Abstract
Screening for colorectal cancer (CRC) using sigmoidoscopy or colonoscopy is now common in many developed countries. This concise, evidence-based review looks at the impact of sigmoidoscopy or colonoscopy screening on CRC incidence, CRC mortality and overall mortality. Data from controlled retrospective and prospective (observational or randomized) studies have generally shown that sigmoidoscopy and colonoscopy, whether for diagnostic, screening or surveillance purposes, are associated with a significant reduction in CRC incidence and CRC mortality. The data on their impact on overall mortality is much more limited, with most studies unable to report a reduction in overall mortality. The results of three meta-analyses have confirmed these conclusions. As expected, sigmoidoscopy has a predominant effect on left-sided CRC, although some studies have shown modest effects on right-sided colon cancer as well. Most studies on colonoscopy have demonstrated that the protective effect applies to both right and left-sided cancer, although the protection seemed better on the left side. Despite the introduction of other screening and diagnostic modalities for the colon, such as computed tomography colonography and colonic capsule endoscopy, lower endoscopy will continue to be an important mode of screening for CRC and evaluating the colon.
Screening for colorectal cancer (CRC) in average-risk or high-risk patients has become the standard of care in most developed countries. Such screening can be accomplished by various modalities, including fecal occult blood testing, fecal DNA testing, CT colonography and colonic capsule endoscopy, but in many countries, particularly the United States, the dominant screening methods are endoscopy (i.e., flexible sigmoidoscopy and colonoscopy). This evidence-based review looks at the impact of sigmoidoscopy and colonoscopy on CRC incidence, CRC mortality and overall mortality. Because the purpose is to look at the effect of sigmoidoscopy and colonoscopy on the general population, studies that focus only on patients who underwent polypectomy were not included.
Flexible sigmoidoscopy has long been used for CRC screening, and continues to be popular in many countries. It has the advantages of being more widely available (it can be competently performed by appropriately trained primary care providers, surgeons, or even non-physician providers), quicker (the procedure time is shorter and there is often no need for sedation), more convenient (no need for whole colon bowel preparation) and less expensive than colonoscopy. If an adenoma is discovered on sigmoidoscopy, then typically full colonoscopy is recommended because of the increased risk of a synchronous colonic neoplasm. Removal of large polyps with cautery snare polypectomy cannot be performed because of the risk of explosion since these patients have not undergone a full bowel preparation. Despite its undoubted efficacy, cross-sectional studies have shown that sigmoidoscopy may miss a substantial portion of right-sided colonic neoplasia in patients without concurrent left-sided neoplasia.1,2
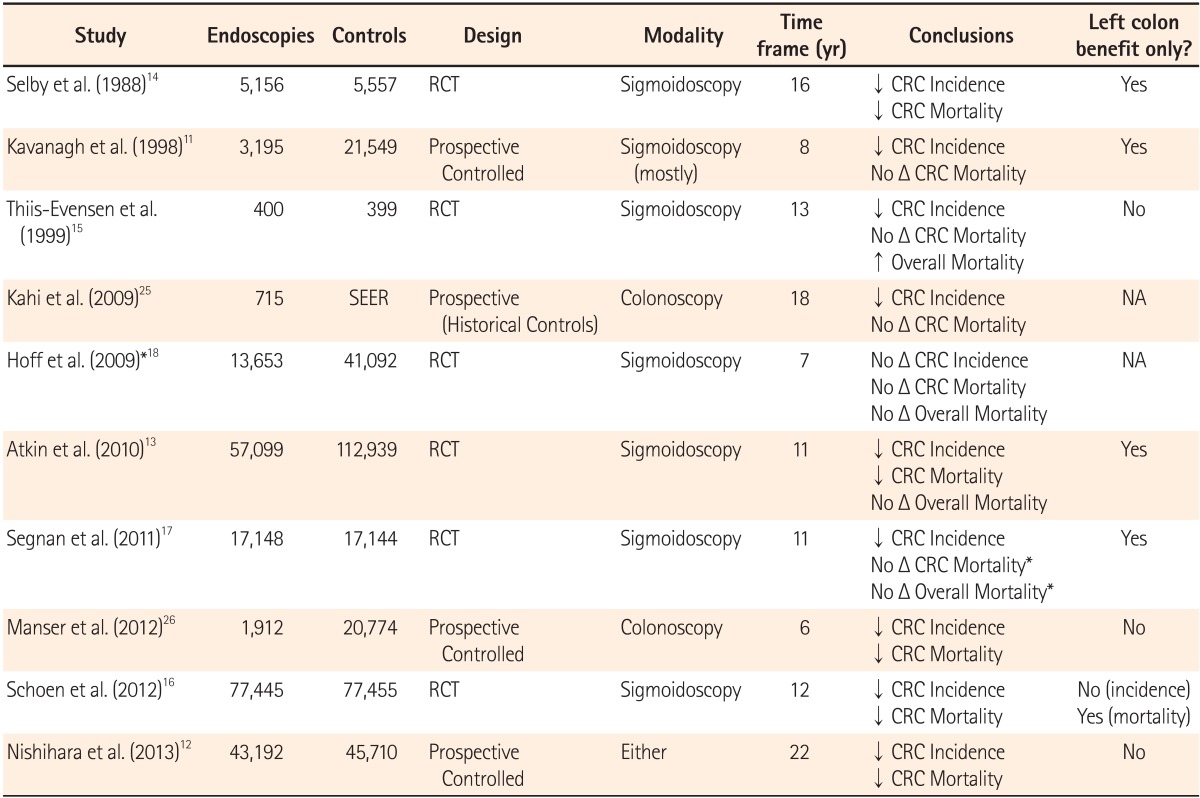
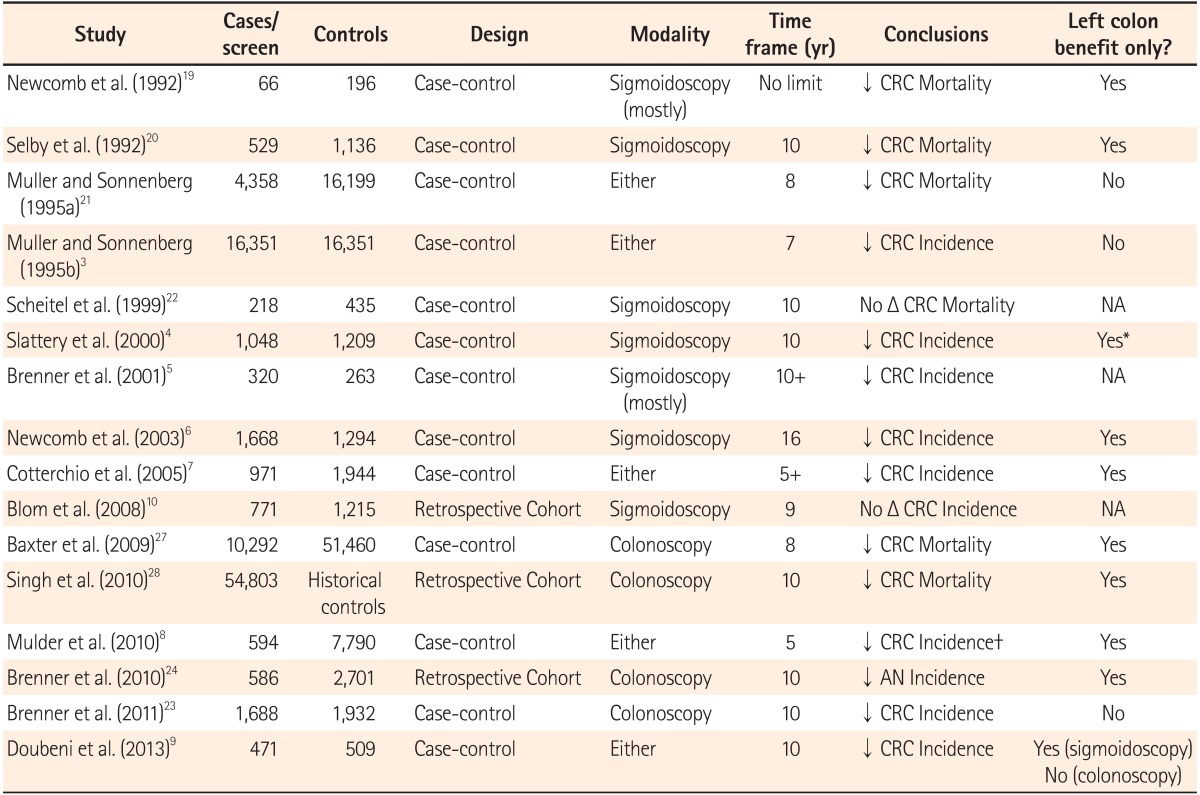
There is a substantial body of literature looking at the impact of sigmoidoscopy on CRC incidence (Tables 1 and 2). The earliest evidence was provided by an American retrospective case-control study,3 and subsequently there have been a series of other case-control studies from various countries confirming that sigmoidoscopy is associated with a reduction in CRC incidence.4,5,6,7,8 Case-control studies typically present their findings as OR, which closely approximate risk ratios in low-prevalence conditions or outcomes; thus, an OR of <1.0 implies a protective effect of the "exposure", in this case sigmoidoscopy, against an undesired outcome, for the purposes of this review either CRC development or mortality.
In one of the earliest studies on this topic, 16,351 U.S. Veterans Administration Health Care System patients with CRC were compared against age- and sex-matched controls.3 The OR for exposure to previous sigmoidoscopy was 0.56 [0.46-0.67] for colon cancer and 0.61 [0.49-0.75] for rectal cancer occurrence. This was followed by a population-based case-control study involving 1,048 subjects with colon cancer (rectal cancers were excluded), with an OR of 0.56 [0.44-0.77] for men and 0.53 [0.33-0.77] for women.4 A case-control study from Germany then showed an OR of 0.28 [0.16-0.48] for lower endoscopy (mostly sigmoidoscopy), with the protective effect extending for >10 years.5 Another population-based case-control study on 1,668 patients with CRC against 1,294 controls reported an OR of 0.24 [0.17-0.33]; this study also showed a protective effect extending for as long as 16 years.6 These results were echoed by a Canadian case-control study with 971 cases and 1,944 controls from the Ontario Cancer Registry, the OR being 0.59 [0.46-0.76].7 Finally, a recent American case-control study with 471 cases and 509 controls showed an OR of 0.50 [0.36-0.70] for sigmoidoscopy exposure.9 Against all this evidence, the only contradicting data come from two Dutch studies, one a retrospective cohort and the other a case-control study, both of which found only non-significant trends towards reduction in CRC incidence with sigmoidoscopy.8,10
Prospective non-randomized controlled studies have also shown that sigmoidoscopy is associated with reduction in CRC incidence.11,12 An earlier study on 24,744 men from a long-term prospective observational study, the Health Professionals Follow-up Study, showed a relative risk for CRC of 0.58 [0.36-0.96] after a follow-up of 8 years after lower endoscopy (mostly sigmoidoscopy).11 More recently, a better designed study utilizing 22-year data from the Nurses Health Study, with 57,166 female subjects, as well as the Health Professionals Follow-up Study, with 31,736 male subjects, demonstrated convincingly that CRC incidence reduction was linked to screening sigmoidoscopy, with a relative risk of 0.60 [0.53-0.68] after negative sigmoidoscopy.12
Randomized controlled trials provide the most important data on sigmoidoscopy and CRC incidence.13,14,15,16,17 The pivotal studies are the United Kingdom Flexible Sigmoidoscopy Trial, which showed a reduction in CRC incidence of 23% amongst 57,237 subjects in the screening group,13 the Italian 'Screening for COlon and REctum (SCORE)' study, which showed a reduction of 18% amongst 17,148 subjects randomized to screening sigmoidoscopy,17 and the U.S. Prostate, Lung and Colorectal Cancer (PLCO) Trial, which showed an incidence reduction of 21% amongst 77,445 screening subjects.16 Prior to this, there were three less conclusive randomized trials that also looked at the effectiveness of sigmoidoscopy in preventing CRC.14,15,18 In the Kaiser Permanente Multi-phasic Evaluation Study, even though the incidence of CRC in the study group (who underwent screening with various modalities) was lower than in the controls (4.3 versus 6.7 cases per persons), a retrospective analysis of the trial data did not show any significant difference in exposure to sigmoidoscopy.14 In the small Telemark Polyp Study from Norway, which randomized 799 individuals, the relative risk was 0.2 [0.03-0.95].15 Finally, the Norwegian Colorectal Cancer Prevention (NORCCAP) trial, a much larger, 7-year trial also from Norway (with 55,736 participants, half of whom were screened with one-time sigmoidoscopy) reported a non-significant relative risk of 0.73 [0.47-1.13].18 It is generally believed that the negative results of the NORCCAP trial were due to excessively short follow-up time.
As expected, most of the studies found that sigmoidoscopy had a protective effect for left-sided CRCs only;6,7,9,11,13,17 in some studies, there were trends towards small protective effects for right-sided colon cancer, but these rarely reached statistical significance, except in the largest studies.12,16 One study that excluded rectal cancers still showed only left-sided benefit when comparing proximal against distal colon cancers.4
Not only does sigmoidoscopy reduce the incidence of CRC, but there is now convincing evidence that sigmoidoscopy reduces CRC-specific mortality as well (Tables 1 and 2). However, data on its impact on overall or all-cause mortality are limited and do not demonstrate a benefit at this time.
The earliest evidence of the effect of sigmoidoscopy on CRC mortality came from retrospective case-control studies.19,20,21 Early on, a small case-control study, with only 66 cases and 196 controls, reported an OR of 0.21 [0.08-0.52], suggesting a strong protective effect of sigmoidoscopy against CRC mortality.19 This was followed by a larger case-control study, this time with 261 cases and 868 controls from the Kaiser Permanente Health System, confirming mortality reduction with an adjusted OR of 0.41 [0.25-0.69].20 A few years later, an even larger Veterans Administration Health Care study involving 4,411 patients who died from CRC (each matched to four controls) showed an OR of 0.66 [0.54-0.82].21 The only exception has been a small case-control with 653 subjects which failed to show any reduction in CRC mortality.22
Two previously described prospective non-randomized controlled studies also looked at CRC mortality.11,12 The earlier study, based on male subjects from the Health Professionals Follow-up Study, found an age-adjusted relative risk of 0.56 [0.20-1.60], denoting a trend towards a protective effect of sigmoidoscopy against CRC death.11 More recent analysis of 22 year follow-up data from both the Nurses Health Study and Health Professionals Follow-up Study demonstrated a relative risk of 0.59 [0.45-0.76], confirming this protective effect.12
Similar to the situation with CRC incidence, randomized controlled trials provide the most important data on the efficacy of sigmoidoscopy in reducing CRC mortality.13,14,16,17 The results of the initial studies were somewhat ambivalent. The Kaiser Permanente Multi-phasic Study showed lower CRC mortality in the group randomized to screening, but retrospective analysis of screening exposure showed that patients in the screening group were not more likely to have undergone sigmoidoscopy.14 In contrast, by intention-to-treat analysis, the Italian SCORE Trial showed a reduction of 22% for CRC mortality, which did not reach statistical significance, but per protocol analysis resulted in a significant 38% reduction.17 Other early randomized studies were not able to demonstrate beneficial effects of sigmoidoscopy on CRC mortality.15,18 In the last few years, more conclusive data became available from the United Kingdom Flexible Sigmoidoscopy Trial, which showed a significant reduction in CRC mortality of 31%,13 while the American PLCO Trial showed a reduction of 26%.16
With regard to overall mortality, the data to date have been less encouraging. None of the available randomized controlled trials were able to demonstrate any improvement in overall mortality,13,14,16,17,18 and one even reported increased overall mortality in those who underwent sigmoidoscopy.15 The reason for this lack of benefit is unclear, but may be due to occasional complications from the sigmoidoscopies or the associated follow-up colonoscopies, or from non-gastrointestinal comorbid conditions in the screened patients that diluted the protective effect of sigmoidoscopy.
Just like with CRC incidence, the impact of sigmoidoscopy is expected to be much more pronounced for left-sided CRC mortality than right-sided mortality, and indeed most studies found mortality protection only from left-sided CRCs,4,8,13,14,16,17,19,20 although there were a few notable exceptions.12,21
The use of colonoscopy for screening purposes has only become popular in the last 15 years or so in a few relatively affluent countries, the principal one being the United States, which is responsible for the majority of the world's colonoscopies. Nevertheless, evidence for its efficacy at reducing CRC incidence and mortality is steadily accumulating, although randomized controlled data are still limited. Colonoscopy has several advantages over sigmoidoscopy: it evaluates both the left and right colon, and, since patients have undergone a full bowel preparation, large polyps can be removed at the time of screening using cautery snare polypectomy or even argon plasma coagulation, if needed. Furthermore, colonoscopy is usually performed by gastrointestinal specialists, with a higher level of expertise than generalists.
There is mounting evidence that colonoscopy leads to a subsequent reduction in CRC incidence (Tables 1 and 2). Retrospective case-control studies provided the initial data.3,7,8,9,23 Five studies from various countries, previously described, included patients who had been exposed to either sigmoidoscopy or colonoscopy, but if we stratify the data it is clear that colonoscopy is associated with decreased incidence of CRC, with an OR of 0.47 [0.37-0.58] (for colon cancer) and 0.61 [0.48-0.77] (rectal cancer) in the Veterans Administration Health System study,3 0.29 [0.15-0.58] in another American study,9 0.70 [0.57-0.87] in a Canadian study,7 0.23 [0.19-0.27] in a German study,23 and 0.45 [0.20-0.98] in a Dutch study.8 In addition, a German retrospective cohort study with 586 screened patients and 2,701 controls found a relative risk of 0.52 [0.37-0.73] for advanced neoplasia incidence.24
More recently, large prospective non-randomized controlled studies have also shown reduction in CRC incidence, with a relative risk of 0.44 [0.38-0.52] (after negative colonoscopy) reported from the Nurses Health Study and Health Professionals Follow-up Study.12 A single-cohort prospective observational study on 715 subjects supported these findings by showing a 67% reduction in CRC incidence when compared to historical controls (from the Surveillance, Epidemiology, and End Results database),25 while a prospective controlled study that followed 22,686 subjects for 6 years also reported decreased CRC incidence with an adjusted OR of 0.31 [0.16-0.59].26 Currently, there are no randomized controlled data on the impact of colonoscopy on CRC incidence, although there are some ongoing trials (e.g., the Nordic-European Initiative on Colorectal Cancer [NordICC] trial, comparing screening colonoscopy versus no screening; and the CONFIRM trial, comparing screening colonoscopy versus fecal occult blood testing) that may provide some findings in the near future.
There is now reasonably robust evidence from several sources that exposure to colonoscopy, whether screening or diagnostic, is associated with a reduction in CRC mortality (Tables 1 and 2). Similar to the research on CRC incidence, retrospective studies account for most of the evidence in this area.21,27,28
Earlier on, a before-mentioned Veterans Administration Health Care System study that included patients who had undergone sigmoidoscopy or colonoscopy showed a protective effect for colonoscopy once the data were stratified (OR 0.43 [0.30-0.63]).21 Subsequently, two large studies using administrative data from the Canadian national health insurance system reported an association between colonoscopy and decreased CRC mortality, with an OR of 0.69 [0.63-0.74] for the Ontario case-control study (with 10,292 cases and 51,460 controls),27 and a risk reduction of 29% for the Manitoba retrospective cohort study (with a total of 54,803 subjects compared against historical controls).28 In the same vein, a retrospective analysis on 1,071 CRC patients not only showed improved survival in those whose cancers were detected by screening as opposed to symptoms, but also a "stage-shift" as well, i.e., higher probability of cancers being detected at an earlier stage.29
With regard to prospective data, the main evidence comes again from the Nurses Health Study and Health Professionals Follow-up Study, which found a 68% reduction in CRC mortality for patients who had undergone screening colonoscopy.12 Another prospective cohort study, previously described, supported this with an OR of 0.12 [0.01-0.93] for CRC mortality.26 There are currently no randomized controlled data on the effect of colonoscopy on CRC mortality.
In conclusion, lower endoscopy is an effective and widely used modality for evaluating the colon and for CRC screening. Studies have generally shown that sigmoidoscopy and colonoscopy, whether for diagnostic, screening or surveillance purposes, is associated with a reduction in CRC incidence and CRC mortality. The data regarding their impact on overall mortality is much more limited at this time. No major study has been able to show a significant reduction in overall mortality from either sigmoidoscopy or colonoscopy. This may be partly explained by the phenomena of non-adherence ("screening" subjects who did not actually undergo lower endoscopy) and contamination ("controls" who actually underwent lower endoscopy as part of routine clinical care), both of which result in underestimation of the effects of lower endoscopy. As expected, sigmoidoscopy has a predominant effect on left-sided CRC, although some studies have shown modest effects on right-sided colon cancer as well, presumably due to discovery of proximal colon cancers associated with synchronous distal polyps. The added value of colonoscopy over sigmoidoscopy has been the subject of some controversy. Some earlier retrospective studies have suggested that the protective effect of colonoscopy on right-sided colon cancers is minimal or non-existent, possibly due to suboptimal bowel preparation and the tendency of flat sessile serrated adenomas to occur in the right colon. However, these studies, though boasting large sample sizes, were based exclusively on claims data and potentially subject to bias;27,28 for example, colonoscopy completion rates might be over-reported during billing to ensure payment for a complete examination even when the cecum or right colon has not been comprehensively examined. Subsequent retrospective and prospective studies have demonstrated that the protective effect applies to both right and left-sided cancer, although usually the protection was better on the left side. Despite the introduction of other screening and diagnostic modalities, such as CT colonography and colonic capsule endoscopy, lower endoscopy will continue to be an important method for CRC screening and colon evaluation. Efforts should continue to be made for improving access and examination quality, with particular focus on enhancing bowel preparation and withdrawal technique.
References
1. Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff DF. Risk of advanced proximal neoplasms in asymptomatic adults according to the distal colorectal findings. N Engl J Med. 2000; 343:169–174. PMID: 10900275.

2. Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N Engl J Med. 2000; 343:162–168. PMID: 10900274.

3. Muller AD, Sonnenberg A. Prevention of colorectal cancer by flexible endoscopy and polypectomy. A case-control study of 32,702 veterans. Ann Intern Med. 1995; 123:904–910. PMID: 7486484.

4. Slattery ML, Edwards SL, Ma KN, Friedman GD. Colon cancer screening, lifestyle, and risk of colon cancer. Cancer Causes Control. 2000; 11:555–563. PMID: 10880038.
5. Brenner H, Arndt V, Sturmer T, Stegmaier C, Ziegler H, Dhom G. Long-lasting reduction of risk of colorectal cancer following screening endoscopy. Br J Cancer. 2001; 85:972–976. PMID: 11592768.

6. Newcomb PA, Storer BE, Morimoto LM, Templeton A, Potter JD. Long-term efficacy of sigmoidoscopy in the reduction of colorectal cancer incidence. J Natl Cancer Inst. 2003; 95:622–625. PMID: 12697855.

7. Cotterchio M, Manno M, Klar N, McLaughlin J, Gallinger S. Colorectal screening is associated with reduced colorectal cancer risk: a case-control study within the population-based Ontario Familial Colorectal Cancer Registry. Cancer Causes Control. 2005; 16:865–875. PMID: 16132797.

8. Mulder SA, van Soest EM, Dieleman JP, et al. Exposure to colorectal examinations before a colorectal cancer diagnosis: a case-control study. Eur J Gastroenterol Hepatol. 2010; 22:437–443. PMID: 19952765.

9. Doubeni CA, Weinmann S, Adams K, et al. Screening colonoscopy and risk for incident late-stage colorectal cancer diagnosis in average-risk adults: a nested case-control study. Ann Intern Med. 2013; 158:312–320. PMID: 23460054.

10. Blom J, Yin L, Liden A, et al. A 9-year follow-up study of participants and nonparticipants in sigmoidoscopy screening: importance of self-selection. Cancer Epidemiol Biomarkers Prev. 2008; 17:1163–1168. PMID: 18483338.

11. Kavanagh AM, Giovannucci EL, Fuchs CS, Colditz GA. Screening endoscopy and risk of colorectal cancer in United States men. Cancer Causes Control. 1998; 9:455–462. PMID: 9794179.
12. Nishihara R, Wu K, Lochhead P, et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013; 369:1095–1105. PMID: 24047059.

13. Atkin WS, Edwards R, Kralj-Hans I, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010; 375:1624–1633. PMID: 20430429.

14. Selby JV, Friedman GD, Collen MF. Sigmoidoscopy and mortality from colorectal cancer: the Kaiser Permanente Multiphasic Evaluation Study. J Clin Epidemiol. 1988; 41:427–434. PMID: 3367172.

15. Thiis-Evensen E, Hoff GS, Sauar J, Langmark F, Majak BM, Vatn MH. Population-based surveillance by colonoscopy: effect on the incidence of colorectal cancer. Telemark Polyp Study I. Scand J Gastroenterol. 1999; 34:414–420. PMID: 10365903.

16. Schoen RE, Pinsky PF, Weissfeld JL, et al. Colorectal-cancer incidence and mortality with screening flexible sigmoidoscopy. N Engl J Med. 2012; 366:2345–2357. PMID: 22612596.

17. Segnan N, Armaroli P, Bonelli L, et al. Once-only sigmoidoscopy in colorectal cancer screening: follow-up findings of the Italian Randomized Controlled Trial--SCORE. J Natl Cancer Inst. 2011; 103:1310–1322. PMID: 21852264.

18. Hoff G, Grotmol T, Skovlund E, Bretthauer M. Risk of colorectal cancer seven years after flexible sigmoidoscopy screening: randomised controlled trial. BMJ. 2009; 338:b1846. PMID: 19483252.

19. Newcomb PA, Norfleet RG, Storer BE, Surawicz TS, Marcus PM. Screening sigmoidoscopy and colorectal cancer mortality. J Natl Cancer Inst. 1992; 84:1572–1575. PMID: 1404450.

20. Selby JV, Friedman GD, Quesenberry CP Jr, Weiss NS. A case-control study of screening sigmoidoscopy and mortality from colorectal cancer. N Engl J Med. 1992; 326:653–657. PMID: 1736103.

21. Muller AD, Sonnenberg A. Protection by endoscopy against death from colorectal cancer. A case-control study among veterans. Arch Intern Med. 1995; 155:1741–1748. PMID: 7654107.

22. Scheitel SM, Ahlquist DA, Wollan PC, Hagen PT, Silverstein MD. Colorectal cancer screening: a community case-control study of proctosigmoidoscopy, barium enema radiography, and fecal occult blood test efficacy. Mayo Clin Proc. 1999; 74:1207–1213. PMID: 10593348.

23. Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M. Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann Intern Med. 2011; 154:22–30. PMID: 21200035.

24. Brenner H, Hoffmeister M, Arndt V, Stegmaier C, Altenhofen L, Haug U. Protection from right- and left-sided colorectal neoplasms after colonoscopy: population-based study. J Natl Cancer Inst. 2010; 102:89–95. PMID: 20042716.

25. Kahi CJ, Imperiale TF, Juliar BE, Rex DK. Effect of screening colonoscopy on colorectal cancer incidence and mortality. Clin Gastroenterol Hepatol. 2009; 7:770–775. PMID: 19268269.

26. Manser CN, Bachmann LM, Brunner J, Hunold F, Bauerfeind P, Marbet UA. Colonoscopy screening markedly reduces the occurrence of colon carcinomas and carcinoma-related death: a closed cohort study. Gastrointest Endosc. 2012; 76:110–117. PMID: 22498179.

27. Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009; 150:1–8. PMID: 19075198.
28. Singh H, Nugent Z, Demers AA, Kliewer EV, Mahmud SM, Bernstein CN. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology. 2010; 139:1128–1137. PMID: 20600026.

29. Amri R, Bordeianou LG, Sylla P, Berger DL. Impact of screening colonoscopy on outcomes in colon cancer surgery. JAMA Surg. 2013; 148:747–754. PMID: 23784448.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download