Blood culture is the most crucial test for the diagnosis and treatment decision of bacteremia. If blood culture samples are contaminated during collection and inoculation, antimicrobial agents may be administered to patients unnecessarily, thereby compromising the validity of test results.
1 Blood culture contamination can be avoided by disinfecting the skin to minimize skin flora, wearing sterile gloves, and strictly observing the aseptic technique during phlebotomy.
12 Healthcare personnel treating coronavirus disease 2019 (COVID-19) patients should wear personal protective equipment (PPE) such as gowns, gloves, masks, and face shields to prevent infection,
3 which may impede adherence to sterilization guidelines. Blood culture is an important test in febrile COVID-19 patients, and the demand for blood culture has surged during the early pandemic.
4 The previous studies reported increased blood culture contamination rates during the COVID-19 pandemic compared to the preceding pandemic,
5678 but comparative studies during the COVID-19 pandemic are rare. This study aims to evaluate the effect of wearing PPE on implementing sterilization guidelines by comparing the blood culture contamination rate of COVID-19 quarantine patients and that of general patients.
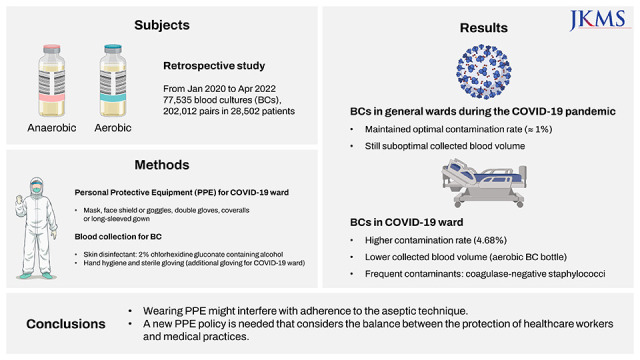
We evaluated the contamination rate of blood cultures conducted at a 1,800-bed teaching hospital in the Republic of Korea from January 2020 to April 2022. For blood collection, the skin was disinfected with 2% chlorhexidine gluconate containing alcohol. Blood was collected after hand hygiene and wearing sterile gloves. In the COVID-19 ward, healthcare workers treated severe COVID-19 patients while wearing coveralls or long-sleeved gowns and double gloves for PPE. Blood was collected after wearing additional sterile gloves. Throughout the study, experienced dedicated nurses from both the COVID-19 ward and general ward collected blood samples for blood culture. Blood drawn in intensive care units (ICUs) was carried out by an intern until February 2021 and by a dedicated nurse from March 2021 onward. Collected blood was incubated with the BACT/ALERT VIRTUO system (bioMérieux, Durham, NC, USA) or the BACTEC FX system (Becton Dickinson, Sparks, MD, USA). Clinical microbiological laboratory procedures did not change during the study period. Cases in which more than two pairs of blood were collected per day were included, and the definition of contaminants followed the Clinical & Laboratory Standards Institute guideline.
2 Blood culture contamination was defined as the identification of skin commensal such as coagulase-negative staphylococci (CoNS),
Cutibacterium acnes,
Micrococcus spp., viridans group streptococci,
Corynebacterium spp.,
Aerococcus spp., or
Bacillus spp. in only one pair of blood samples per day from a patient.
Rates were presented as frequencies and compared by the pairwise chi-squared tests. Continuous variables were presented as median and interquartile range and compared by the pairwise Mann-Whitney U tests after a significant Kruskal-Wallis test. P values were adjusted by the Bonferroni method. 95% confidence intervals are presented as the Clopper-Pearson confidence intervals. Statistical significance was considered as P < 0.01. All statistical analyses were conducted using R 4.2.2 (R Foundation for Statistical Computing, Vienna, Austria).
During the study period of 28 months, 77,535 blood cultures (202,012 pairs) were performed in 28,502 patients.
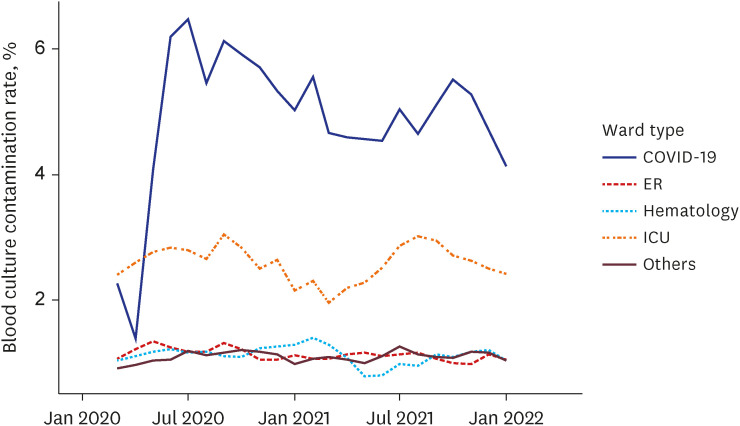
Table 1 shows the number of blood cultures, contamination rate, and positive rate by type of wards. The contamination rate of all blood cultures was significantly high in the COVID-19 ward at 4.68%, compared to ICUs at 2.56%, emergency rooms at 1.13%, hematology wards at 1.08%, and general wards at 1.07% (All of
P < 0.001). In the 6-month moving average contamination rate graph by ward type, a continuous difference in contamination rate was confirmed (
Fig. 1). The most common contaminant in the COVID-19 ward was CoNS (85.5%, 65/76), which was the same as in other wards, followed by
Bacillus spp. (6.6%, 5/76),
Corynebacterium spp. (5.3%, 4/76),
Cutibacterium spp. (1.3%, 1/76) and viridans streptococci (1.3%, 1/76). Detailed frequencies of contaminants of other wards are presented in
Supplementary Table 1.
The blood volume for blood culture is the most important factor in recovering pathogens.
2 To assess the effect of PPE wearing on collected blood volume, we compared the blood volume of peripheral blood cultures, excluding central venous blood cultures. Among them, 37,137 pairs with collected blood volume measured by BACT/ALERT VIRTUO were compared. The median volume of the aerobic blood culture bottles was 4.0 mL in the COVID-19 ward, which was significantly lower than that of the hematology wards (5.5 mL,
P < 0.001) and the general wards (5.0 mL,
P < 0.001). But there was no significant difference in the blood culture positive rate (
Table 1).
Since bacteremia can increase mortality in COVID-19 patients, it is crucial to accurately identify the pathogen using blood culture.
7 Increased contamination rates of blood culture were reported in COVID-19 patients; however, these studies conducted in US, Europe and Japan and the study periods included the epidemic waves, when the number of COVID-19 patients surged.
5678 During the COVID-19 waves, adequate infection prevention and control activities may not have been maintained due to a lack of medical resources and manpower. Due to the number of COVID-19 patients maintained at a low level through the end of 2021 in Korea, there was no shortage of medical resources for treating COVID-19 patients,
9 allowing us to evaluate the effect of wearing PPEs itself on the contamination rates of blood culture. In this study, the blood culture contamination rate of general wards has remained at an optimal level of around 1.0% throughout the COVID-19 pandemic. However, the blood culture contamination rate was higher in the COVID-19 ward than in other wards, including the ICUs. This finding suggests that wearing PPE itself might affect adherence to the aseptic technique.
Wearing PPE has played a crucial role in preventing transmission during the COVID-19 pandemic. Depending on the country, the PPE policies when treating COVID-19 patients vary, and in Korea, coveralls or gowns and double gloving were initially recommended.
10 In the early period of COVID-19 pandemic, the anxiety levels of the healthcare workers were substantial, leading in an overwhelming demand for PPE.
11 Nevertheless, as evidenced by our data, the excessive PPE might cause various adverse effects. During PPE removal, it has been found that the coveralls increase self-contamination compared to gowns.
12 Excessive PPE may impede hand hygiene practices.
13 In addition, double gloving diminishes dexterity and tactile sensitivity, which could hinder the performance of healthcare workers.
14
According to a study that comprehensively analyzed changes in blood culture during COVID-19 pandemic in the United Kingdom, an increase in contaminants by skin commensals, including CoNS was observed.
7 The relatively high proportion of contaminants caused by CoNS in the COVID-19 ward in our study was consistent with the previous findings. To the best of our knowledge, no report has evaluated the change in blood collection volume during the COVID-19 pandemic. The BACT/ALERT VIRTUO system enable to measure the blood volume in each bottle, but there is the possibility of overestimation.
15 In this study, the measured peripheral blood collection volume in aerobic bottles in the COVID-19 ward of our study was lower compared to the general and hematology wards. These findings suggest that wearing PPE and double gloving might make colleting blood more difficult.
This study has a few limitations due to retrospective design. First, we were unable to take into account all variables that could affect the contamination rate of blood culture, such as the clinical expertise of healthcare workers performing blood culture. Second, we could not investigate exactly which PPE was used by the healthcare workers who performed the blood culture in COVID-19 wards. Third, we could not include individual clinical situations because we used a single definition for blood culture contamination. We believe this is an inherent limitation of big data analysis and a limitation shared in the previous reports.
578
In conclusion, wearing PPE might impact adherence to aseptic technique and clinical performance. A comprehensive PPE policy that considers the balance between protection and medical practice is required for healthcare workers.
Ethics statement
The Institutional Review Board (IRB) at Seoul National University Hospital reviewed the study protocol and approved the study (IRB No. 2205-140-1327). The requirement for informed consent was waived due to the retrospective design of the study.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download