Abstract
Background/Aims
Inflammatory bowel disease (IBD) management guidelines have been released from Western countries, but no adequate data on the application of these guidelines in Asian countries and no surveys on the treatment of IBD in real practice exist. Since there is a growing need for a customized consensus for IBD treatment in Asian countries, Asian Organization of Crohn's and Colitis performed a multinational survey of medical doctors who treat IBD patients in Asian countries.
Methods
A questionnaire was developed between August 2013 and November 2013. It was composed of 4 domains: personal information, IBD diagnosis, IBD treatment, and quality of IBD care. Upon completion of the questionnaire, a web-based survey was conducted between 17 March 2014 and 12 May 2014.
Results
In total, 353 medical doctors treating IBD from ten Asian countries responded to the survey. This survey data suggested a difference in available medical treatments (budesonide, tacrolimus) among Asian countries. Therapeutic strategies regarding refractory IBD (acute severe ulcerative colitis [UC] refractory to intravenous steroids and refractory Crohn's disease [CD]) and active UC were coincident, however, induction therapies for mild to moderate inflammatory small bowel CD are different among Asian countries.
Inflammatory bowel disease (IBD) incidence and prevalence have increased since the middle of the 20th Century. Several studies indicated a dramatic rise of disease incidence not only in Western countries but also in Asian countries. 12 Until now, Asian physicians treating IBD patients have referred to consensus guidelines provided by Western committees. However, Asian physicians always consider whether IBD treatment and diagnosis in Asia should be performed the same way as in Western countries because the differences in genetic background and environmental factors between Asian and Western countries are great.3 In addition, the types of approved drugs differ even among Asian countries. Under complicated circumstances, Asian physicians as well as Western physicians face common problems regarding what to do for patients with refractory IBD, such as second-line therapies for steroid-refractory UC and therapeutic strategies for refractory CD with loss of response to anti-tumor necrosis factor (TNF) therapies.
Thus, there is a growing need for a customized consensus for IBD treatment in Asian countries. For this purpose, the Asian Organization of Crohn's and Colitis (AOCC) performed a multinational survey of medical doctors who treat IBD patients in Asian countries.
Our intent is to establish optimal treatment guidelines for Asian IBD patients based on of data from a multinational survey of medical doctors treating IBD patients.
Members of the IBD Study Group of Korean Association for the Study of Intestinal Diseases (KASID) developed a questionnaire between August 2013 and November 2013. It was composed of 4 domains: personal information (9 items), IBD diagnosis (18 items), IBD treatment (30 items), and quality of IBD care (36 items). KASID officers and colleagues in China (M.H.C.) and Japan (H.N.) peer-reviewed the questionnaire. The questionnaires are shown in the Appendix. Upon completion of the questionnaire, a web-based survey was conducted between 17 March 2014 and 12 May 2014.
In total, 353 physicians from Korea, China, Japan, India, Hong Kong, Singapore, Taiwan, Malaysia, the Philippines, and Indonesia participated in this survey. Most respondents were gastroenterologists who worked in academic teaching hospitals.
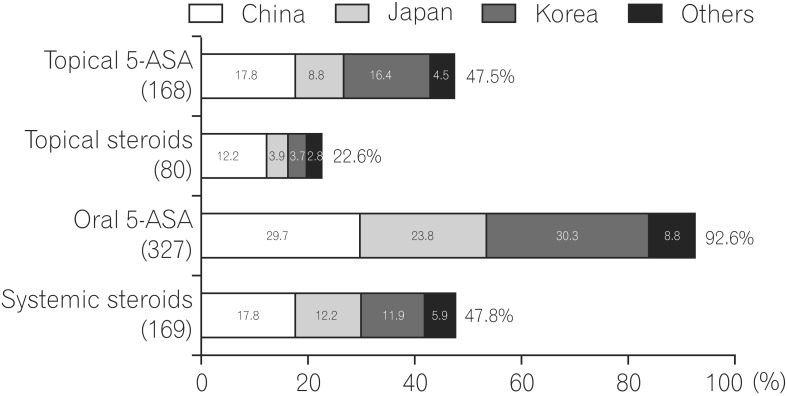
For the treatment of mild to moderate UC, topical 5-aminosalicylic acid (5-ASA) was most preferred, followed by oral 5-ASA. In patients with left-sided UC, oral 5-ASA was most preferred, followed by topical 5-ASA. Many physicians used oral 5-ASA in combination with topical 5-ASA. Among participants, Chinese physicians preferred to use topical and systemic steroids compared with physicians from other countries.
The treatment employed for mild to moderate extensive UC is shown in Fig. 1. Oral 5-ASA was most preferred, followed by systemic steroids. In comparison with treatment for left-sided UC and proctitis, systemic steroid use was preferred, although physicians might consider cases refractory to oral and topical 5-ASA.
It is very important that physicians cooperate with surgeons when managing acute severe UC. Regarding surgical consultation at treatment initiation for acute severe UC, physicians in China, Japan, and other countries always and usually consult surgeons, while physicians in Korea sometimes and rarely consult them. Data regarding this question are quite different between Korea and other Asian countries.
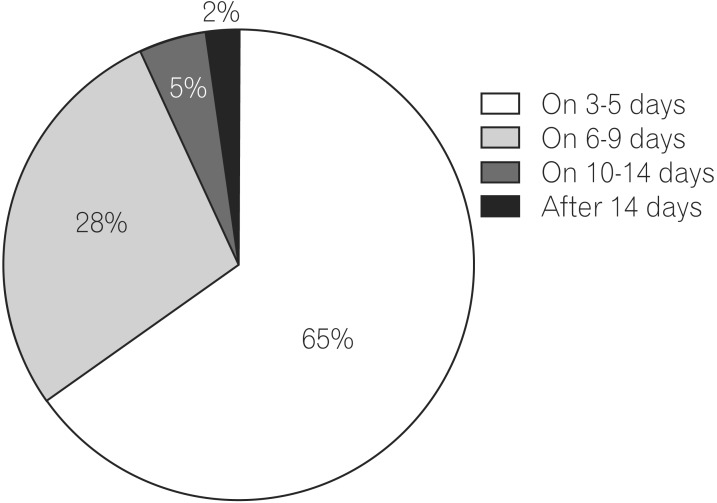
We usually use intravenous (IV) steroids for acute severe UC; however, 69% and 28% of physicians judged the therapeutic response 3-5 days and 6-9 days after initiating IV steroids, respectively (Fig. 2). Thus, 93% of physicians assessed steroid response as soon as possible because patients with acute severe UC sometimes require second-line therapy and surgical treatment.
Regarding second-line therapy for patients with acute severe UC refractory to IV steroids, many physicians in Asia except Japan selected anti-TNF therapies, followed by cyclosporine. On the other hand, Japanese physicians selected tacrolimus (TAC), followed by anti-TNF therapies. A few Japanese physicians selected apheresis therapies (Fig. 3).
This question was regarding the treatment of steroid-dependent UC. Many physicians in Asia favored the use of thiopurines. Overall, 78% of physicians selected thiopurines, and 11% of them selected anti-TNF therapies. Some Japanese physicians (3% of all participants) selected TAC and apheresis.
For steroid-refractory UC, many physicians in Asia except Japan selected anti-TNF therapies in combination with thiopurines, while Japanese physicians selected TAC, followed by anti-TNF. Overall, 44% of participants selected anti-TNF for steroid-refractory UC.
Cytomegalovirus (CMV) and Clostridium difficile infection are possible factors exacerbating UC flares. Regarding how concerned physicians are about these infections in cases of severe UC attacks, many physicians in China, Japan, and Korea always tested for CMV infection; however, only 12% of other Asian physicians always tested for it. Overall, 59% of physicians always checked for CMV infection in severe UC. In C. difficile infection, a similar tendency was observed. Thus, most physicians in Asia are likely to consider the involvement of these infections in severe attacks of UC (Fig. 4).
When we use maintenance treatment with 5-ASA, adherence to 5-ASA drugs is an important issue. This survey showed that many physicians seemed to prescribe 5-ASA two times or once daily. Overall, 54% and 15% of participants selected twice daily and once daily regimens, respectively.
For induction therapy in mild to moderate inflammatory small bowel CD, many Asian physicians considered the use of 5-ASA. Of note, survey data showed that more physicians in Japan and China selected nutritional therapy than those in Korea and other Asian countries. In addition, Japanese physicians did not prefer the corticosteroid use when treating patients with mild to moderate active small intestinal CD (Fig. 5). In cases of mild to moderate inflammatory colonic CD, a similar tendency was observed.
Regarding the treatment of severe inflammatory small bowel CD, 25% of participants selected prednisolone in combination with 5-ASA, followed by anti-TNF therapies (14%), nutritional therapy (14%), and thiopurines (13%). Only 3% of physicians selected budesonides. Physicians in Japan and China preferred anti-TNF therapies, while those in Korea preferred prednisolone.
In treating severe inflammatory colonic CD, a similar tendency was observed. Physicians in Japan and China preferred anti-TNF, while those in Korea and other Asian countries preferred prednisolone for remission induction.
These questions were regarding Asian physicians' approach towards treating steroid-dependent or refractory CD. In cases of steroid-dependent CD, most physicians preferred to use thiopurine, followed by anti-TNF therapies. However, when treating steroid-refractory CD, physicians considered using anti-TNF agents. In particular, Japanese physicians strongly favored anti-TNF agents.
We sometimes encounter cases of thiopurine-intolerant or refractory CD. Most physicians favored anti-TNF antibodies. A few physicians in China and other countries selected methotrexate (MTX).
Regarding combination therapy with anti-TNF antibodies and thiopurines or anti-TNF monotherapy for thiopurine-naïve CD patients, overall, 15% of participants always preferred combination therapy and 41% usually preferred it. Interestingly, Japanese physicians preferred monotherapy compared with physicians from other countries (Fig. 6).
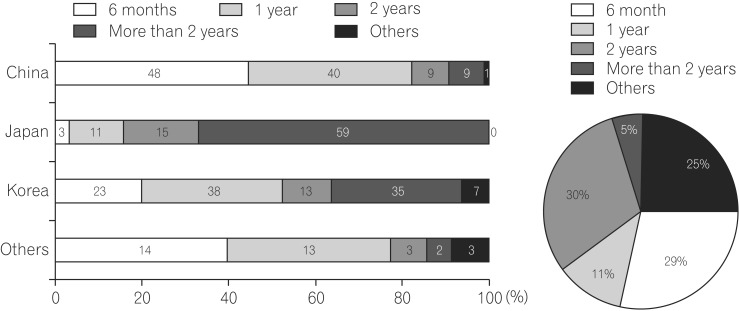
The duration of combination therapy is a clinically important issue for physicians and patients because we are always concerned about its risks. Overall, 25% and 29% of Asian physicians tended to continue combination therapy for 6 months and 1 year, respectively. In addition, Japanese physicians strongly preferred to continue combination therapy for a longer time (>2 years) (Fig. 7).
When asked how to treat non-responders to anti-TNF therapies, all physicians agreed with dose escalation, followed by changing to another anti-TNF agents. Interestingly, >40% of physicians in China favored checking serum trough levels of anti-TNF antibodies.
Most physicians favored combination therapy in CD patients whose remission was induced by anti-TNF therapies. In particular, Korean physicians favored combination therapy compared with physicians from other countries.
To monitor CD patients during treatments, most physicians used clinical activity, blood tests, and colonoscopy for disease monitoring. As for other imaging modalities, a few physicians favored CT enterography (11%), followed by magnetic resonance (MR) enterography (6%).
When asked whether they monitored 6-thioguanine nucleotides and 6-methylmercaptopurine levels, serum infliximab (IFX) levels, and antibodies to IFX (ATI), most physicians answered "No." These data indicated that facilities for routine monitoring of these values in Asia are limited.
As to when physicians performed colonoscopy for postoperative CD patients, most physicians performed it within 1 year after the operation, even in patients who did not have abdominal symptoms related to CD flares.
When asked what treatments they would consider in postoperative CD patients with moderate to severe endoscopic recurrence who had been treated with 5-ASA, many physicians selected thiopurine or anti-TNF agents. Japanese physicians preferred anti-TNF agents in comparison with thiopurines.
When asked what treatments they would consider in postoperative CD patients with moderate to severe endoscopic recurrence who had been treated with a maximum thiopurine dose, all Asian physicians agreed with additional use of anti-TNF agents.
Regarding the treatment of postoperative CD patients with moderate to severe endoscopic recurrence who had been treated with anti-TNF therapies, all Asian physicians considered additional use of thiopurine, dose escalation, or shortened intervals of anti-TNF therapies.
The present survey demonstrates that current therapeutic approaches and clinical management of IBD vary among Asian countries. First, this survey focused on UC treatment. All participants agreed with 5-ASA use for mild to moderate UC as a first-line therapy with little difference among Asian countries. In the current survey, there was no question regarding the optimal 5-ASA dose for induction and maintenance of remission or the 5-ASA types mainly used in their countries. However, meta-analysis data have already demonstrated that there do not appear to be any differences in efficacy or safety among the various 5-ASA formulations.4 In addition, a 2.4-g daily dosage appears to be a safe and effective induction therapy for patients with mild to moderate active UC. Patients with moderate disease may benefit from an initial dose of 4.8 g/day. Thus, although Asian physicians need a consensus on the optimal 5-ASA dosage for induction of remission and maintenance for UC patients, this survey showed that most physicians agreed with 5-ASA use as a first-line therapy.
The survey data from question 10 showed that many physicians prescribe 5-ASA two times or once daily because they kept the patient's adherence in mind. However, a meta-analysis showed that adherence does not appear to be enhanced by once daily dosing in the clinical trial setting.4 Whether once daily dosing of 5-ASA improves adherence in a community-based setting is unknown, and whether time-decreasing prescriptions contribute to favorable effects for UC patients might depend on not only adherence but also mucosal concentration of 5-ASA.
Despite the development of several medical therapies, acute severe UC treatment is still challenging. All participants considered consulting surgeons when treating acute severe UC. Additionally, 93% of physicians assessed steroid response within 9 days. Taken together, these data suggested that many physicians felt the importance of cooperation with surgeons for starting severe acute UC treatment and the necessity of rapid decision-making in patients with UC who fail to respond to IV steroids. The next question concerned optimal second-line therapy for patients with acute severe UC refractory to IV steroids. In general, for patients with refractory acute severe UC, after initially using IV steroids for 5-7 days, possible treatment choices included either IV cyclosporine or IV IFX. Most physicians in Asia except Japan selected anti-TNF therapies, followed by cyclosporine. On the contrary, Japanese physicians favored TAC, followed by anti-TNF therapies. A few Japanese physicians selected apheresis therapies. These survey data strongly suggested a difference in available medical treatments among Asian countries.
Which is better as a second-line therapy for steroid-refractory severe UC, anti-TNF therapy or calcineurin inhibitors (CIs)? Use of both cyclosoprine and IFX has appeared to be effective and safe as a rescue therapy compared to placebo in acute severe UC; however, data regarding head-to-head comparisons of CIs and anti-TNF agents are limited and based on retrospective observational studies. Also, no prospective studies have compared the efficacy of TAC with IFX as a second-line therapy. Minami et al.5 retrospectively assessed the short-term outcomes of 29 severe UC patients treated with TAC or IFX and concluded that the effects of TAC are potentially similar to those of IFX on severe UC, despite the limited number of enrolled patients. Overall, the rescue effect of CIs (both cyclosporine and TAC) as second-line therapies for severe UC refractory to IV corticosteroids is similar to that of IFX.6 However, how to optimally select CIs or IFX in such clinical settings remains unclear.
As for steroid-dependent UC, most physicians agree with the use of thiopurines for tapering corticosteroids. The thiopurines, azathioprine and its metabolite 6-mercaptopurine, are purine analogs that effectively maintain remission in patients with IBD, particularly in steroid-refractory or steroid-dependent disease. All participants recognized that the effect of thiopurine on refractory IBD is apparent in clinical practice. Only a few prospective studies and meta-analyses have been reported, although little is known about the long-term clinical outcomes of UC patients who initially responded to thiopurine treatment.7 Most importantly, when patients who are maintained in remission on azathioprine or 6-mercaptopurine discontinue their medications, a very high relapse rate of 70%-87% occurs.8910 In this regard, our next step is to survey how to optimize the dose of thiopurine drugs and how long we should continue thiopurines for maintenance. To establish this, we might require votes regarding the adjustment of thiopurine dose as the European Crohn's and Colitis Organization members did.11
Numerous case series have reported the involvement of CMV and C. difficile infection in patients with severe UC refractory to standard immunosuppressive therapy because the prognosis of patients with UC complicated by these infections is poor.12 Survey data demonstrated that more than half of physicians in China, Japan, and Korea always tested for CMV and C. difficile infection in refractory UC cases. CMV is often overlooked in refractory UC cases, and it is of particular importance to have an expert pathologist carefully examine mucosal biopsies for evidence of this pathogen. However, previous survey data showed that many physicians diagnosed CMV infection with antigenemia assay,13 although many experts recognized that CMV antigenemia assay was not necessarily useful for the decision to start antiviral therapy. As reported previously, the sensitivity of CMV diagnosis with histopathology in biopsy specimens was relatively low.14 Therefore, we always encounter a dilemma regarding diagnosis of CMV infection in refractory UC patients. Unfortunately, the questions of this survey did not include diagnostic criteria regarding CMV infection. In the future, we will need a consensus on the diagnosis of CMV infection in Asia. This is a big issue for clinical practice.
Survey data regarding induction therapy for mild to moderate inflammatory small bowel CD showed that many Asian physicians first selected 5-ASA. Of note, this survey revealed that more physicians in Japan and China selected nutritional therapy than those in Korea and other Asian countries. Safety and therapeutic efficacy of nutritional therapy for CD patients is well known, despite no placebo-controlled trial data.15 Whether physicians select nutritional therapy depends on patients' acceptability, convenience, and adherence. Treatment for severe inflammatory small bowel CD varied among the countries. Overall, 25% of participants selected prednisolone in combination with 5-ASA, followed by anti-TNF therapies, nutritional therapy, and thiopurines. Only 3% of physicians selected budesonides, which might differ from the tendency in Western countries. Also, the use of budesonide might be limited to the countries whose governments permit its use. Of note, physicians in Japan and China selected anti-TNF therapies, while those in Korea selected prednisolone. In treating severe inflammatory colonic CD, a similar tendency was observed. Overall, physicians in Japan and China preferred to use anti-TNF therapies, while those in Korea and other Asian countries preferred prednisolone for remission induction. The reason why preferences differed in remission induction among Asian countries remains unclear.
Treatments for steroid-dependent and refractory CD were thiopurine drugs and anti-TNF agents, which Asian physicians selected first. These results were similar to those for UC treatment. Recently, data from Western countries suggested the following factors as potential predictors of an aggressive disease course in CD: age <40 years at diagnosis, presence of perianal lesions, early need for steroids, severe endoscopic lesions, and the existence of NOD2/CARD15 mutation.16171819 In these cases, Western physicians would recommend top-down therapy with anti-TNF antibodies. Therefore, in AOCC, Asian physicians cooperate to identify the risk factors in which poor prognoses of Asian CD patients are involved to determine who requires early anti-TNF therapies.
Most physicians favored combination therapy in CD patients whose remission was induced by anti-TNF therapies. In particular, Korean physicians favored combination therapy compared with physicians in other countries. Also, Japanese physicians strongly preferred to continue combination therapy for more time. However, the optimal duration of combination anti-TNF therapies and thiopurine for CD remains unclear. The use of anti-TNF antibodies has significantly impacted the management of CD patients. Most efficacy data with these agents are limited to those collected during relatively short-term (up to 1 year) clinical trials. Because of the chronic relapsing and progressive nature of CD, clinical trial data over longer durations of treatment are desirable to demonstrate both long-term efficacy and safety of these agents.
Considering several risks of combination therapy, monotherapy might be favorable after remission induction with combination therapy. However, the outcome of anti-TNF therapy cessation for CD in clinical and/or endoscopic remission in routine clinical practice is uncertain. Louis et al. reported that approximately 50% of 115 patients with CD who were treated for at least 1 year with IFX and an antimetabolite agent experienced a relapse within 1 year after IFX discontinuation. In addition, they commented that patients with a low risk of relapse can be identified using a combination of clinical and biologic markers.20
Brooks et al. also reported that relapse rates at 1 year following elective withdrawal of anti-TNF were 36%, with high retreatment response rates. Predictors of relapse include ileocolonic involvement, previous anti-TNF therapy, and raised fecal calprotectin.21 As mentioned previously, we will need to identify several factors (clinical and biologic markers) that contribute to the cessation of anti-TNF therapies in CD patients in the future.
A recent critical issue is the therapeutic strategy for treating CD patients who lose response to anti-TNF therapy. Also, no consensus exists regarding therapies for patients with CD refractory to anti-TNF therapy and thiopurines. All physicians considered dose escalation, followed by changing to another anti-TNF agent.2223 In cases refractory to a standard regimen of anti-TNF therapies, a pharmacokinetic study measuring serum trough levels of anti-TNF antibodies, ATI, and anti-adalimumab antibodies will be required in the future, as >40% of the participants in China checked serum trough levels of anti-TNF antibodies. The survey results for question 5-3 and 5-4 showed that most physicians could not check serum trough levels of IFX, ATI, and 6TG levels in RBC. However, this monitoring is essential for optimizing treatment for individual IBD patients.
To monitor CD patients, many physicians used clinical activity, blood tests, and colonoscopy for disease monitoring. On imaging modalities for evaluating small intestinal lesions, physicians favored CT enterography, followed by 6-thioguanine nucleotides enterography. These data suggested that many Asian physicians were not familiar with using MR enterography to follow CD patients. However, the sensitivity and specificity of MRI for the detection of active disease and correlation with segmental endoscopic disease severity and detection of complications are high, with >80% sensitivity and >90% specificity. MRI also has been a valuable tool in the assessment of response to therapy; pathological improvements in MRI scans related to disease activity are responsive and reliable indicators of endoscopic healing.2425 Considering the radiation exposure by CT enterography, MRI might become the first modality for evaluating small intestinal lesions in CD patients. However, accumulation of more clinical data regarding the advantage of MRI as an imaging modality is necessary.
Postoperative management of CD patients is very important to avoid repeated surgery.2627 Most physicians recognize the necessity of early detection of endoscopic recurrence in postoperative CD patients with no clinical symptoms because they consider performing colonoscopic examination within 1 year after the operation. In addition, survey data regarding medical treatments in cases of postoperative CD with moderate to severe endoscopic recurrence showed that Asian physicians considered using thiopurine or anti-TNF agents, although Japanese physicians preferred to use anti-TNF agents in comparison with thiopurines. In cases of postoperative CD patients with moderate to severe endoscopic recurrence who have been treated with anti-TNF antibodies, all Asian physicians selected additional thiopurine use, dose escalation, or shortened intervals of anti-TNF treatment. It is natural that most physicians agree with the use of two medications for postoperative CD with moderate to severe endoscopic recurrence. In this regard, a future clinical issue is how to identify patients who need biologics, thiopurines, or both in postoperative CD.
In summary, the current survey results demonstrated the treatments of UC and CD in Asian countries, suggesting that most therapeutic strategies were coincident. Therefore, we should reach a consensus regarding the medical treatments of IBD on the basis of this survey.
ACKNOWLEDGEMENT
The authors would like to thank all physicians in Asia joining this wed-based survey. All authors have contributed to the creation of the questionnaire described in this article, and all authors participated in the preparation, review and approval of the manuscript content.
Notes
Financial support: This work was supported by the Japanese Society for the Promotion of Science "KAKENHI" 24590941 and supported in part by Health and Labour Sciences Research Grants for research on intractable diseases from the Ministry of Health, Labour and Welfare of Japan (Investigation and Research for Intractable Inflammatory Bowel Disease).
References
1. Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asiapacific Crohn’s and colitis epidemiology study. Gastroenterology. 2013; 145:158–165. PMID: 23583432.

2. Prideaux L, Kamm MA, De Cruz PP, Chan FK, Ng SC. Inflammatory bowel disease in Asia: a systematic review. J Gastroenterol Hepatol. 2012; 27:1266–1280. PMID: 22497584.

3. Ng SC, Tang W, Leong RW, et al. Environmental risk factors in inflammatory bowel disease: a population-based case-control study in Asia-Pacific. Gut. 2015; 64:1063–1071. PMID: 25217388.

4. Feagan BG, Macdonald JK. Oral 5-aminosalicylic acid for induction of remission in ulcerative colitis. Cochrane Database Syst Rev. 2012; 10:CD000543. PMID: 23076889.

5. Minami N, Yoshino T, Matsuura M, et al. Tacrolimus or infliximab for severe ulcerative colitis: short-term and long-term data from a retrospective observational study. BMJ Open Gastroenterol. 2015; 2:e000021.

6. Nakase H, Yoshino T, Matsuura M. Role in calcineurin inhibitors for inflammatory bowel disease in the biologics era: when and how to use. Inflamm Bowel Dis. 2014; 20:2151–2156. PMID: 25029618.

7. Timmer A, McDonald JW, Tsoulis DJ, Macdonald JK. Azathioprine and 6-mercaptopurine for maintenance of remission in ulcerative colitis. Cochrane Database Syst Rev. 2012; 9:CD000478. PMID: 22972046.

8. Hawthorne AB, Logan RF, Hawkey CJ, et al. Randomised controlled trial of azathioprine withdrawal in ulcerative colitis. BMJ. 1992; 305:20–22. PMID: 1638191.

9. Sandborn WJ. A review of immune modifier therapy for inflammatory bowel disease: azathioprine, 6-mercaptopurine, cyclosporine, and methotrexate. Am J Gastroenterol. 1996; 91:423–433. PMID: 8633486.
10. Cuffari C, Present DH, Bayless TM, Lichtenstein GR. Optimizing therapy in patients with pancolitis. Inflamm Bowel Dis. 2005; 11:937–946. PMID: 16189424.

11. Travis SP, Stange EF, Lémann M, et al. European evidencebased Consensus on the management of ulcerative colitis: current management. J Crohns Colitis. 2008; 2:24–62. PMID: 21172195.

12. Nakase H, Honzawa Y, Toyonaga T, et al. Diagnosis and treatment of ulcerative colitis with cytomegalovirus infection: importance of controlling mucosal inflammation to prevent cytomegalovirus reactivation. Intest Res. 2014; 12:5–11. PMID: 25349558.

13. Hida N, Nakamura S, Hahm KB, et al. A questionnaire-based survey on the diagnosis and management of inflammatory bowel disease in East Asian countries in 2012. Digestion. 2014; 89:88–103. PMID: 24458117.

14. Yoshino T, Nakase H, Ueno S, et al. Usefulness of quantitative real-time PCR assay for early detection of cytomegalovirus infection in patients with ulcerative colitis refractory to immunosuppressive therapies. Inflamm Bowel Dis. 2007; 13:1516–1521. PMID: 17828781.

15. Zachos M, Tondeur M, Griffiths AM. Enteral nutritional therapy for induction of remission in Crohn’s disease. Cochrane Database Syst Rev. 2007; CD000542. DOI: 10.1002/14651858.CD000542.pub2. PMID: 17253452.

16. Louis E, Michel V, Hugot JP, et al. Early development of stricturing or penetrating pattern in Crohn’s disease is influenced by disease location, number of flares, and smoking but not by NOD2/CARD15 genotype. Gut. 2003; 52:552–557. PMID: 12631668.

17. Allez M, Lemann M, Bonnet J, Cattan P, Jian R, Modigliani R. Long term outcome of patients with active Crohn’s disease exhibiting extensive and deep ulcerations at colonoscopy. Am J Gastroenterol. 2002; 97:947–953. PMID: 12003431.

18. Lakatos PL, Czegledi Z, Szamosi T, et al. Perianal disease, small bowel disease, smoking, prior steroid or early azathioprine/ biological therapy are predictors of disease behavior change in patients with Crohn’s disease. World J Gastroenterol. 2009; 15:3504–3510. PMID: 19630105.

19. Dubinsky MC. Serologic and laboratory markers in prediction of the disease course in inflammatory bowel disease. World J Gastroenterol. 2010; 16:2604–2608. PMID: 20518081.

20. Louis E, Mary JY, Vernier-Massouille G, et al. Maintenance of remission among patients with Crohn’s disease on antimetabolite therapy after infliximab therapy is stopped. Gastroenterology. 2012; 142:63–70. PMID: 21945953.

21. Brooks AJ, Sebastian S, Cross SS, et al. Outcome of elective withdrawal of anti-tumour necrosis factor-α therapy in patients with Crohn’s disease in established remission [published online ahead of print May 18, 2015]. J Crohns Colitis. DOI: 10.1016/j.crohns.2014.09.007.

22. Yanai H, Lichtenstein L, Assa A, et al. Levels of drug and antidrug antibodies are associated with outcome of interventions after loss of response to infliximab or adalimumab. Clin Gastroenterol Hepatol. 2015; 13:522–530. PMID: 25066837.

23. Guerra I, Bermejo F. Management of inflammatory bowel disease in poor responders to infliximab. Clin Exp Gastroenterol. 2014; 7:359–367. PMID: 25258548.
24. Panés J, Bouzas R, Chaparro M, et al. Systematic review: the use of ultrasonography, computed tomography and magnetic resonance imaging for the diagnosis, assessment of activity and abdominal complications of Crohn’s disease. Aliment Pharmacol Ther. 2011; 34:125–145. PMID: 21615440.

25. Ordás I, Rimola J, Rodríguez S, et al. Accuracy of magnetic resonance enterography in assessing response to therapy and mucosal healing in patients with Crohn’s disease. Gastroenterology. 2014; 146:374–382. PMID: 24177375.

26. Jones GR, Kennedy NA, Lees CW, Arnott ID, Satsangi J. Systematic review: The use of thiopurines or anti-TNF in post-operative Crohn’s disease maintenance – progress and prospects. Aliment Pharmacol Ther. 2014; 39:1253–1265. PMID: 24738574.

27. Baudry C, Pariente B, Lourenço N, et al. Tailored treatment according to early post-surgery colonoscopy reduces clinical recurrence in Crohn’s disease: a retrospective study. Dig Liver Dis. 2014; 46:887–892. PMID: 25081846.

Fig. 3
Second-line therapies in acute severe UC when intravenous steroids fail. TNF, tumor necrosis factor.
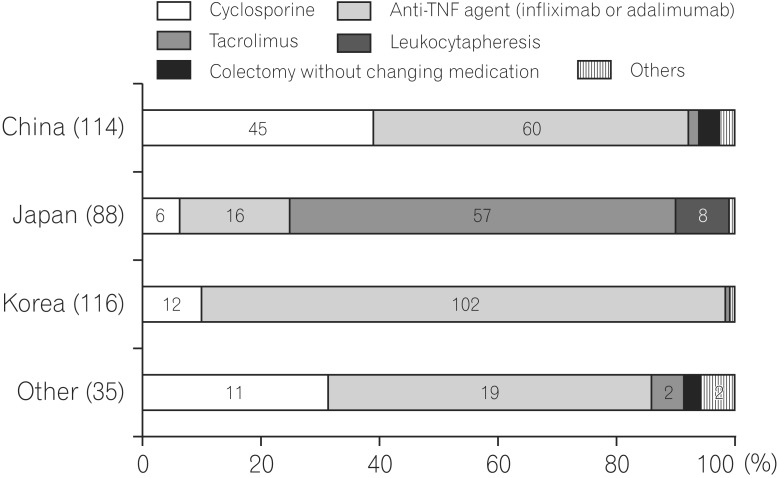
Fig. 5
Induction therapy in mild to moderate inflammatory small bowel CD. 5-ASA, 5-aminosalicylic acid.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download