Abstract
Patients with inflammatory bowel disease (IBD) have an elevated risk of venous thromboembolism compared with the general population. The most common sites of venous thromboembolism in IBD patients are the deep veins of the legs, the pulmonary system, and portal and mesenteric veins. However, cerebral venous thrombosis is rarely associated with IBD. This report describes a case of cerebral venous thrombosis in a patient with Crohn's disease. A 17-year-old girl, diagnosed 4 years earlier with Crohn's disease, presented with headache and vomiting. Magnetic resonance imaging of the brain with venography showed venous thrombosis in the cortical veins, superior sagittal sinus, right transverse sinus, and right internal jugular vein. The patient immediately started anticoagulation therapy with intravenous heparin infusion followed by daily oral rivaroxaban 10 mg. Follow-up imaging after 2 weeks showed resolution of the thrombosis, with recanalization of the cortical veins, superior sagittal sinus, right transverse sinus, and right internal jugular vein. She continued rivaroxaban therapy for 6 months, and remained well, without neurologic sequelae. A high level of concern for cerebral venous thrombosis may be important when treating active IBD patients, because anticoagulation treatment can prevent fatal complications.
Patients with IBD have a higher risk of venous thrombosis compared with the general population.1 The most common sites of venous thrombosis in IBD patients are the deep veins of the legs, pulmonary system, and portal and mesenteric veins.2 However, cerebral venous thrombosis is rarely associated with IBD, and is more likely to occur as a complication of UC than of CD.3 Cerebral venous thrombosis in patients with CD has been reported only rarely.45 Furthermore, there have been no case reports of cerebral venous thrombosis occurring during a flare up of CD, in Korea.We describe a case of cerebral venous thrombosis as a complication of active CD during flare up. We have also reviewed the English-language literature on this topic.
A 17-year-old girl was hospitalized with abdominal pain that had persisted for 2 weeks. She had been diagnosed 4 years earlier with CD and subsequently treated at our gastroenterology clinic. Her CD exhibited non-stricturing, non-penetrating behavior, with ileocolonic location and stomach involvement. She was treated with azathioprine (Azathioprine® PCH; Pharmachemie BV, Haarlem, The Netherlands) and mesalazine (Pentasa® SR; Ferring, Saint-Prex, Switzerland). She had recently maintained disease remission with a regimen of azathioprine 100 mg, after discontinuing mesalazine because of neutropenia.
Upon admission, she complained of severe, throbbing headache and vomiting. Her headache had developed 1 week earlier, with no previous attacks. The headache was located in the right and left temporal regions, and could not be controlled with simple analgesics. She did not complain of other symptoms that might suggest infection, such as fever or chills. Her vital signs were stable, with a blood pressure of 115/66 mmHg, pulse rate of 62 beats per minute, respiratory rate of 20 breaths per minute, and body temperature of 36.3℃. She was alert and did not demonstrate neurologic symptoms, although she appeared to be acutely ill. Her white blood cell count was 3,500/mm3, her hemoglobin level was 10.2 g/dL, and her platelet count was 327,000/mm3. All other tests, including biochemical tests, electrolyte tests, coagulation tests, and autoantibodies (including perinuclear antineutrophil cytoplasmic antibodies, cytoplasmic antineutrophil cytoplasmic antibodies, lupus anticoagulants, anti-double strand deoxyribonucleic acid, antiphospholipid antibodies, anticardiolipin antibodies, and anticyclic citrullinated peptides), were within normal limits, except for an elevated CRP level of 21.6 mg/dL. Her CDAI score was 244.
We could not perform colonoscopy or three-dimensional CT of the small bowel for workup of what appeared to be aggravated CD, because the patient was unable to drink fluids. Upper endoscopy revealed multiple erosions in the esophagus and stomach, and microscopic examination of biopsy specimens found suspicious granuloma, suggesting upper gastrointestinal involvement of CD. In a limited colonoscopic examination performed after administration of an enema, longitudinal ulcers and a cobble stone appearance with skipped patterns were observed from the terminal ileum to the proximal transverse colon (Fig. 1). These findings had worsened since the patient's previous colonoscopy, performed 1 year earlier. We initiated treatment with a biologic agent because her condition was declining despite administration of immune-modulating agents, and because of prognostic factors associated with poor outcomes, including her young onset of disease and involvement of the upper gastrointestinal tract. Infliximab (Remsima®; Celltrion, Incheon, Korea) 5 mg/kg was selected because she suffered from mental retardation and would find it difficult to self-inject medication. After treatment began, the inflammatory activity was rapidly controlled, as indicated by a decreased CDAI score of 96.
After consultation with neurologists, a cerebrospinal fluid analysis was performed to rule out the possibility of encephalomeningitis. Although testing revealed an elevated intracranial pressure of 220 mmH2O, no white blood cells or red blood cells were detected. Additionally, her protein level was 15.0 mg/dL and her glucose level was 74 mg/dL, further minimizing the likelihood of encephalomeningitis. Therefore, a CT of the brain was performed to rule out other causes of headache and to find the cause of the elevated intracranial pressure. This revealed hyper-attenuations at the anterior and medial superior sagittal sinus, right transverse sinus, and cortical veins, and thus suggested a diagnosis of cerebral venous thrombosis (Fig. 2). The patient then underwent MRI of the brain with venography, resulting in detection of venous thrombosis in the cortical veins, superior sagittal sinus, right transverse sinus, and right internal jugular vein (Fig. 3). Blood tests for homocysteine, factor V, VIII, IX, XI, and vWF antigen were also performed to rule out thrombophilic conditions, and the results were normal. However, her levels of antithrombin III (126%), protein C activity (159%), and protein S activity (131%) were all high. Her D-dimer level (1.4 mg/mL) was also slightly elevated, as may occur during exacerbation of CD.
The patient was diagnosed with cerebral venous thrombosis as a complication of CD flare-up, without underlying thrombophilic conditions. She was treated with intravenous heparin (Heparin® 25,000 IU/5mL; JW pharmaceutical, Seoul, Republic of Korea). A follow-up CT scan performed after 7 days of anticoagulation showed resolution of the dense attenuation within the superior sagittal sinus and right transverse sinus (Fig. 4). Her headache and vomiting improved after 9 days of treatment, and completely disappeared after 14 days. An MRI with venography was conducted after 2 weeks of anticoagulation and showed resolution of the venous thrombosis with recanalization of the cortical veins, superior sagittal sinus, and right transverse sinus (Fig. 5).
The patient was discharged on a regimen of rivaroxaban (Xarelto®; Bayer HealthCare AG, Leverkusen, Germany) 10 mg daily, with treatment continued for 6 months. She remained stable, without neurological damage.
IBD can be complicated by a variety of extra-intestinal conditions, including venous thrombosis due to hypercoagulability. In Korea, a few cases of thrombotic complications in patients with CD have been reported (Table 1).56789 In cases of venous thrombosis, cerebral vascular involvement is very rarely observed.45 Cerebral venous thrombosis can be accompanied by neurologic abnormalities caused by rapidly elevating intracranial pressure, and can result in serious adverse events. Therefore, early differential diagnosis of this rare complication is important for CD patients complaining of headache and vomiting. In a study that retrospectively analyzed data from 65 case reports of IBD patients with cerebral venous thrombosis, the average patient age was 29, and women experienced complications more frequently than men (37 vs. 28).3 The incidence of UC was almost double compared with CD (42 vs. 21), and active disease was reported in 78.4% of the cases. The predominant neurological symptoms were headache (80%), seizure (35%), vomiting (29%), hemiplegia or tetraplegia (29%), altered consciousness (21%), vision deficits (12%), and papilledema (7%). The most common site of cerebral venous thrombosis was the superior sagittal sinus (50.7%), and thrombosis in multiple sites occurred in about 50% of cases, like the one we have reported here. The main risk factors for hypercoagulability were anemia (49%) and thrombocytosis (26%); however, there were many cases (23%) accompanied by coagulation abnormalities of fibrinogen, elevated factor VII, elevated factor VIII, protein C deficiency, and protein S deficiency. In our case, cerebral venous thrombosis complicated during flareup of CD, without underlying thrombophilic conditions.
In Korea, only one case has previously documented cerebral venous thrombosis as a complication of CD.5 In that case, a 45-year-old man presented with headaches and was diagnosed with cerebral venous thrombosis as a complication of CD, based on CT and MRI findings. He was treated with heparin and warfarin. However, that patient's CD was stable and not in an active phase, in contrast to our case. In addition, his thrombophilic condition was not fully examined by factor V, VIII, IX, XI, and vWF antigen testing. Therefore, our case report is the first to describe cerebral venous thrombosis during flare-up of CD, without the presence of underlying thrombophilic conditions, in Korea.
Patients with IBD who develop thrombosis often have active disease at the time of thromboembolism.101112 Grainge et al.10 analyzed 13,756 patients with IBD and 71,672 matched controls, and found that 139 patients and 165 controls developed venous thromboembolism. Overall, patients with IBD had a 3.4 times higher risk of developing venous thromboembolism than did controls, with risk increasing up to 8.4 times during a flare-up of IBD. Currently, there is no clear evidence based on randomized controlled trials indicating whether anticoagulation treatment should be used as a preventive measure for patients with IBD. However, anticoagulation therapy for hospitalized patients with active IBD has been associated with lower incidence of venous thrombosis and mortality.1112 Few international guidelines recommended preventive use of anticoagulant therapy for hospitalized patients with active IBD,11 and the Korean IBD treatment guidelines have not addressed this issue.1314
In patients with IBD complicated by cerebral venous thrombosis, favorable outcomes are possible with early diagnosis and appropriate treatment. However, when patients are not treated, the mortality rate can be as high as 50%.3 Therefore, physicians should be especially careful to consider the possibility of cerebral venous thrombosis in patients with IBD, especially when there is active disease, as in our case. Treatment of cerebral venous thrombosis must continue for at least 3 months, but if there are risk factors for thrombosis, coagulation abnormalities, or thrombogenic mutation, then long term treatment of more than 6 months should be maintained.15 Since the underlying IBD can be a cause of thrombosis, treatment of the inflammation itself is essential.11 In our case, the patient's inflammatory activity of CD was rapidly controlled with a biologic agent, and anticoagulation with intravenous heparin reversed her thrombophilic conditions.
Although this is the second case reported in Korea of CD complicated by cerebral venous thrombosis, this is the first case in active CD without underlying thrombophilic conditions. Once again, a high level of concern for cerebral venous thrombosis is important when treating active IBD patients, because anticoagulation may prevent fatal complications.
References
1. Bernstein CN, Blanchard JF, Houston DS, Wajda A. The incidence of deep venous thrombosis and pulmonary embolism among patients with inflammatory bowel disease: a population-based cohort study. Thromb Haemost. 2001; 85:430–434. PMID: 11307809.
2. Talbot RW, Heppell J, Dozois RR, Beart RW Jr. Vascular complications of inflammatory bowel disease. Mayo Clin Proc. 1986; 61:140–145. PMID: 3080643.
3. Katsanos AH, Katsanos KH, Kosmidou M, Giannopoulos S, Kyritsis AP, Tsianos EV. Cerebral sinus venous thrombosis in inflammatory bowel diseases. QJM. 2013; 106:401–413. PMID: 23243293.
4. Kwon Y, Koene RJ, Cho Y. A case of cerebral venous sinus thrombosis associated with Crohn's disease: dilemma in management. Gastroenterol Rep (Oxf). [published online ahead of print November 10, 2014]. DOI: 10.1093/gastro/gou079.
5. Huh SY, Kim JK, Park SJ. Cerebral venous sinus thrombosis in a patient with Crohn disease. Kosin Med J. 2009; 24:190–192.
6. Chung C, Kang DH, Kim EA, et al. A case of pulmonary embolism in recurrent ileal Crohn's disease after total colectomy. Korean J Gastrointest Endosc. 2001; 22:111–115.
7. Chung ES, Kim JH, Jung JH, et al. A case of pulmonary thromboembolism in Crohn's disease. Tuberc Respir Dis. 2009; 66:370–373.
8. Kim W, Kang B, Kim BW, et al. Crohn's disease initially accompanied by deep vein thrombosis and ulnar neuropathy without metronidazole exposure. Gut Liver. 2013; 7:252–254. PMID: 23560164.
9. Oh DY, Jung HK, Kwon KJ, et al. Unusual complication of Crohn's disease: portal hypertension related with rapid progression of portal vein and superior mesenteric vein thrombosis. Korean J Med. 2013; 84:713–717.
10. Grainge MJ, West J, Card TR. Venous thromboembolism during active disease and remission in inflammatory bowel disease: a cohort study. Lancet. 2010; 375:657–663. PMID: 20149425.
11. Papa A, Gerardi V, Marzo M, Felice C, Rapaccini GL, Gasbarrini A. Venous thromboembolism in patients with inflammatory bowel disease: focus on prevention and treatment. World J Gastroenterol. 2014; 20:3173–3179. PMID: 24695669.
12. Zezos P, Kouklakis G, Saibil F. Inflammatory bowel disease and thromboembolism. World J Gastroenterol. 2014; 20:13863–13878. PMID: 25320522.
13. Ye BD, Yang SK, Shin SJ, et al. Guidelines for the management of Crohn's disease. Korean J Gastroenterol. 2012; 59:141–179. PMID: 22387837.
14. Choi CH, Kim YH, Kim YS, et al. Guidelines for the management of ulcerative colitis. Korean J Gastroenterol. 2012; 59:118–140. PMID: 22387836.
15. Einhäupl K, Stam J, Bousser MG, et al. EFNS guideline on the treatment of cerebral venous and sinus thrombosis in adult patients. Eur J Neurol. 2010; 17:1229–1235. PMID: 20402748.
Fig. 1
Endoscopic findings. Endoscopic findings show the longitudinal ulcers (A) A B with cobble stone appearance (B).
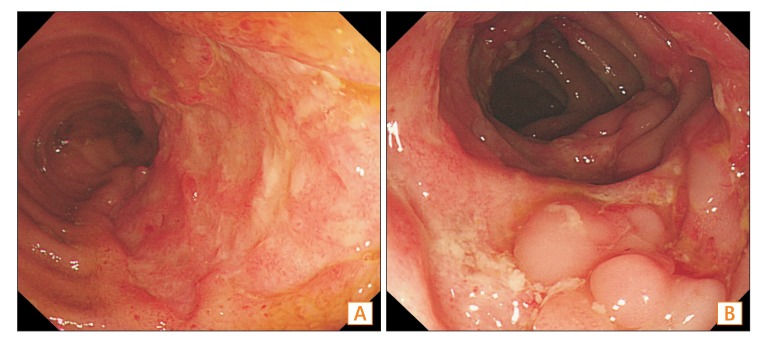
Fig. 2
Brain CT findings. The CT shows hyperattenuation segments at the anterior and medial superior sagittal sinus (A), right transverse sinus (B, arrow), and cortical veins (B, arrowhead).
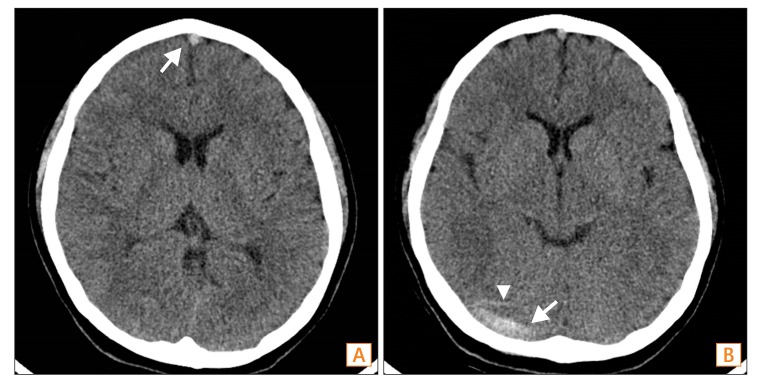
Fig. 3
Brain MRI with venography. Magnetic resonance venography shows venous thrombosis in the cortical veins (B, thin arrow), superior sagittal sinus (A, arrowheads), right transverse sinus (B, arrow), and right internal jugular vein (B, arrowhead).
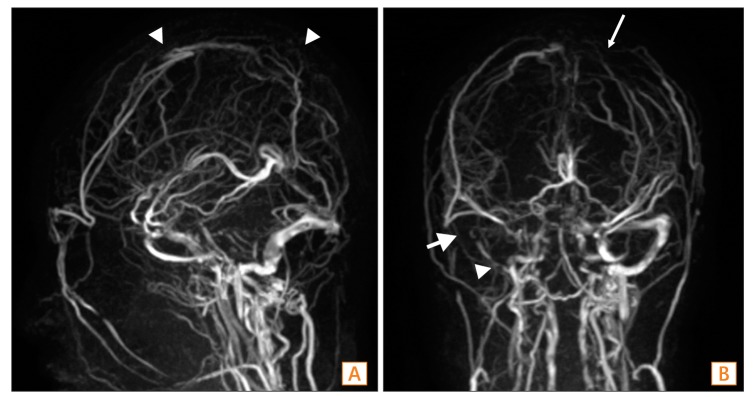
Fig. 4
Follow-up brain CT after 7 days of anticoagulation. Follow up CT shows resolution of dense attenuation within the superior sagittal sinus (A), right transverse sinus (B, arrow), and cortical veins (B, arrowhead).
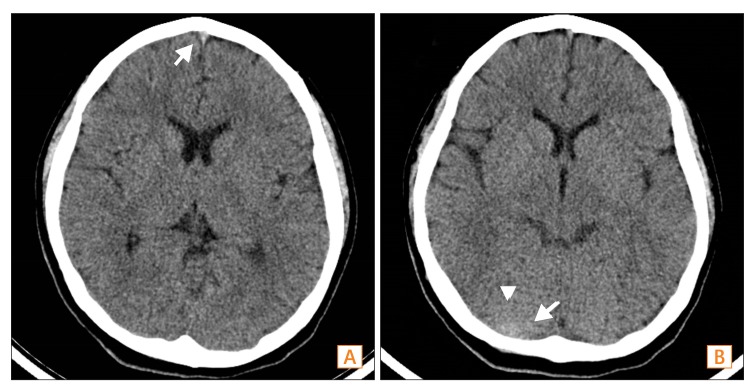
Fig. 5
Follow-up brain MRI with venography after 2 weeks of anticoagulation. Follow up MRI with venography shows resolved venous thrombosis with recanalization of the cortical veins (B, thin arrow), superior sagittal sinus (A, arrowheads), right transverse sinus (B, arrow), and right internal jugular vein (B, arrowhead).
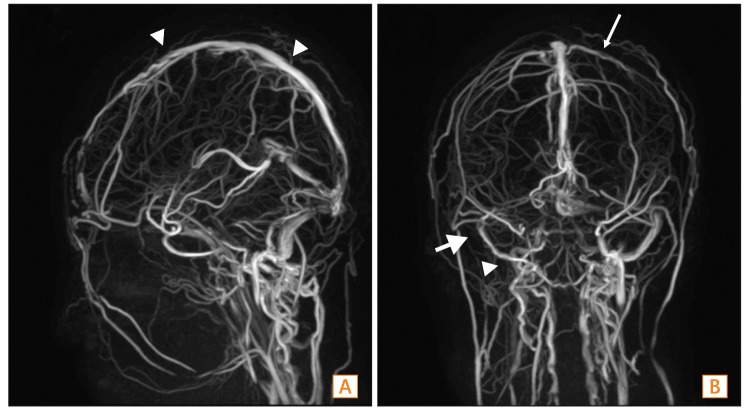
Table 1
Thrombotic Complications in Patients With CD in Korea
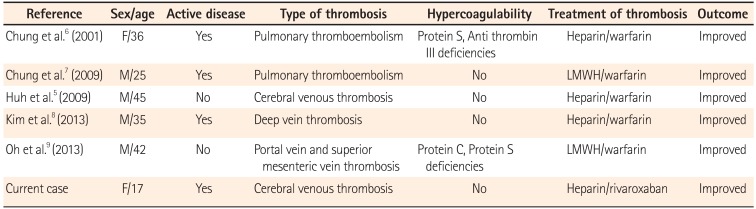
| Reference | Sex/age | Active disease | Type of thrombosis | Hypercoagulability | Treatment of thrombosis | Outcome |
|---|---|---|---|---|---|---|
| Chung et al.6 (2001) | F/36 | Yes | Pulmonary thromboembolism | Protein S, Anti thrombin III deficiencies | Heparin/warfarin | Improved |
| Chung et al.7 (2009) | M/25 | Yes | Pulmonary thromboembolism | No | LMWH/warfarin | Improved |
| Huh et al.5 (2009) | M/45 | No | Cerebral venous thrombosis | No | Heparin/warfarin | Improved |
| Kim et al.8 (2013) | M/35 | Yes | Deep vein thrombosis | No | Heparin/warfarin | Improved |
| Oh et al.9 (2013) | M/42 | No | Portal vein and superior mesenteric vein thrombosis | Protein C, Protein S deficiencies | LMWH/warfarin | Improved |
| Current case | F/17 | Yes | Cerebral venous thrombosis | No | Heparin/rivaroxaban | Improved |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download