1.77 (1.58–1.99) |
1.57 (1.39–1.77) |
< 0.001*
|
|
Sex |
|
|
|
|
|
|
|
|
|
|
Male |
1.02 (0.90–1.16) |
- |
- |
1.11 (0.99–1.25) |
- |
- |
1.19 (1.11–1.28) |
1.27 (1.18–1.37) |
< 0.001*
|
|
Female |
ref |
- |
- |
ref |
- |
- |
ref |
ref |
|
|
Region (n = 30,288) |
|
|
|
|
|
|
|
|
|
|
Capital |
0.75 (0.66–0.84) |
0.87 (0.77–0.99) |
0.034*
|
0.80 (0.71–0.89) |
0.96 (0.85–1.08) |
0.457 |
0.85 (0.79–0.91) |
1.03 (0.95–1.11) |
0.468 |
|
Non-capital |
ref |
ref |
|
ref |
ref |
|
ref |
ref |
|
|
Underlying condition (n = 30,211) |
|
|
|
|
|
|
|
|
|
|
None |
1.99 (1.56–2.56) |
2.25 (1.74–2.90) |
< 0.001*
|
2.07 (1.53–2.79) |
2.24 (1.65–3.05) |
< 0.001*
|
1.43 (1.17–1.74) |
1.37 (1.12–1.68) |
< 0.001*
|
|
1–2 |
1.42 (1.22–1.64) |
1.43 (1.23–1.66) |
< 0.001*
|
1.19 (1.05–1.34) |
1.17 (1.04–1.32) |
0.011*
|
1.18 (1.09–1.27) |
1.14 (1.06–1.23) |
< 0.001*
|
|
3+ |
ref |
ref |
|
|
|
|
ref |
ref |
|
|
Vaccination |
|
|
|
|
|
|
|
|
|
|
None |
ref |
ref |
|
ref |
ref |
|
ref |
ref |
|
|
1–2 doses |
1.08 (0.92–1.25) |
1.05 (0.89–1.23) |
0.565 |
1.07 (0.92–1.24) |
1.02 (0.88–1.20) |
0.756 |
0.89 (0.81–0.99) |
0.85 (0.77–0.94) |
< 0.001*
|
|
Booster + |
1.41 (1.23–1.62) |
1.19 (1.03–1.38) |
0.019*
|
1.39 (1.22–1.57) |
1.15 (1.00–1.31) |
0.049*
|
1.04 (0.96–1.12) |
0.89 (0.82–0.96) |
< 0.001*
|
|
Reinfection |
|
|
|
|
|
|
|
|
|
|
Yes |
1.03 (0.77–1.39) |
0.97 (0.71–1.33) |
0.861 |
1.59 (1.19–2.12) |
1.31 (0.97–1.77) |
0.078 |
1.28 (1.05–1.56) |
1.19 (0.97–1.46) |
0.090 |
|
No |
ref |
ref |
|
ref |
ref |
|
ref |
ref |
|
|
Location of death |
|
|
|
|
|
|
|
|
|
|
Medical facilities |
0.43 (0.37–0.50) |
0.47 (0.41–0.55) |
< 0.001*
|
0.43 (0.37–0.49) |
0.46 (0.40–0.53) |
< 0.001*
|
0.48 (0.45–0.52) |
0.48 (0.45–0.52) |
< 0.001*
|
|
Others |
ref |
ref |
|
ref |
ref |
|
ref |
ref |
|
|
Prescription (J code) |
|
|
|
|
|
|
|
|
|
|
Yes |
0.64 (0.53–0.77) |
0.74 (0.61–0.89) |
< 0.001*
|
0.76 (0.64–0.89) |
0.86 (0.73–1.02) |
0.079 |
1.11 (1.00–1.23) |
- |
- |
|
No |
ref |
ref |
|
ref |
ref |
|
ref |
- |
- |
In the 60–79 years age group, death occurrence in 2022 (aOR, 1.70; 95% CI, 1.42–2.03) was associated with a higher likelihood of sudden death than occurrence in 2021. Individuals with no underlying condition (aOR, 2.24; 95% CI, 1.65–3.05) and one or two underlying conditions (aOR, 1.17; 95% CI, 1.04–1.32) had a higher risk of sudden death compared with individuals with more than three underlying conditions. People with more than two vaccine booster shots (aOR, 1.15; 95% CI, 1.00–1.31) had a higher risk of sudden death than unvaccinated individuals.
Age > 80 years, death occurrence in 2022 (aOR, 1.57; 95% CI, 1.39–1.77), and male sex (aOR, 1.19; 95% CI, 1.12–1.26) were associated with an increased risk of sudden death. Individuals without underlying condition (aOR, 1.37; 95% CI, 1.12–1.68) and one or two underlying conditions (aOR, 1.14; 95% CI, 1.06–1.23) had a higher risk of sudden death than individuals with more than three underlying conditions. People with one or two doses and more than two vaccine booster shots (aOR, 0.85 and 0.89, respectively) had a lower risk of sudden death than unvaccinated individuals.
These findings indicated that year of death, underlying conditions, vaccination, and location of death significantly affected the survival period in all age groups. Further, region, sex, and prescription were significantly associated with the survival period only in certain age groups. Finally, reinfection was not significantly associated with the survival period in any age group.
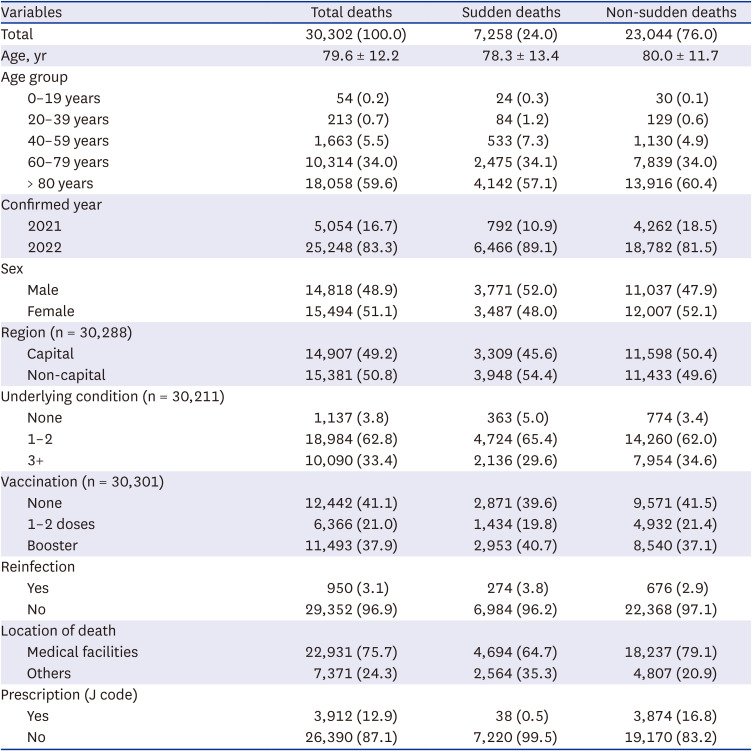
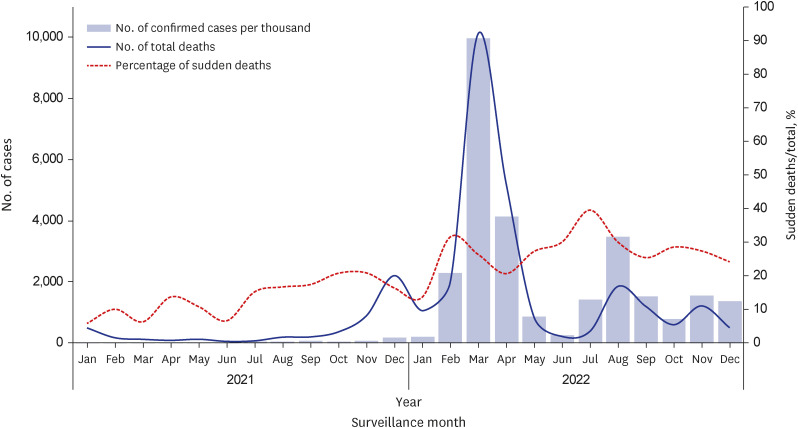
Notable, the 0–59 years age group, which has been initially termed as a low-risk group, showed the highest risk of sudden mortality. After confirming that death occurrence in 2022 and lack of underlying conditions were the strongest risk factors for sudden mortality in the 0–59 years age group, we compared the vaccination rates in this age group with those in the national population. Within this age group, the proportion of unvaccinated individuals in the general population was 16.1% while the sudden mortality rate among unvaccinated individuals without underlying condition in 2022 was 61.6% (
Fig. 2).
Fig. 2
Proportion of vaccinations among individuals aged 0–59 years.
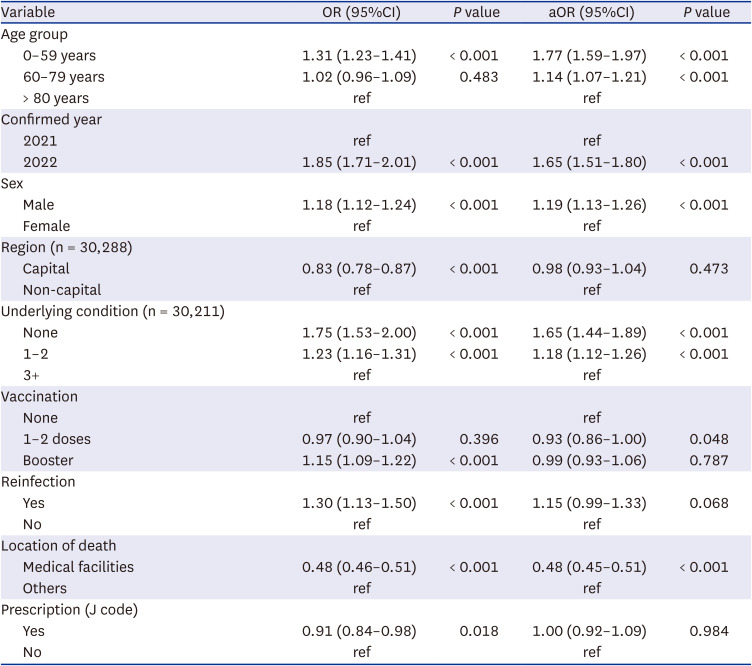
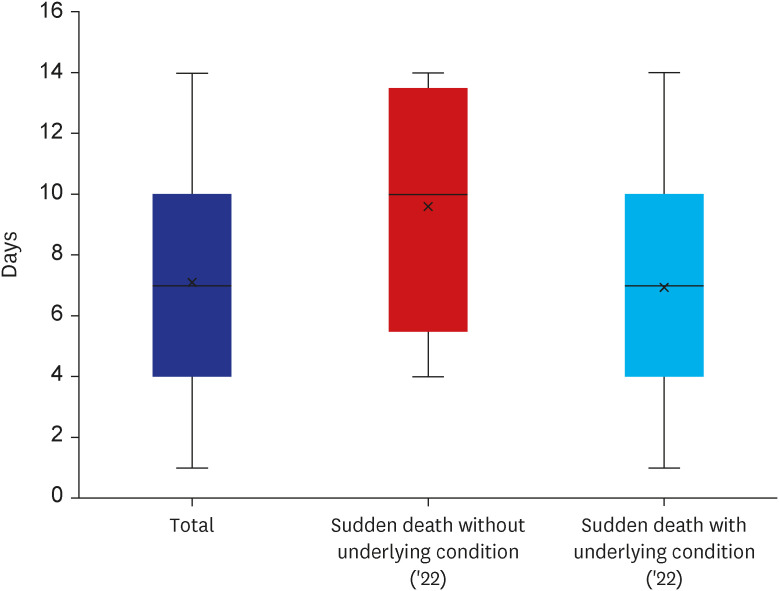
We analyzed the average duration from the J-code prescription to confirmation of a positive test. Although it took an average of 7 days from the initial prescription to confirmation for individuals with prescription history, this average duration was 10 days among individuals aged 0–59 years in the sudden death group who had no underlying conditions (
Fig. 3).
Fig. 3
Time from J code prescription to diagnosis among individuals aged 0–59 years.
DISCUSSION
This is the first study to analyze characteristics related to sudden death following a diagnosis of COVID-19. We found that younger people (aged 0–59 years) were at risk of sudden death; further, the identified risk factors differed among the age groups.
In all age groups, death occurrence in 2022 had a higher likelihood of being sudden death than occurrence in 2021. This could be attributed to the emergence of the omicron variant in 2022, which involves relatively low severity but high transmission, and thus resulting to more deaths and a higher number of sudden deaths in 2022 than those in 2021. Regarding the location of death, patients who died in medical facilities where professional treatment was available had a relatively lower risk of sudden death. This demonstrates the importance of the medical system since it implies that settings with a less established medical system have an increased risk of sudden death in. Thus, it is important to establish an infrastructure for treating patients with COVID-19 outside of specialized medical facilities and a response system that allows prompt access of emergent patients to the medical system.
Contrastingly, we found that patients with underlying medical conditions had a relatively lower risk of sudden death. This could be attributed to the relatively easier access to medical facilities by patients with underlying medical conditions, where they can be more frequently tested for COVID-19. However, this could also be due to the fact we included all types of diseases rather than diseases related to COVID-19. Thus, future studies that categorize the underlying conditions are warranted.
Although receiving one or more booster vaccination shots was significantly associated with sudden mortality in the 0–59 and 60–79 years age groups, this finding should be interpreted cautiously since the CI for each age group was close to one. Among patients aged ≥ 80 years, regardless of the number of vaccination shots, vaccinated patients had a decreased risk of sudden death, which suggests that vaccination may decrease the risk of sudden death among older individuals.
Our findings suggested that an age of 0–59 years could be crucial factor of sudden death after a diagnosis of COVID-19. Further, individuals who received J-code prescriptions had a decreased risk of sudden death. Specifically, our findings suggested that taking prescribed medication for allopathic treatment increased the duration from prescription to confirmation from 7 to 10 days.
However, the increased duration from prescription to confirmation among individuals aged 0–59 years can increase the risk of spreading COVID-19 due to delayed diagnosis. Additionally, individuals aged 0–59 years tend to avoid testing for COVID-19 in order to maintain their daily lives.
12 Accordingly, the government should implement tailored policies that facilitate rapid diagnosis to allow maintenance of daily life and stigma prevention. Moreover, individuals aged 0–59 years showed a substantially high rate of non-vaccination, which indicates the need for tailored efforts to increase the vaccination rate in the young healthy generation.
We found that individuals aged 0–59 years without underlying conditions had a high risk of sudden death. This could be attributed to young healthy individuals without underlying conditions tend to be confident about their health and have relatively low interest in health, which lead to them to being unvaccinated and delay testing for COVID-19. Accordingly, sudden death in the young healthy generation can be mitigated by active testing and treatment, with strong recommendations for vaccination and visits to medical facilities upon appearance of symptoms. In conclusion, ‘continued interest in health’ is a key factor in avoiding sudden death in the economically active group (under 60 years of age).
This study has several limitations. First, the cause of sudden death was analyzed based on information collected at the point in time. Therefore, in future studies, it is necessary to utilize detailed data of a wider range of items, including J code data of the deceased in 2020, body mass index, smoking status, etc. Second, we could not precisely determine the duration from disease onset to death since we could not identify the dates of symptom onset for all cases; therefore, the infection period was unclear. In particular, in the case of post-confirmed cases, it is impossible to investigate the dates of symptom onset. Third, the types of vaccines varied across individuals; moreover, their effects vary depending on the individual's characteristics and the timing of vaccination. Fourth, the age range of < 60 years was relatively wide; however, the total number of deaths was small; therefore, we could not analyze age sub-groups within this age range. Further studies addressing these limitations are warranted to accurately identify the cause of sudden deaths.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download