Abstract
A 57-year-old man with chronic kidney disease and a history of using numerous herbal medications visited Inje University Ilsan Paik Hospital for abdominal pain and vomiting. An abdominal radiograph showed diffuse small bowel distension containing multiple air-fluid levels and extensive calcifications along the colon. Computed tomography showed colon wall thickening with diffuse calcification along the colonic mesenteric vein and colonic wall. Colonoscopy, performed without bowel preparation, showed bluish edematous mucosa from the transverse to the distal sigmoid colon, with multiple scar changes. At the mid transverse colon, a stricture was noted and the scope could not pass through. A biopsy of the stricture site revealed nonspecific changes. The patient was diagnosed with phlebosclerotic colitis. After the colonoscopy, the obstructive ileus spontaneously resolved, and the patient was discharged without an operation. Currently, after 2 months of follow-up, the patient has remained asymptomatic. Herein, we report the rare case of an obstructive ileus caused by phlebosclerotic colitis with a colon stricture.
Phlebosclerotic colitis (PC) is a rare disease; chronic mesenteric ischemia that is characterized by calcification of the mesenteric vein and thickening of the colonic wall, which result in ischemic colitis.1 Ischemic colitis is primarily caused by arterial obstruction secondary to arteriosclerosis, thrombosis, or embolism in the left-sided colon. However, PC is affected by fibrosis and sclerosis of the mesenteric vein that cause colonic congestion.12 The underlying pathophysiology is unclear, but a few studies have suggested that it might be related to toxins, calcinosis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia (CREST) syndrome, Churg-Strauss syndrome, lymphocytic phlebitis, portal hypertension, cardiac disease, diabetes mellitus, dyslipidemia, or hemodialysis.34 PC usually involves the proximal colon and has no obvious cause, but certain toxins absorbed from the right-sided colon have been implicated in causing chronic venous damage.2 We report a case of PC with a transverse colonic stricture in a patient with chronic kidney disease, who had been taking multiple kinds of herbal medications for over 6 months.
A 57-year-old man visited Inje University Ilsan Paik Hospital after experiencing abdominal pain, nausea, and vomiting for 3 weeks. He had visited our emergency room for the same symptoms 2 weeks prior, where he was suspected of having paralytic ileus. However, he was discharged against our medical advice, insisting that his symptoms were not severe. His symptoms had not improved since this visit. He had chronic renal disease for 10 years. Instead of taking prescription drugs, he had been using self-manufactured herbal medication for over 6 months. The herbal medication included more than 10 herbal ingredients such as sansisi (Gardenia jasminoides), hua shi (magnesium silicate), long gu (Mastodi ossis fossilia or talc), and mu li (Ostrea gigas). He had been taking no other medication except for the herbal medicine. He was a 15-pack-year current smoker, and did not drink alcohol.
The patient looked acutely ill; his blood pressure was 132/71 mmHg, pulse rate 97/min, respiratory rate 20/min, and body temperature 36.2℃. The patient's abdomen was distended and tympanic, and showed tenderness without rebound tenderness. In addition, his bowel sounds were decreased. Laboratory tests were as follows: white blood cell 6,970/mm3, hemoglobin 8.1 g/dL, platelet count 372,000/mm3, BUN 43 mg/dL, creatinine 4.52 mg/dL, and CRP 0.3 mg/dL. The electrolyte levels were within normal limits.
A plain radiograph showed diffuse small bowel distension and colon wall calcification along the colonic area (Fig. 1A and B). Because of his reduced renal function, a non-contrast-enhanced CT scan was taken, which showed diffuse fluid-filled distension of the small bowel with colonic wall thickening and calcifications in the colon wall and at the mesocolon, suggesting atherosclerotic changes (Fig. 2). Paralytic ileus was suspected, and the patient was initially managed with supportive care including hydration, bowel rest, and nasogastric drainage. However, a follow-up CT taken on hospital day 7 did not show any improvement in bowel distention. Colonoscopy without bowel preparation performed on hospital day 8 showed diffuse bluish edematous mucosal change, multiple scarring, and loss of vascularity from the distal sigmoid to the transverse colon. There was a pinpoint stricture in the transverse colon, 65 cm from the anus, and scope passage was not possible (Fig. 3). A biopsy taken from the stricture site showed chronic inflammation and fibrosis with mild regenerative change (Fig. 4). Under the supposition of a PC diagnosis, a contrast-enhanced CT scan with delayed phase angiography was performed, which showed extensive calcifications along the colonic wall, mesenteric, and portal veins (Fig. 5). Total colectomy was recommended, but the patient refused. Fortunately, on the day after the colonoscopy, the patient's symptoms dramatically improved, and the ileus disappeared (Fig. 1C and D). Presumably, this was due to the dilatational effect from the scope passage attempt, or dislodgement of a fecalith. Based on radiologic, endoscopic, and histologic findings, we diagnosed the patient with PC. After several days of a soft diet, the patient remained asymptomatic, and was discharged. The patient is currently symptom-free, after 2 months of follow-up.
In 2000, Iwashita et al. first reported PC as a new disease entity, describing it as an ischemic lesion resulting from phlebosclerosis.5 Due to the lack of pathological inflammation, Iwashita et al.1 proposed the name "idiopathic mesenteric phlebosclerosis" (IMP) in 2003. IMP is characterized by mesenteric vein calcification and venous congestion of the colon. All of the PC patients were Asians, and their symptoms were insidious or abrupt and mainly occurred in the right hemicolon.2 Symptoms include abdominal pain, vomiting, diarrhea, hematochezia, and constipation caused by chronic venous insufficiency and venous congestion.3 To the best of our knowledge, there have been three reported cases of PC in Korea; these cases are summarized in Table 1.
Abdominal radiography shows multiple thread-like or linear calcifications mainly along the right-sided colon, and abdominal CT scan shows colon wall thickening and calcification of the mesenteric vein.6 Barium enema shows haustral disappearance, luminal irregularities, rigidity, narrowing, and thumb-printing.7 Colonoscopy findings show rigidity of the colon wall, luminal narrowing, and ulceration with dark purple-blue mucosal change.5 This color may be caused by chronic congestion with ischemia or by toxins that stain the bowel mucosa.8 Certain toxins may be absorbed by venous return from the proximal colon. Therefore, most cases of PC primarily involve the right-sided colon.9 Histologic findings include thickening of the venous walls and tortuous veins, fibrotic degeneration of the venous walls with calcifications, and markedly fibrous thickening in the submucosa of the colonic wall without hemorrhage or thrombosis of the mesenteric vein.2 However, it has been suggested that PC may have a relatively long subclinical stage, and calcification within the colonic wall and mesenteric veins at certain stages may not be seen.6 In our case, radiologic findings showed mesenteric vein calcifications, but endoscopic biopsy revealed no mesenteric vein calcifications. Since a mucosal biopsy may not be sufficient for evaluation of submucosal vessels, we thought that it was prudent to take only a small amount of tissue, since we anticipated that delayed wound healing by venous congestion and biopsy-induced bleeding could be problematic.
The underlying pathophysiology of PC is not well known, but dialysis, portal hypertension, diabetes, and vasculitis have been suggested as possible causes.34 Many studies report that PC is related to herbal medicine. Recently, after reviewing 25 cases of PC, Hiramatsu et al.8 reported that a commonly used herbal ingredient, sansisi (gardenia fruit), was correlated with PC. Our patient also had a history of longterm herbal medication usage, including sansisi (gardenia fruit). However, our patient had also been taking many other kinds of herbal ingredients, including zhi zi (G. jasminoides), hua shi (magnesium silicate), long gu (Mastodi ossis fossilia or talc), and mu li (Ostrea gigas), so it is not clear which ingredient caused PC. Another study reported that stopping herbal medicines improved the patient's symptoms.10 However, although our patient was strongly advised not to take the herbal medicines, he persistently ingested them, even during the hospital admission, due to his firm belief in the efficacy of the herbal medication.
The management of PC ranges from supportive care to surgery, based on disease severity. PC may be complicated by hemorrhage, bowel obstruction, and perforation.1112 If no other signs of bowel compromise are present, supportive care may be considered. The obstructive ileus in our patient was likely caused by the recurrent ulceration of PC, and spontaneously improved after the colonoscopy examination. The exact reason is unclear, but we believe that it may have been due to dislodgement of a fecalith, or that the scope passage attempt during the colonoscopy procedure may have caused some dilatation at the stricture site, which caused improvement of ileus. Since subsequent aggravation of colonic obstruction seemed probable, we recommended colectomy, but the patient refused. Spontaneous improvement of ileus in a patient with PC has previously been reported.6 Our patient also showed a self-limiting course after conservative care, but it is not clear whether a watchful waiting for future patients with PC should be mandatory.
In conclusion, we report a case of PC with a transverse colonic stricture in a patient with chronic kidney disease who had been taking multiple kinds of herbal medication for more than 6 months. In this patient, PC was improved by supportive care. Since PC is frequently associated with chronic kidney disease and contrast-enhanced CT is not feasible, early endoscopy seems to be required for early diagnosis of PC, especially if there are multiple calcifications found on the bowel wall. Further clinical experience is required to establish optimal treatment plans and to elucidate the prognosis of PC.
References
1. Iwashita A, Yao T, Schlemper RJ, et al. Mesenteric phlebosclerosis: a new disease entity causing ischemic colitis. Dis Colon Rectum. 2003; 46:209–220. PMID: 12576895.
2. Chang KM. New histologic findings in idiopathic mesenteric phlebosclerosis: clues to its pathogenesis and etiology--probably ingested toxic agent-related. J Chin Med Assoc. 2007; 70:227–235. PMID: 17591581.

3. Song JH, Kim JI, Jung JH, et al. A case of phlebosclerotic colitis in a hemodialysis patient. Korean J Gastroenterol. 2012; 59:40–43. PMID: 22289953.

4. Kang HY, Noh R, Kim SM, Shin HD, Yun SY, Song IH. Phlebosclerotic colitis in a cirrhotic patient with portal hypertension: the first case in Korea. J Korean Med Sci. 2009; 24:1195–1199. PMID: 19949682.

5. Yao T, Iwashita A, Hoashi T, et al. Phlebosclerotic colitis: value of radiography in diagnosis--report of three cases. Radiology. 2000; 214:188–192. PMID: 10644121.

6. Hu P, Deng L. Phlebosclerotic colitis: three cases and literature review. Abdom Imaging. 2013; 38:1220–1224. PMID: 23589075.

7. Markos V, Kelly S, Yee WC, Davis JE, Cheifetz RE, Alsheikh A. Phlebosclerotic colitis: imaging findings of a rare entity. AJR Am J Roentgenol. 2005; 184:1584–1586. PMID: 15855120.

8. Hiramatsu K, Sakata H, Horita Y, et al. Mesenteric phlebosclerosis associated with long-term oral intake of geniposide, an ingredient of herbal medicine. Aliment Pharmacol Ther. 2012; 36:575–586. PMID: 22817400.

9. Choi JM, Lee KN, Kim HS, et al. Idiopathic phlebosclerotic colitis: a rare entity of chronic ischemic colitis. Korean J Gastroenterol. 2014; 63:183–186. PMID: 24651592.

10. Hirasaki S, Matsumura K. Development of phlebosclerotic colitis under treatment with Chinese herbal therapy. Intern Med. 2014; 53:1709–1710. PMID: 25088891.

11. Chang YY, Lin HH, Lin CC. Phlebosclerotic colitis presenting as intestinal obstruction. Clin Gastroenterol Hepatol. 2014; 12:e81–e82. DOI: 10.1016/j.cgh.2014.02.018. PMID: 24561098.

12. Kato T, Miyazaki K, Nakamura T, Tan KY, Chiba T, Konishi F. Perforated phlebosclerotic colitis: description of a case and review of this condition. Colorectal Dis. 2010; 12:149–151. PMID: 19175648.

Fig. 1
Plain abdominal radiograph. Initial plain abdominal radiograph shows a diffuse small bowel ileus with multiple air-fluid levels and numerous calcification densities along the colon. (A) Supine, (B) Erect. Dramatically improved ileus, 1 day after the colonoscopy. (C) Supine, (D) Erect.
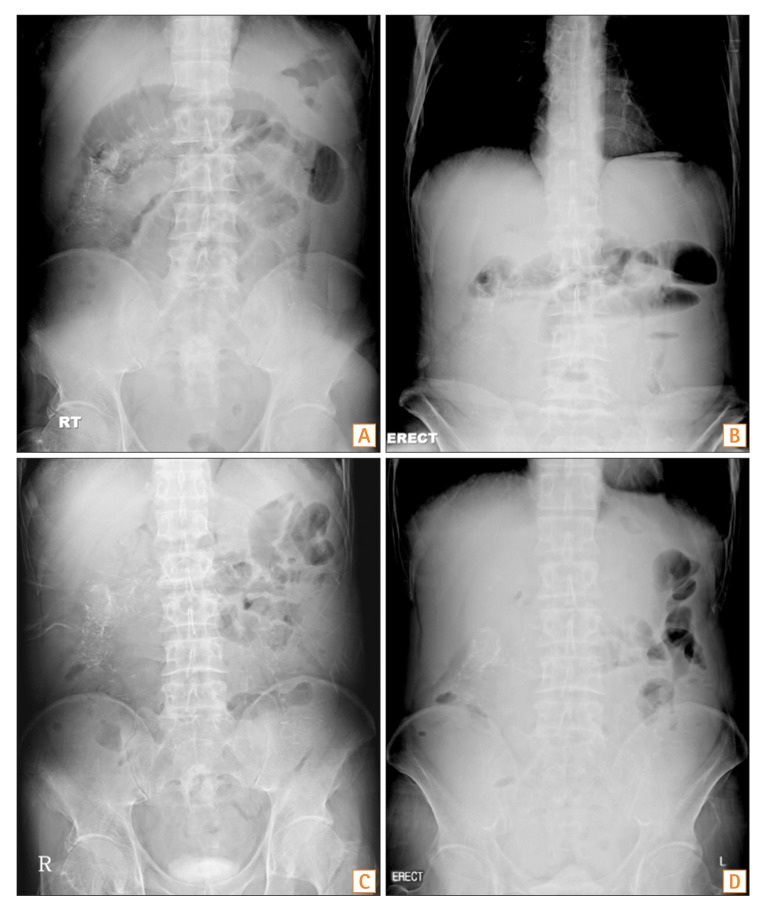
Fig. 2
Non-contrast-enhanced abdominal CT scan. (A) Diffuse fluid-filled distension of A B small bowel. (B) Colonic wall calcifications.
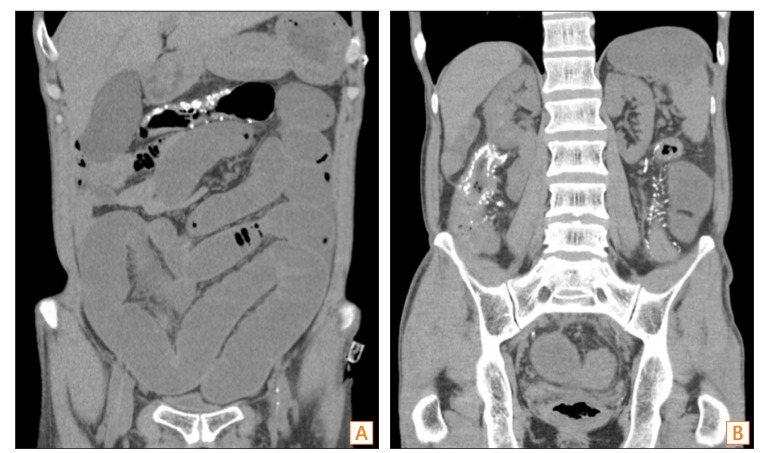
Fig. 3
Colonoscopy findings. (A) Pinpoint stricture in the transverse colon, scope passage was not possible. (B) Blue-grayish congestive change with diffuse scarring found in the transverse colon.
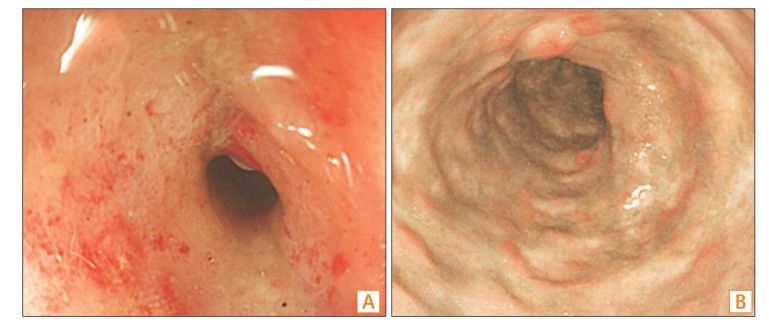
Fig. 4
Pathologic findings at the stricture site. The mucosa shows lymphoid cell infiltration and mild architectural distortion of crypts, which are suggestive of regenerative changes (H&E, ×100). No submucosal vessel was included in the specimen.
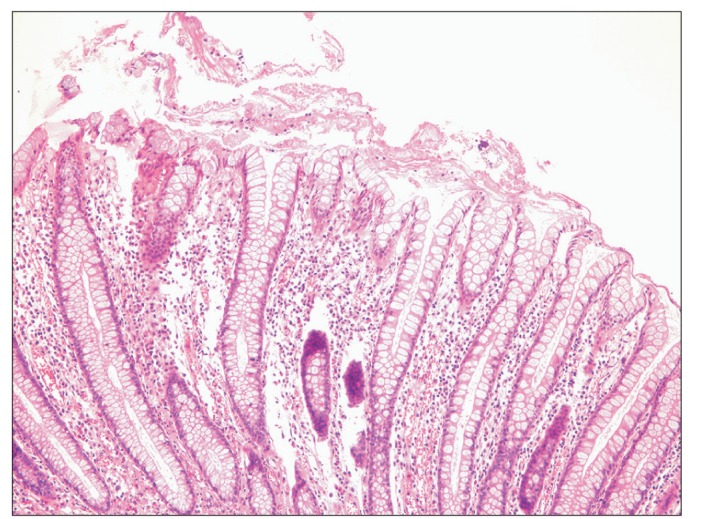
Fig. 5
Contrast-enhanced abdominal CT angiography. Abdominal CT scan shows extensive calcifications along the colonic wall (thick arrow) and mesenteric veins (thin arrow).
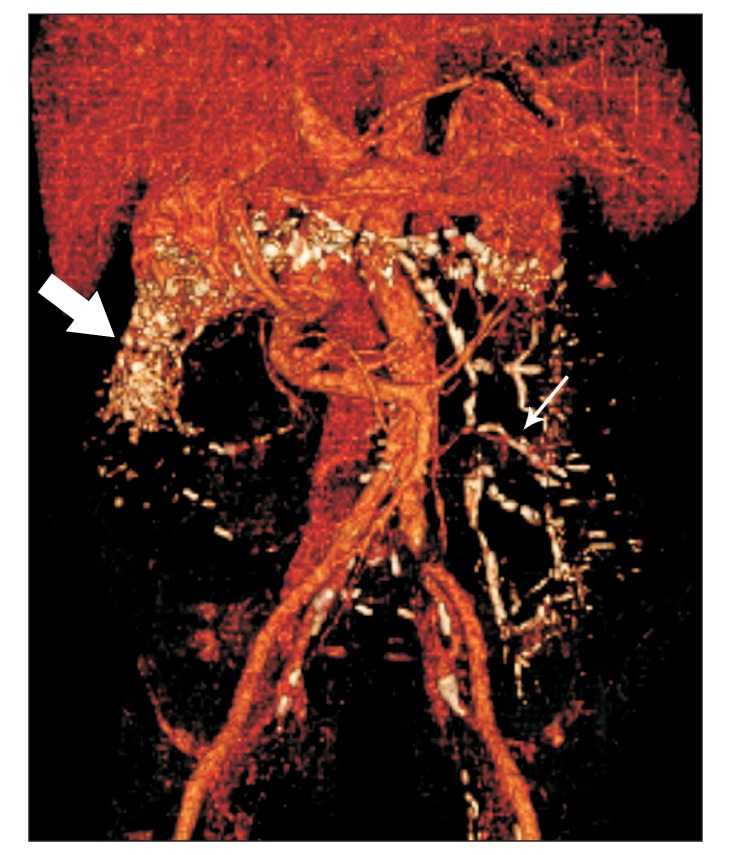
Table 1
Review of Previously Reported Phlebosclerotic Colitis Cases in Addition to Our Case
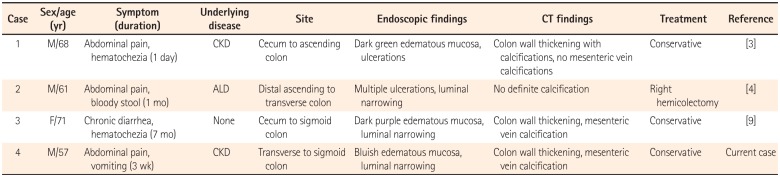
| Case | Sex/age (yr) | Symptom (duration) | Underlying disease | Site | Endoscopic findings | CT findings | Treatment | Reference |
|---|---|---|---|---|---|---|---|---|
| 1 | M/68 | Abdominal pain, hematochezia (1 day) | CKD | Cecum to ascending colon | Dark green edematous mucosa, ulcerations | Colon wall thickening with calcifications, no mesenteric vein calcifications | Conservative | [3] |
| 2 | M/61 | Abdominal pain, bloody stool (1 mo) | ALD | Distal ascending to transverse colon | Multiple ulcerations, luminal narrowing | No definite calcification | Right hemicolectomy | [4] |
| 3 | F/71 | Chronic diarrhea, hematochezia (7 mo) | None | Cecum to sigmoid colon | Dark purple edematous mucosa, luminal narrowing | Colon wall thickening, mesenteric vein calcification | Conservative | [9] |
| 4 | M/57 | Abdominal pain, vomiting (3 wk) | CKD | Transverse to sigmoid colon | Bluish edematous mucosa, luminal narrowing | Colon wall thickening, mesenteric vein calcification | Conservative | Current case |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download