Abstract
Peritonsillar abscess is a common deep throat infection. Early diagnosis and prompt, appropriate management of a peritonsillar abscess prevents mortality. A 45-year-old woman on steroids for an ulcerative colitis (UC) exacerbation presented with sore throat and multiple skin ulcers on her left forearm and right foot. Computed tomography of the neck revealed a peritonsillar abscess. Gram staining and culture of the abscess were negative, and a skin biopsy suggested pyoderma gangrenosum (PG). The final diagnosis was peritonsillar involvement of steroid-refractory PG-associated UC. The patient showed a complete response to infliximab. Here, we report a case of successful infliximab treatment for peritonsillar involvement of steroid-refractory PG-associated UC.
Pyoderma gangrenosum (PG) is a rare inflammatory skin disease characterized by painful nodules or papulopustules that rapidly develop into ulcers with irregular margins. PG seldom presents as atypical nodules or aseptic abscesses.1,2 PG lesions, a cutaneous manifestation of IBD, can occur anywhere on the body, but the most common sites are the shins and regions adjacent to stomas.3,4 We report here the case of a PG lesion at an atypical site: the peritonsillar area presenting with an abscess. To our knowledge, this is the first report of PG-associated UC presenting with a peritonsillar abscess.
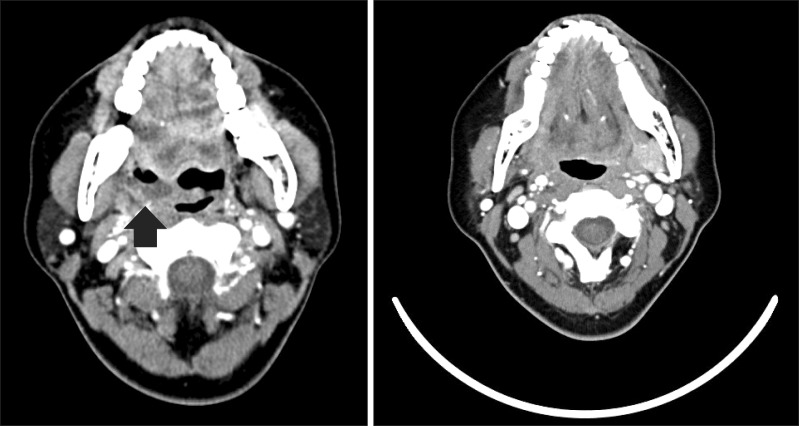
A 45-year-old woman with a history of UC presented with bloody diarrhea and abdominal pain that worsened 10 days before visiting the hospital. Over the previous 3 years, she was treated with oral sulfasalazine and suppository mesalazine. Colonoscopy showed diffuse ulcers and nodules with mucosal edema and hemorrhage (Fig. 1). The patient was diagnosed with a severe episode of UC and was treated with prednisolone (40 mg/day). On the seventh day of admission, her UC worsened and she had an increased number of bloody stools and a fever (38.7℃). The patient also developed a sore throat and painful nodules on her left forearm and foot that progressed rapidly to ulcers with irregular margins (Fig. 2A). Biopsy of a skin lesion revealed massive lymphocytic, neutrophilic infiltration in the dermal interstitium with abscess formation (Fig. 2B). On oral examination for her sore throat, the tonsils were found to be extremely swollen and fluctuant with pus, which was collected for gram staining and culture analysis. CT of the neck revealed a hypodense mass with gas formation consistent with a peritonsillar abscess (Fig. 3A). The abscess was incised and drained and the patient was administered empirical intravenous antibiotics. Gram staining, and bacterial and fungal cultures were negative; therefore, antibiotics were discontinued. We diagnosed steroid-refractory PG-associated UC with peritonsillar involvement and a sterile abscess. For treatment of the steroid-refractory UC, the patient received 5 mg/kg of infliximab intravenously at 0, 2, and 6 weeks, and then every 8 weeks thereafter. The sterile peritonsillar abscess disappeared (Fig. 3B), and the skin lesions regressed significantly 4 weeks after the first infliximab infusion (Fig. 4). The patient was discharged and has been receiving infliximab as maintenance therapy.
Pyoderma gangrenosum (PG) is a rare, immune-mediated ulcerating skin disease. The cause of PG remains unknown, but up to 50% of cases occur in association with other conditions such as IBD, connective tissue disease, or hematological disorders.5,6 PG skin lesions are commonly associated with IBD and occur in approximately 1-2% of patients with IBD. In Korea, the incidence of PG-associated IBD is unknown with few reported cases.7 Some evidence suggests that it is not related with the clinical activity of the underlying intestinal disease, but sometimes coincides with disease exacerbation or treatment failure.4 PG is clinically diagnosed based on characteristic features and the exclusion of other specific skin disorders.8 The typical features of PG are single or multiple erythematous papules or pustules, but subsequent necrosis of the dermis leads to the development of deep ulcers that contain purulent material that is sterile on culture. However, PG rarely presents as atypical nodules or aseptic abscess.1,2
PG lesions can occur anywhere on the body. The most common sites are the shins and regions adjacent to stomas, but oral involvement is uncommon. Previous reports of prominent involvement of the oral mucosa in patients with PG indicate that the most common sites are the tongue, palate, lips, buccal mucosa, and gingiva.9 In this case, PG occurred on the left forearm and right foot, and in the peritonsillar space. The sterile abscess in the peritonsillar space was a variant of PG. Peritonsillar abscess is a common deep throat infection; early diagnosis and prompt, appropriate management are critical to avoid mortality. Standard treatment is antibiotics, incision, and drainage.
However, the peritonsillar lesion in this case presented as a sterile abscess, which is a variant presentation of PG-associated UC. In contrast with a pyogenic abscess, PG must be treated immediately with immunosuppressive drugs. Therefore, when a UC patient presents with a peritonsillar abscess, peritonsillar involvement of PG should be considered a differential diagnosis.
There are no uniform guidelines for the effective treatment of PG. Traditional treatment involves the use of systemic steroids and immunosuppressive drugs such as cyclosporine.10 Recently, anti-tumor necrosis factor-alpha biologic drugs have extended the therapeutic choice for IBD. In a controlled trial for PG, a larger number of patients in the infliximab-treated group (46%, 6/13) showed improvement compared with those in the placebo group (6%, 1/17). Twenty of twenty-nine patients (69%) on infliximab showed a beneficial clinical response.11 In our case, the patient developed PG while on steroid treatment. Therefore, steroid-refractory PG-associated UC was diagnosed and infliximab treatment was initiated. The patient showed good clinical response. Although more data are needed to determine the efficacy and safety of infliximab for steroid-refractory PG-associated UC, infliximab is a therapeutic option for steroid-refractory PG-associated UC.
In conclusion, PG lesions can occur anywhere on the body, but peritonsillar involvement is rare. PG rarely presents as atypical nodules or sterile abscesses. We report the case of a patient with PG who presented with a peritonsillar abscess at an atypical site.
References
1. Johnson JL, West DA, Haggstrom AN. Pyoderma gangrenosum associated with an aseptic splenic abscess in a patient with neurofibromatosis. Pediatr Dermatol. doi: 10.1111/pde.12129. Published online ahead of print 28 March 2013.

2. Allen CP, Hull J, Wilkison N, Burge SM. Pediatric pyoderma gangrenosum with splenic and pulmonary involvement. Pediatr Dermatol. 2013; 30:497–499. PMID: 23627664.

3. Tavarela Veloso F. Review article: skin complications associated with inflammatory bowel disease. Aliment Pharmacol Ther. 2004; 20(Suppl 4):50–53. PMID: 15352894.
5. von den Driesch P. Pyoderma gangrenosum: a report of 44 cases with follow-up. Br J Dermatol. 1997; 137:1000–1005. PMID: 9470924.

6. Crowson AN, Mihm MC Jr, Magro C. Pyoderma gangrenosum: a review. J Cutan Pathol. 2003; 30:97–107. PMID: 12641787.

7. Yoo YW, Jung SH, Lee YJ, et al. A case of pyoderma gangrenosum associated with ulcerative colitis. Intest Res. 2008; 6:80–84.
8. Van Assche G, Dignass A, Bokemeyer B, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 3: special situations. J Crohns Colitis. 2013; 7:1–33. PMID: 23040453.

9. Paramkusam G, Meduri V, Gangeshetty N. Pyoderma gangrenosum with oral involvement - case report and review of the literature. Int J Oral Sci. 2010; 2:111–116. PMID: 20737938.

10. Reichrath J, Bens G, Bonowitz A, Tilgen W. Treatment recommendations for pyoderma gangrenosum: an evidence-based review of the literature based on more than 350 patients. J Am Acad Dermatol. 2005; 53:273–283. PMID: 16021123.

11. Brooklyn TN, Dunnill MG, Shetty A, et al. Infliximab for the treatment of pyoderma gangrenosum: a randomised, double blind, placebo controlled trial. Gut. 2006; 55:505–509. PMID: 16188920.

Fig. 1
Colonoscopic finding. Colonoscopy shows diffuse ulcers and nodularity with mucosal edema and hemorrhage at the sigmoid colon and rectum.
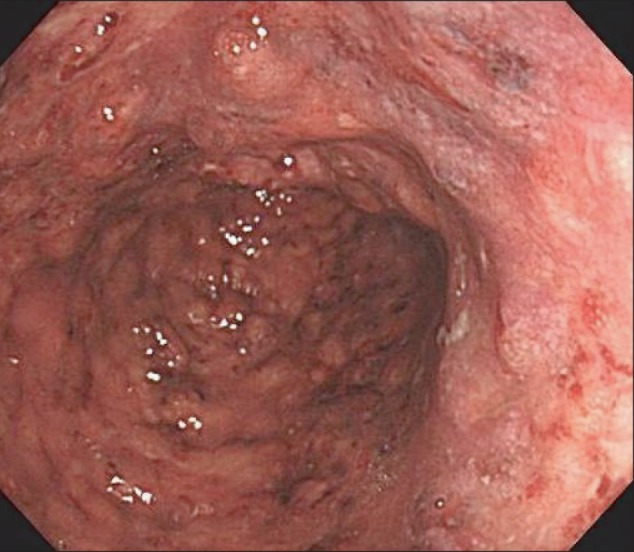
Fig. 2
Skin lesions and biopsy finding. (A) A large ulcer with edema, exudate, and pus on the left forearm and foot (B) Massive lymphocytic and neutrophilic infiltration (arrow) of the dermal interstitium (black star) suggestive of pyoderma gangrenosum (PG) (H&E stain, ×100).





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download