INTRODUCTION
The prevalence and incidence of hospital admissions have increased owing to the changing population demographics.
12 Healthcare services are continuously challenged to provide increasingly complex interventions.
3 Although some patients present with chronic wounds on admission, various types of wounds can occur in hospitals owing to the use of medical devices and medications, such as vasoactive agents.
4 According to a report, wounded patients generally occupy 27–50% of acute hospital beds on any given day.
5 This percentage is expected to increase as the population continues to age.
6 The increasing prevalence and incidence of acute and chronic wounds among hospitalized patients are major concerns.
78 Based on these factors, there will be a substantial increase in the need for wound management.
910
A key challenge for hospitals is the lack of integrated wound care services. While certain types of wounds are more likely to require specialist treatment,
1112131415 straightforward wounds caused by everyday injuries can often be treated by primary healthcare providers. Additionally, hospitals commonly treat chronic wounds of patients who cannot be provided active treatments (such as surgical debridement) or refuse major procedures because of the risks associated with underlying systemic diseases. In most tertiary centers in Korea, trained residents and/or internists in each department—rather than wound care specialists—provide wound care for patients who do not require specialist treatment. The lack of education and routine training in professional wound dressing and the huge variety of wound-dressing products, procedures, and treatments constitute potential problems.
3161718 Wound-dressing procedures vary among individuals.
19 Non-standard, inappropriate, and non-reproducible dressings enhance the difficulty in monitoring wound healing and ensuring continuity of care, resulting in poor patient satisfaction with conventional wound care systems.
20
The Korean Act to Improve the Training Environment and Status of Medical Trainees was enacted in 2015 and came into effect in December 2017.
21 Fundamentally, it aims to limit the work of training residents/interns to a maximum of 80 hours per week, thereby prohibiting continuous work lasting more than 36 hours per week. Therefore, inpatient wound care must be shared to prevent long working hours and comply with the 80-hour work-week stipulated by the Act.
2223
Therefore, an effective strategy is required to deliver high-quality care to wounded hospitalized patients. To our knowledge, no Korean hospital has a specific team responsible for non-specialist wound care. In the absence of a specialized unit, the responsibility for wound care is distributed, and dressings may be applied inconsistently. Therefore, this study sought to systematize and organize a hospital wound dressing team.
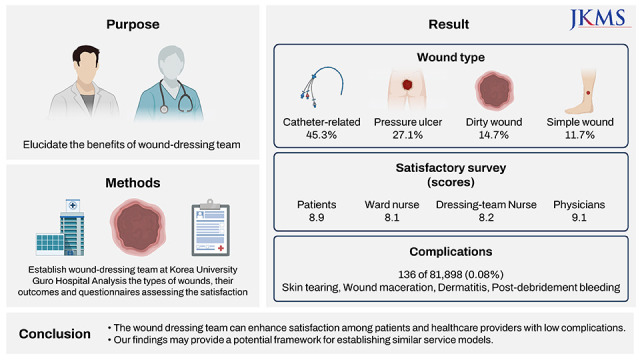
Although the existing literature has comprehensively examined the benefits of specialized wound care services and multidisciplinary team care, information on the development and integration of wound dressing teams for patients who do not require specialized wound care is scarce. Therefore, the present study aimed to elucidate the benefits of a wound dressing team by reporting our experiences with the establishment of such a team.
METHODS
Building the team
Estimating the number of patients who were likely to use the wound dressing service was a major hurdle in the initial team planning process. Therefore, a pilot team was required before establishing a formal wound dressing team. The pilot team included a medical director, a wound-specialist nurse, and two dressing nurses. They offered invaluable advice and unique perspectives based on their personal experiences to help the wound dressing team perform their responsibilities. The formal team was established in 2017 at the Korea University Guro Hospital, Seoul, a tertiary hospital with 1,075 beds.
The wound dressing team included a team director (plastic surgeon and the director of the Diabetic Wound Center), a subdirector (a board-certified plastic surgeon specializing in wound healing), a senior plastic-surgery resident, a wound-specialist nurse (coordinator of the Diabetic Wound Center), and six full-time dressing nurses.
Considering the benefit of having all team members in one location, the study team was situated in a patient ward.
Team members’ education
Training for all personnel is of utmost importance. Well-trained and respectful nurses are essential for a successful wound dressing team. Therefore, the team members underwent extensive training in wound dressing and learned about various wound dressing products and procedures. A comprehensive training program should include lessons and rigorous practice in in-hospital education during the probationary period. Particularly, each applicant required at least one year of clinical experience and three weeks of pre-clinical training to participate in this specialized nursing unit. During the first week, the dressing team mastered its primary role, learned about the referral system, and acquired basic knowledge about wound management. The training during the second and third weeks covered the probationary practice of catheter dressing and abrasion and pressure ulcer wounds, respectively.
Team members further underwent a six-month wound care program offered by the Korean Wound Management Society (KWMS). Their training program included lectures, practice, and written exams. The team members acquired professional qualifications recognized by the KWMS upon passing a test.
The wound dressing team attended weekly meetings to assess complex cases. They discussed the difficult cases that emerged during the practice, while the team director or subdirector moderated the treatment plans.
Referral system process
Administrative assistance was critical in ensuring that the institutional infrastructure could support the dressing team in providing the highest standard of care. Electronic medical records, which were installed and implemented in 2018, were modified to allow for the proper referral and documentation of patients, including the wound description and clinical photos.
When patients were admitted via the outpatient clinic or emergency department or transferred from another hospital, the ward nurses were asked to register and briefly document all their wounds, irrespective of severity. Thereafter, the clinician of the admitting department was asked to decide to whom the patient should be referred, and whether to the wound dressing team with a “wound not needing specialist care,” or the internist, or the resident in the admitting department.
If the admitting department’s clinician decided to refer the patient to the wound dressing team, the referral procedure was performed via the electronic medical record system. In the referral form, the clinician was required to indicate the wound’s location (a specific part of the body), type of dressing required (e.g., catheter or ulcer dressing), size (dimension or depth) of the wound, any underlying diseases (e.g., diabetes or chronic kidney disease), and patient’s referral department. Additionally, the form provided free text space for the clinician to elaborate the reason behind the referral.
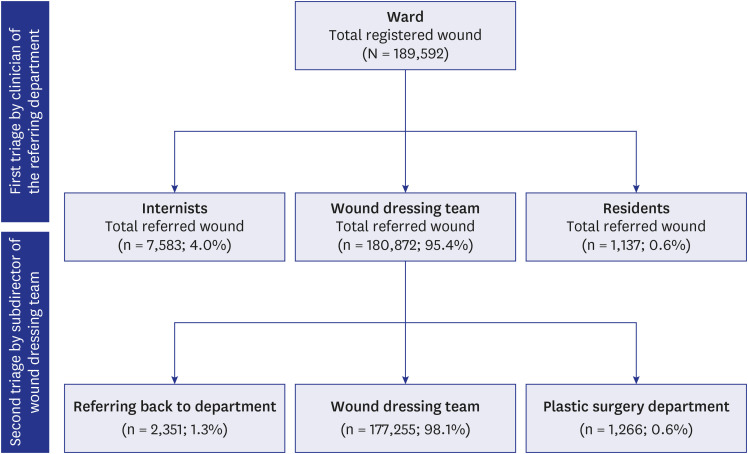
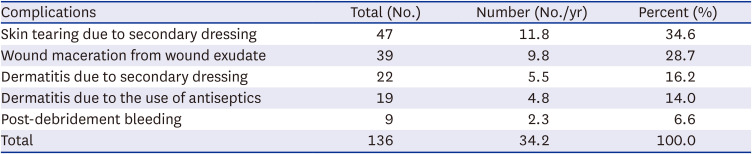
Subsequently, the subdirector of the dressing team performed a confirmation procedure based on the patient’s wound severity and general health. After undergoing this triage process, each wound was considered as requiring one of the following. Either the patient was added to the dressing team list, or returned to the department for treatment (for acute surgical wounds, tracheostomy tube-change dressing, or a potential wound suspected to be linked to other serious medical diseases), or the patient was referred to a wound specialist (e.g., a plastic surgeon). These two steps of the triage—initiated by the admitting department’s clinician and confirmed by the subdirector of the dressing team—enabled an accurate and appropriate triage based on both the patient’s wound severity and general health (
Fig. 1).
Fig. 1
A Consolidated Standards of Reporting Trials diagram illustrating the referral-triage-allocation process.
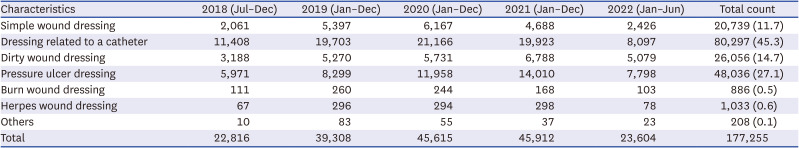
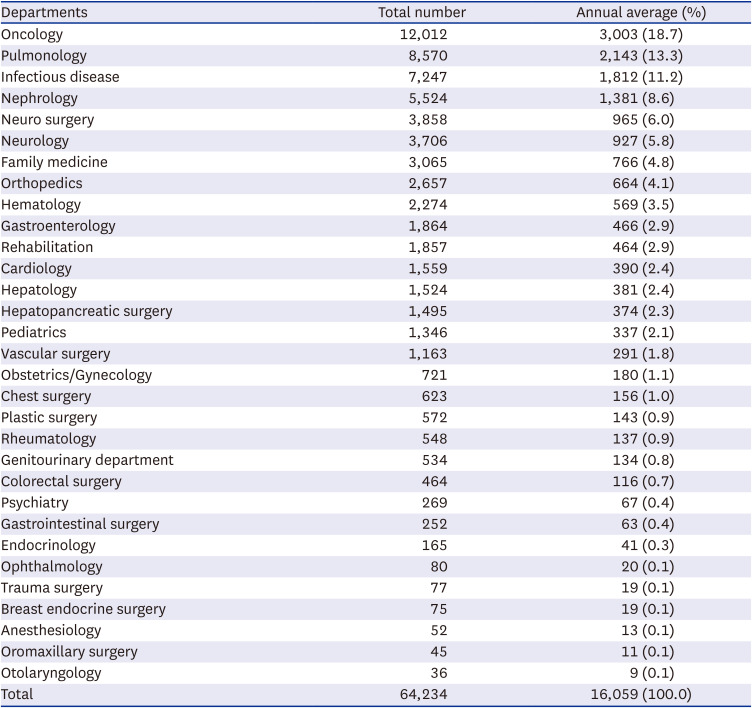
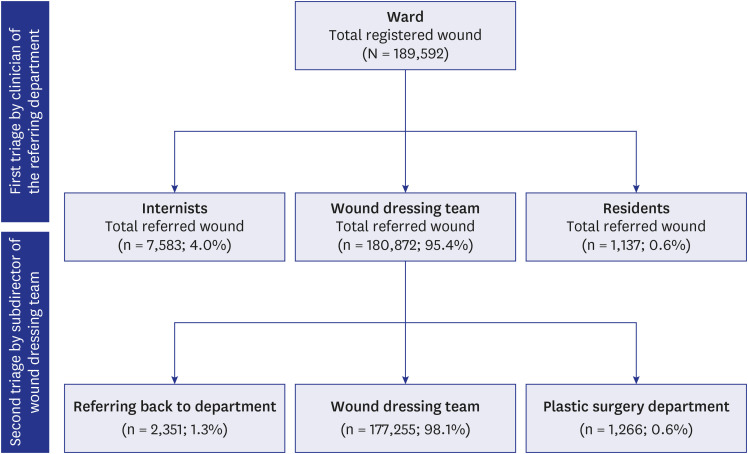
Outcome measures
Data on the number and types of wounds managed by the dressing team, referring departments, and complications were obtained from the electronic medical records. After establishing the electronic medical records-based referring system that enabled statistical investigation, data between July 2018 and June 2022 were analyzed to assess injury types and outcomes.
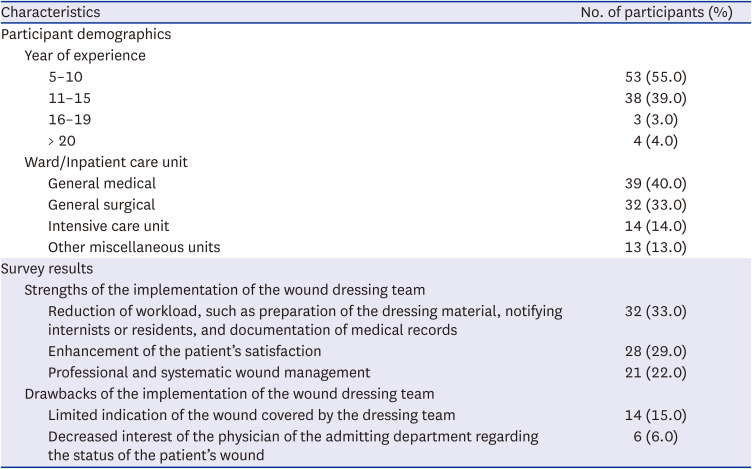
Additionally, a survey was administered using a questionnaire. Patients whose wounds were treated by the dressing team, ward nurses, dressing team nurses, and residents/internists participated in the survey. They were invited to complete a questionnaire after obtaining their informed consent. The process was conducted consecutively among patients who were admitted between May 2022 and June 2022 and were mentally stable enough to respond to the questionnaire voluntarily. Nurses with at least five years of ward experience were surveyed to compare the differences after the development of this system.
The questionnaire included a satisfaction score on a scale of 0–10 (0 = worst and 10 = optimal) regarding the experience of the wound dressing team. The survey participants were asked to describe the advantages and drawbacks of this system freely. Feedback from patients, ward and dressing team nurses, residents, and internists was collected anonymously; further, participants provided written suggestions for improvements and critiques.
Data analysis
Data from the electronic medical records were exported as an Excel file (Microsoft, Redmond, WA, USA), analyzed using IBM SPSS Statistics version 20.0 (IBM Corp., Armonk, NY, USA), and cross-checked for accuracy. Descriptive analyses were utilized, and the results were interpreted qualitatively.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of Korea University Guro Hospital (approval No. 2023GR0147). Informed consent was obtained from each subjects.
DISCUSSION
Ideally, every wound should be treated by a wound specialist to ensure the most effective treatment.
2024 However, resources for specialized wound treatment are limited in most hospitals.
25 The latest medical findings suggest that wound specialists generally prefer a more proactive and aggressive approach to wound care. In the study hospital, wound specialists (plastic surgeons and nurses specializing in wound management) mainly treat hard-to-heal wounds, such as those caused by diabetes. They provided specialized treatment and care, including surgical debridement, biologic dressings, and hyperbaric oxygen therapy.
112526272829 Therefore, the wound dressing team was established to implement a more standardized approach.
30 They cleaned the wound thoroughly to prevent infections and other complications, and applied appropriate dressings to keep the wound moist and promote healing. A dressing nurse closely monitored the wound to ensure that it healed properly. If a wound showed signs of infection or an inability to heal, the nurse consulted the director or subdirector of the team without delay.
Every hospital cannot apply a one-model-fits-all approach to establish a wound dressing team. Available human resources, patient care systems, and patient populations are context-specific. However, evidently, certain key elements are essential when developing a dressing team. Specific design and operational elements promote the dressing team’s success.
First, the team should include experienced wound specialist physicians and/or nurses who can provide appropriate care for various types of wounds. The second key element in this model is a clearly established referral mechanism. The referral process would facilitate a quick review of each patient’s wound and case, thereby allowing the team members to decide which patients to include in the wound dressing team list. Third, nurses require fairly rigorous education and training to develop the skills and knowledge required to provide appropriate dressings; thus, opportunities were given to their participating in training courses and the international congress regarding wound management. This enabled the dressing team nurses to sharpen their knowledge of wound dressing and encouraged them to be specialists as wound dressing nurses, thereby contributing to maintaining the long service of trained team nurses. Communication is another prerequisite for success. Members of the wound dressing team must be open to suggestions and provide adequate documentation to avoid misunderstandings and discrepancies. For example, members should communicate with each other during case discussions and weekly team meetings to prevent complications, and to develop treatment plans. Thus, case discussions are an essential component of effective wound care. This study further highlighted the importance of a positive culture of collegiality and cooperation within the hospital. Finally, the team should be located close to the patient wards to provide easy access to patients.
Continued wound management in the continuum of treatment plans is a top priority to achieve a consistent outcome; thus, the service provided by our dressing team continues on weekends. However, the number of on-duty nurses decreases from four out of six during weekdays to three during weekends. During weekends, all the work routinely performed during weekdays is executed, including the takeover process of wound management for every wound in the work list and documentation of wound photographs. The consultation via the group messenger or by phone within the dressing team, that is, between the subdirector, plastic-surgery residents, and dressing nurses, is also available 24 hours during weekends. However, the double triage process for newly admitted patients is suspended during weekends and resumes on Monday mornings. Newly registered dressings that are initiated during weekends by ward nurses, which have yet to be allocated and confirmed by the double triage system, are conducted temporarily by on-duty internists or residents of the admitting departments. By limiting the sudden increment of the total number of dressing lists from the newly admitted patients during the weekends, the service can be maintained with the limited personnel.
We have modified the existing system to establish the current dressing team model. In the early phase, when an electronic medical record-based referral system was not established, referrals were based on verbal or documented notifications from the referring department to the ward and dressing team or vice versa. This one-way flow limited simultaneous and concordant decisions in the practice and caused errors in delivering the opinions of each working team. Thus, we suggested the development of new modalities to enhance referrals and consultations based on an electronic medical record system. The current form of referral system was established through various modificatory steps, which expediated the “dressing-to-do” list and increased the number of patients being managed in a day.
The results revealed that the most significant advantage of implementing this service was the enhancement of the satisfaction of each section of the medical staff. Each section could save time and reduce their burden due to the systematized referral process. Dressing nurses can provide professional wound care services through the newly developed dressing materials under the guidance of the team’s wound care specialist. Ward nurses were liberated from notifying residents or internists regarding inpatient wound care. Managing pressure ulcers, which occur at any time during the patient’s hospitalization, is burdensome. Through regular and scheduled identification and protection provided by the dressing team, the deterioration of pressure ulcers could be prevented.
Notably, the Korean Act to Improve the Training Environment and Status of Medical Trainees came into effect in December 2017, and the circumstances regarding the limit on the training residents/interns’ working hours became a critical issue in Korea.
212223 Various policies implemented to regulate the working hours of trainees and strategies to modulate routine jobs—predominantly performed by internists or residents—garnered attention among the administrators of training hospitals. Inpatient wound care, which was a major routine job of internists or residents, can now be performed by the wound dressing team more professionally and efficiently by implementing this system. Before the settlement of the current system, a minor conflict between the internists/residents and nurses was unavoidable owing to the vague boundaries of their workload. However, with the aid of regular meetings to enhance mutual understanding between each section of this system, the conflict issues have diminished, and the satisfaction of each section of the medical staff has been increased. Consequently, it enhances the contentment among patients who utilize this service, along with nurses, residents, and internists.
Establishing a wound dressing team exhibits the following benefits: the team can provide professional (or at least better than average) wound dressing, thus ensuring safe, appropriate, and efficient wound care. Additionally, it can offer scheduled on-time dressing appointments and individual wound care plans, education, and regular follow-ups. Wound dressings administered by a team member will promote a continuous relationship between patients and healthcare providers, thereby improving trust and clinical outcomes. Furthermore, the wound dressing team can assume some of the burden of training residents and internists.
However, the decreased interest of physicians in the wound care of their admitted patients has been the main drawback since this system was stipulated. To overcome this drawback, our team attempted to initiate communication between the physician and the dressing team through the order communication system with proper documentation of the wound state. For example, when there is a good or bad change of the wound state in patients, the dressing team always notifies the physician in each of the admitted departments so that the physicians are aware of the change. In addition, clinical education for trainees, such as internists or residents, is another essential issue. Although the implementation of the wound management system reduced the burden of dressing, it also decreased the opportunity for wound care in practice. To overcome this, we launched and developed an educational program on wound care for the internists and residents. This program was regularly conducted by the department of education and training of the hospital, as an essential education program that every trainee has to complete each year during their training period.
The present study has limitations. Since the wound care team was established at a single academic institution, the results may not be generalizable across all practice settings. This study focused on reporting the experience of developing and integrating wound dressing teams in a single large academic medical center. Additionally, data before the establishment of the wound dressing team were not available; thus, direct comparisons of the service satisfaction, complication rates, or expenditures could not be conducted.
Based on our experience in establishing a wound dressing team, we conclude that the team can enhance patient satisfaction by providing professional wound care services and scheduled on-time dressing. Additionally, ward nurses and internists/residents were satisfied with the system because their workload was reduced. Furthermore, wound care using this system was safe. Our positive and promising outcomes are expected to provide a potential framework for establishing similar service models.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download