Abstract
Background/Aims
Vaccinations in patients with inflammatory bowel disease (IBD) are recommended to prevent infectious diseases. However, there are few reports of vaccination in IBD patients in Korea. The frequency of complementary and alternative medicine (CAM) use is high despite its uncertain effectiveness. This study aimed to identify the rates of vaccination and use of CAM in patients with IBD.
Methods
A total of 219 patients attended an education session for IBD patients held at Severance Hospital on March 23, 2013. We conducted a survey on vaccination and CAM use in IBD patients; 120 patients completed the questionnaire.
Results
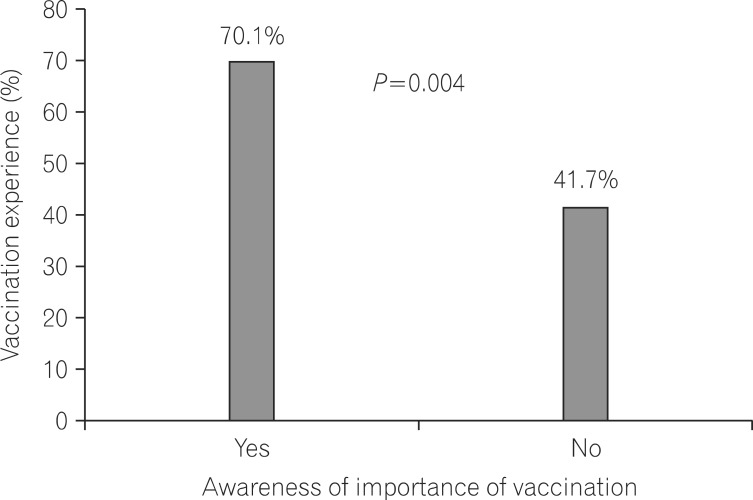
The influenza vaccination rate was 44.2% and pneumococcal vaccination rate was 4.2%. Thirty-one (66%) patients were aware of the importance of vaccination. The vaccination rate was higher in patients who were aware of the importance of vaccination compared with that in patients who were unaware of the importance of vaccination (70.1% vs. 41.7%, P=0.004). The rate of CAM use was 30.0%. The most commonly used CAMs were oral products: vitamins (33.3%), red ginseng (25.0%), and probiotics (19.4%).
Conclusions
Awareness of the importance of vaccination and actual vaccination rates were low in IBD patients. Despite insufficient evidence on the effectiveness of CAMs in IBD patients, many patients used CAMs. We believe that repeated education and promotion of vaccination are important. Further large-scale studies to investigate the efficacy and safety of CAMs are warranted in patients with IBD.
Ulcerative colitis (UC), CD, and BehÇet disease (BD) are chronic IBD with unidentified causes. The clinical manifestations of these diseases vary from intestinal symptoms such as diarrhea, abdominal pain, or intestinal hemorrhage, to extra-intestinal symptoms such as arthritis, ocular symptoms, or skin manifestations. IBD is characterized by a relatively early age of onset and chronic repeated relapse and remission.1 Therefore, patients with IBD require lifelong healthcare services including consistent management and regular follow-up examinations. IBD has arisen as a socio-economic problem in recent years with an increasing incidence and prevalence in East Asia.2,3,4
Steroids, immunomodulators, and/or tumor necrosis factor (TNF)-α blockers are commonly used in patients with IBD.5,6 The risk of opportunistic infectious diseases is increased in patients with IBD due to exogenous immunosuppressive medications and also due to the endogenous immunosuppressive mechanism of IBD itself.7 In a study conducted in the United States, infection was the most common cause of hospital admission, accounting for 27.5% of all patients admitted with IBD; sepsis and pneumonia were the leading causes of death.8 The major causes of pneumonia, including infection with influenza virus, pneumococcus, and other bacterial species, could be prevented with appropriate vaccination.9 Therefore, several clinical practice guidelines for IBD patients recommend annual vaccination.7 However, both doctors and patients have overlooked the importance of vaccination in clinical practice. In addition, the status of vaccination in IBD patients has been insufficiently investigated in Korea.
Complementary and alternative medicine (CAM) includes a wide range of treatments with different definitions. The National Center for Complementary and Alternative Medicine (NCCAM) has defined CAM as a group of diverse medical and healthcare systems, practices, and products that are not presently considered a part of conventional medicine.10 Despite the use of various medications such as steroids, immunomodulators, and TNF-α blockers, symptoms are only partially controlled in some patients. Many CAM treatments for IBD have not yet been medically proven. However, many people believe that CAM treatments are less toxic and considerably safer than the standard medical treatment and this has generated growing interest and increased usage.11 Some studies report that 21-60% of IBD patients in Western countries use CAM treatments.1,12 However, there has been little investigation of the use of CAM by IBD patients in Korea, probably due to a lack of interest by physicians. We therefore performed this study to investigate the status and patient awareness of vaccination and CAM use in IBD patients.
The survey included IBD patients who attended an educational session held at the Severance Hospital, Yonsei University College of Medicine on March 23, 2013. The aim of the survey was to examine the experiences of vaccination and CAM use in patients diagnosed with UC, CD, or BD. Of the 219 patients who attended the education session, 120 completed the questionnaire. The survey questionnaire comprised vaccination-related items and CAM-related items. Vaccination-related items included the awareness of the importance of vaccination in IBD patients, whether the patient had received an explanation of the importance of vaccination from physicians, vaccination history, and reasons for refusing vaccination. Regarding types of vaccinations, respondents were able to choose from multiple answers: vaccines for hepatitis A virus, hepatitis B virus, pneumococcus, human papillomavirus, influenza and herpes zoster. CAM-related items included questions on whether the patients had taken CAMs, the purchase route, the reasons for CAM treatment, and subjective effectiveness.
This study was performed following institutional review board (IRB) approval (4-2013-0811) from Severance Hospital.
The chi-square test was used for the analysis of categorical data between groups. One-way ANOVA was used to analyze differences in continuous variables. Differences were considered statistically significant at P<0.05. All statistical analyses were performed using SPSS Statistics 17.0 software (SPSS Inc., Chicago, IL, USA).
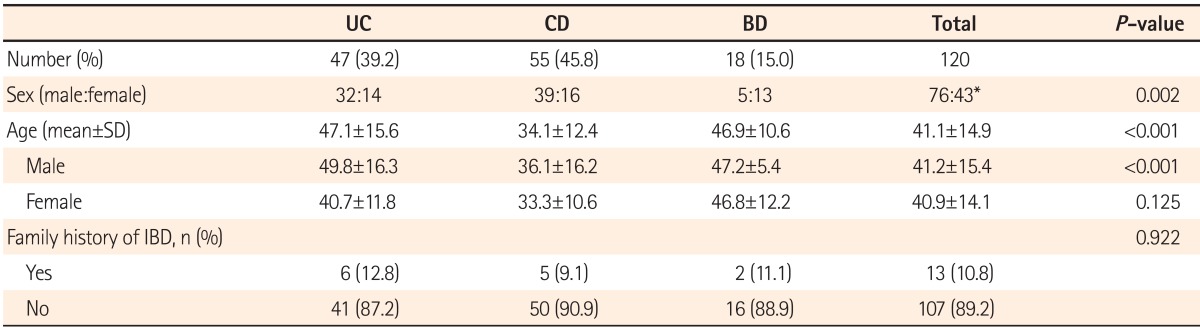
The mean age of the 120 survey respondents was 41.1±14.9 years. There were 76 men (63.3%) and 43 women (35.8%) (1 patient did not answer the question about sex). The most common form of IBD was CD in 55 patients (45.8%), followed by UC in 47 patients (39.2%) and BD in 18 patients (15%). There were 32 (69.6%) male UC patients and 14 (30.4%) female UC patients, with 1 non-respondent (2.1%); 39 (70.9%) male CD patients and 16 (29.1%) female CD patients; and 5 (27.8%) male BD patients and 13 (72.2%) female BD patients. The mean age was 47.1±15.6 years in the UC patients, 34.1±12.4 years in the CD patients, and 46.9±10.6 years in the BD patients. Thirteen patients (10.8%) had a family history of IBD and 107 patients (89.2%) had no family history of IBD (Table 1).
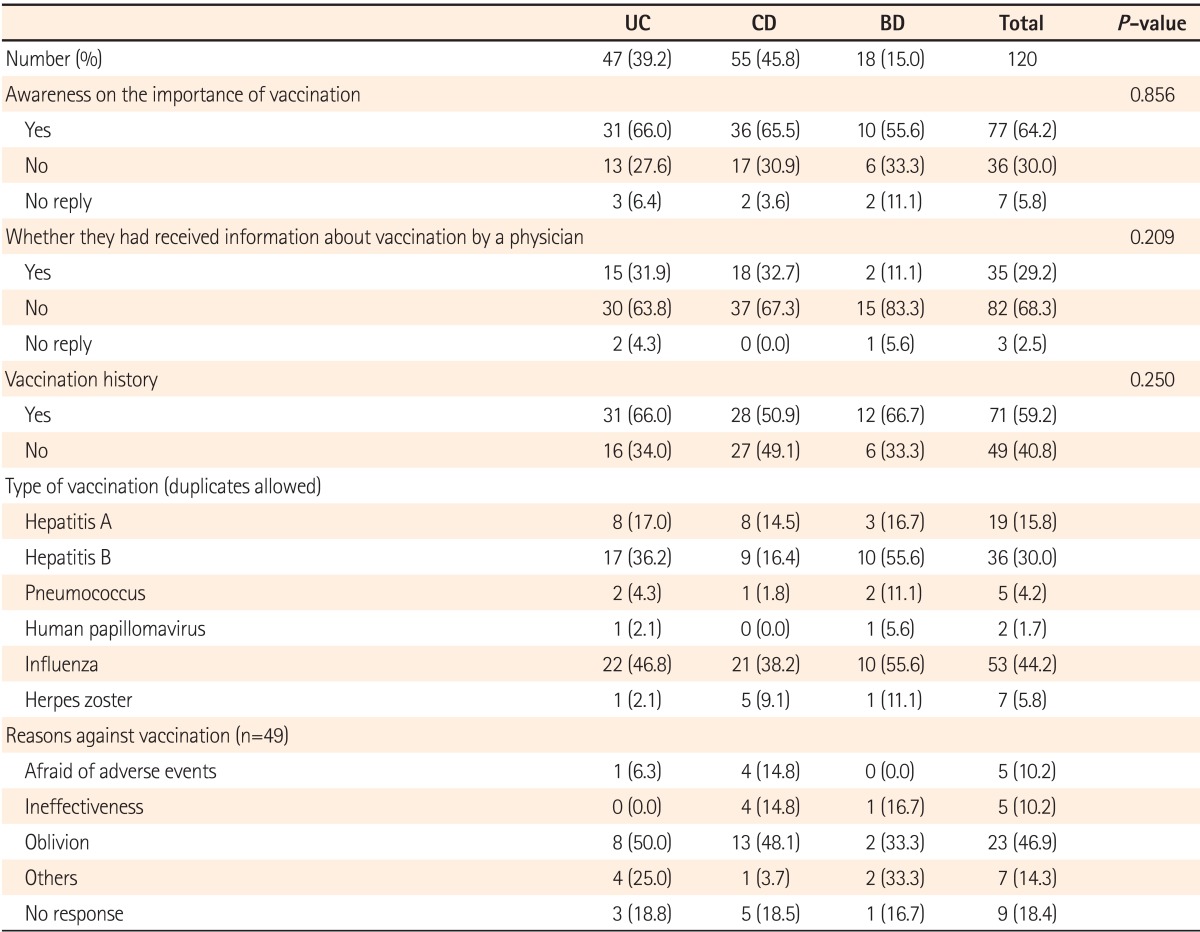
The response to the question "vaccination is more important in IBD patients than healthy individuals" was "yes" in 77 (64.2%) patients and "no" in 36 (30.0%) patients; 7 patients (5.8%) did not reply. Among the UC patients, 31 (66.0%) answered "yes," 13 (27.7%) answered "no," and 3 (6.4%) did not reply to this question. Among the CD patients, 36 (65.5%) answered "yes," 17 (30.9%) answered "no," and 2 (3.6%) did not reply to this question. Among the BD patients, 10 (55.6%) answered "yes," 6 (33.3%) answered "no," and 2 (11.1%) did not reply to this question. No statistical difference was found between the diseases. Thirty-five patients (29.2%) reported that they had been informed by their physicians of the necessity of vaccination, whereas 82 patients (68.3%) had not been informed. Among those who were informed, 15 had UC (31.9%), 18 had CD (32.7%), and 2 had BD (11.1%). Patients who had not been informed about vaccination by their physicians were asked to answer further questions on the alternative sources of information on vaccination. Twenty-one patients (52%) responded that they received information through the internet and 10 (22%) through an IBD patients' association. However, physician-delivered information on the vaccination was not significantly different between disease groups (P=0.209). Of all the respondents, 54 patients (70.1%) were aware of the importance of the vaccination, whereas 15 patients (41.7%) were unaware. The vaccination rate was significantly higher in patients who were aware of the importance of vaccination than in those who were unaware (P=0.004; Fig. 1). Excluding vaccinations during childhood, 71 respondents (59.2%) had received ≥1 vaccination (hepatitis A, hepatitis B, pneumococcus, human papillomavirus, influenza, and/or herpes zoster), whereas 49 (40.8%) had not. The total vaccination rate was not significantly different among the disease groups. Among those who were vaccinated, 19 patients (15.8%) were vaccinated against hepatitis A, 36 (30.0%) against hepatitis B, 5 (4.2%) against pneumococcus, 2 (1.7%) against human papillomavirus, 53 (44.2%) against influenza, and 7 (5.8%) against herpes zoster. Those who were not vaccinated were asked to state the reason for the non-vaccination. Twenty-three patients (46.9%) replied that had forgotten the type of vaccination, 5 (10.2%) stated fear of adverse events, 5 (10.2%) thought that vaccines were ineffective, 7 patients (14.3%) stated other reasons, and 9 patients (18.4%) did not reply (Table 2).
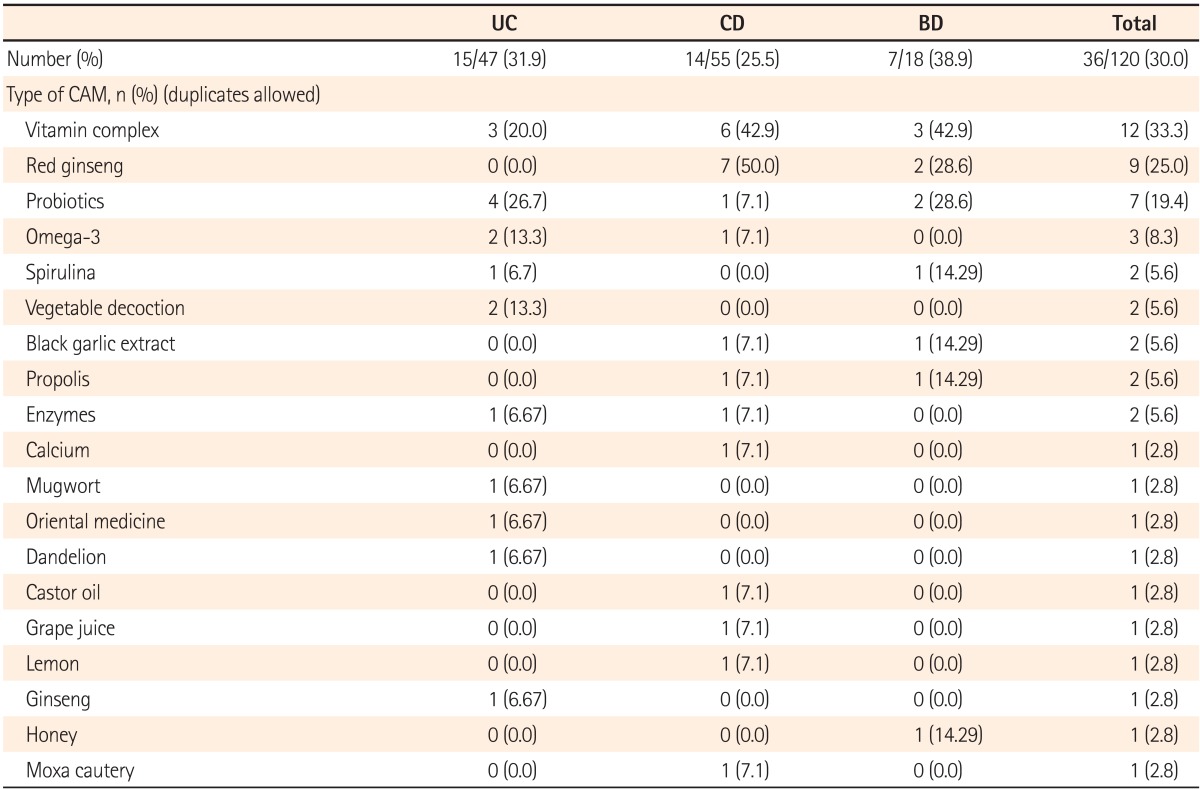
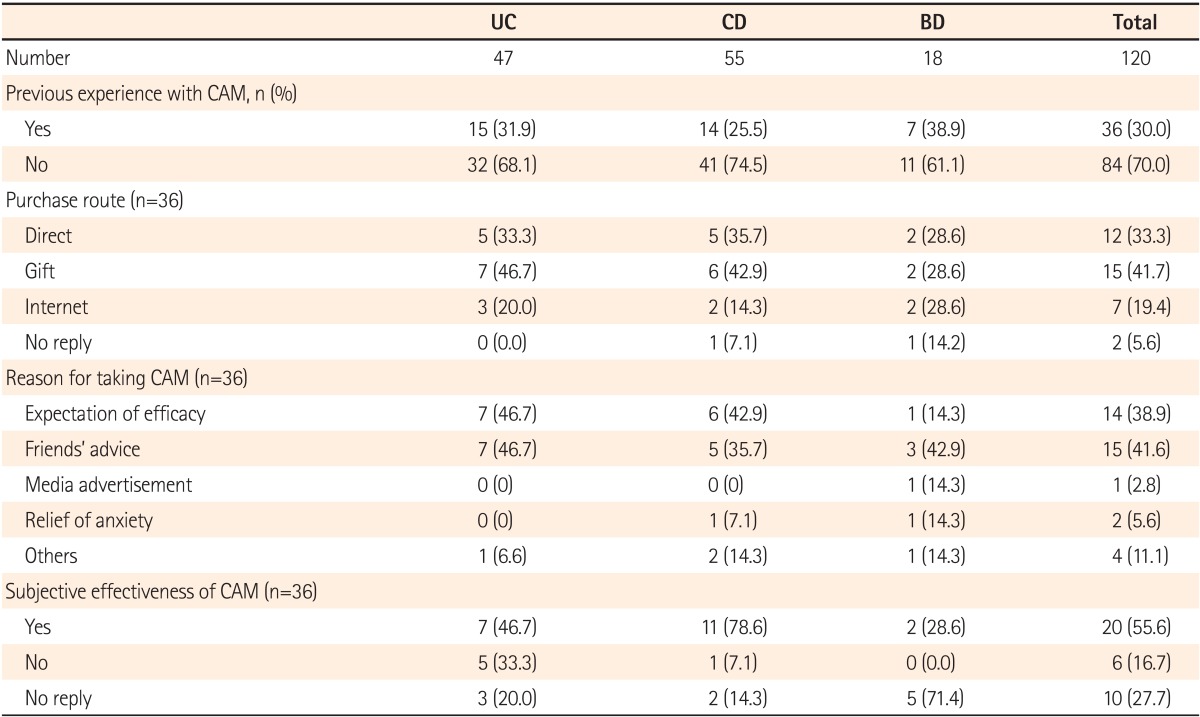
According to the survey results, 36 patients (30.0%) were currently taking a functional health food or folk remedy, whereas 84 patients (70.0%) were not. Of the 36 patients using a CAM, the most common was vitamins in 12 (33.0%) patients, followed by red ginseng in 9 (25.0%) and probiotics in 7 (19.4%). Other CAM treatments included omega-3 products, spirulina, garlic extract, cabbage decoction, dandelion decoction, mugwort, and propolis (Table 3). CAM products were purchased directly in 12 patients (33.3%), gifted by friends or family members in 15 (41.6%), and purchased through the internet in 7 (19.4%). Considering the reason for CAM use, 14 patients (38.9%) stated improvement in symptoms, 15 (41.6%) stated friends' suggestions, 1 (2.7%) stated the media, 2 (5.6%) stated relief of anxiety, 4 (11.1%) stated other reasons, and 7 (18.9%) did not respond. CAM use was found to be subjectively effective in 20 patients (55.6%) and subjectively ineffective in 6 patients (16.7%); 10 patients (27.8%) did not answer this question (Table 4).
Our study aimed to develop strategies for the improvement in vaccination and CAM use in Korean patients with IBD in actual clinical setting based on the survey results. Immunosuppression may occur as a result of treatment in IBD patients due to the use of immunomodulators or as a result of underlying disease, thus increasing susceptibility to opportunistic infection. Therefore, the importance of vaccination should be emphasized more in IBD patients than in other patients. However, it is often overlooked, not only by patients but also by physicians.13,14 According to a study performed in the United States, 86% of patients with IBD received immunosuppressive treatment. In contrast, only 28% were vaccinated against influenza and only 9% against pneumococcus.15,16 A Korean study showed similar results, with a low vaccination rate (37.5% with the influenza vaccine and 6.3% with the pneumococcal vaccine).17 In our study, the vaccination rates were 44.2% with the influenza vaccine and 5% with the pneumococcal vaccine, which were comparable with previous results. Hepatitis A, hepatitis B, and human papillomavirus vaccination rates were even lower, ranging between 1.7% and 29.2%.
Rheumatoid arthritis shares similar characteristics with IBD in that both are immune disorders and require the use of steroids and TNF-α blockers. According to the results of a German cohort study on patients with rheumatoid arthritis and IBD, the proportion of patients aware of the importance of vaccination and those who received information from doctors (rheumatology specialists, general physicians) on the need for vaccination were 78.4% and 44.2%, respectively; both these values are higher than those found in our study.18 The actual vaccination rate was also higher than that in our study; 65.3% with the influenza vaccine and 65.3% with the pneumococcal vaccine. According to subgroup analysis, the patient group most aware of the need for vaccination (age ≥60 years, use of anti-TNF agent or rituximab) had a higher pneumococcal vaccination rate.18 Similarly, in our study the vaccination rate was also higher in the patients who were aware of the importance of vaccination.
A recent study performed in the United States proposed that the vaccination rate for influenza and pneumococcus could be enhanced systematically, for example by keeping medical records of medications and vaccination status, and by providing repeated education targeting patients as well as healthcare providers.19 Likewise, checking each patient's vaccination status regularly at outpatient clinics is crucial to increase the vaccination rate.
In our survey, 36 patients (30.0%) responded that they were current users of CAMs, mostly oral products. This result is comparable to that of a previous Korean study in patients with stomach cancer.20 In a New Zealand study on IBD patients, the most common CAM was oral products, as in our study. However, in a German study, the most common CAM was homeopathy, accounting for 52.9%.1,11 This difference can be attributed to differing cultural backgrounds and types of traditional CAMs.
The reason for CAM use was mostly due to friends and family members in our study. Despite the subjective effectiveness reported by >50% of respondents, this raises a particular concern that patients have not discussed the use of CAM with their doctors. Thus, they may be receiving inaccurate information on CAMs, which could result in interaction with other medications and cause adverse events. Therefore, physicians should be more aware of current CAM use in patients and provide objective and accurate information to patients.
Patients are vulnerable to unfiltered information provided through the internet and mass media. Lack of proper education and provision of inaccurate information may lead to psychological instability and anxiety about medications and surgical procedures important to the treatment of IBD. In our study, the proportion of patients who obtained medical information from the internet rather than from their physicians was high. Therefore, educational sessions and academic symposiums held by hospitals and academic institutes will provide IBD patients with knowledge and understanding.
There are some limitations to this study. Since the survey results were acquired from a single tertiary hospital, selection and recall biases are inevitable. The proportion of CD patients was higher than that of the UC patients, and this does not reflect the relative prevalences of types of IBD in Korea. This finding may indicate indirectly that CD patients are more interested in the education sessions. In addition, the authors were unable to analyze other objective data including disease status, current medication, serological test results before vaccination, and infection history, due to the anonymous conditions of the survey. Since patients who already had antibodies against hepatitis A and B would not have received additional vaccinations, the exact vaccination rate could be slightly lower than that recorded here. Moreover, determination of the overall frequency of use of probiotics in IBD patients could be inaccurate because we were unable to ascertain whether probiotics were prescribed by physicians. Finally, data on the socioeconomic status of patients were limited. Additional studies are needed to further investigate the efficacy, safety, and predictive factors for the use of CAMs.
References
1. Koning M, Ailabouni R, Gearry RB, Frampton CM, Barclay ML. Use and predictors of oral complementary and alternative medicine by patients with inflammatory bowel disease: a population-based, case-control study. Inflamm Bowel Dis. 2013; 19:767–778. PMID: 23429459.

2. Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008; 14:542–549. PMID: 17941073.

3. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54. PMID: 22001864.

4. Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asiapacific Crohn's and colitis epidemiology study. Gastroenterology. 2013; 145:158–165. PMID: 23583432.

5. Ye BD, Yang SK, Shin SJ, et al. Guidelines for the management of Crohn's disease. Korean J Gastroenterol. 2012; 59:141–179. PMID: 22387837.

6. Choi CH, Kim YH, Kim YS, et al. Guidelines for the management of ulcerative colitis. Korean J Gastroenterol. 2012; 59:118–140. PMID: 22387836.

7. Gisbert JP, Chaparro M. Vaccination strategies in patients with IBD. Nat Rev Gastroenterol Hepatol. 2013; 10:277–285. PMID: 23419290.

8. Ananthakrishnan AN, McGinley EL. Infection-related hospitalizations are associated with increased mortality in patients with inflammatory bowel diseases. J Crohns Colitis. 2013; 7:107–112. PMID: 22440891.

9. Stobaugh DJ, Deepak P, Ehrenpreis ED. Hospitalizations for vaccine preventable pneumonias in patients with inflammatory bowel disease: a 6-year analysis of the Nationwide Inpatient Sample. Clin Exp Gastroenterol. 2013; 6:43–49. PMID: 23818801.

10. Complementary, alternative, or integrative health: what's in a name?. National Center for Complementary and Alternative Medicine (NCCAM) [homepage on the Internet]. Maryland: NCCAM publication;updated 2013 May. cited 2008 October. Available from: http://nccam.nih.gov/health/whatiscam/.
11. Langhorst J, Anthonisen IB, Steder-Neukamm U, et al. Patterns of complementary and alternative medicine (CAM) use in patients with inflammatory bowel disease: perceived stress is a potential indicator for CAM use. Complement Ther Med. 2007; 15:30–37. PMID: 17352969.

12. Ng SC, Lam YT, Tsoi KK, Chan FK, Sung JJ, Wu JC. Systematic review: the efficacy of herbal therapy in inflammatory bowel disease. Aliment Pharmacol Ther. 2013; 38:854–863. PMID: 23981095.

13. Campins M, Cossio Y, Martinez X, Borruel N. Vaccination of patients with inflammatory bowel disease. Practical recommendations. Rev Esp Enferm Dig. 2013; 105:93–102. PMID: 23659508.

14. Wasan SK, Baker SE, Skolnik PR, Farraye FA. A practical guide to vaccinating the inflammatory bowel disease patient. Am J Gastroenterol. 2010; 105:1231–1238. PMID: 20104218.

16. Melmed GY. Vaccination strategies for patients with inflammatory bowel disease on immunomodulators and biologics. Inflamm Bowel Dis. 2009; 15:1410–1416. PMID: 19462435.

17. Yun HS, Min YW, Chang DK, et al. Factors associated with vaccination among inflammatory bowel disease patients in Korea. Korean J Gastroenterol. 2013; 61:203–208. PMID: 23624734.

18. Feuchtenberger M, Kleinert S, Schwab S, et al. Vaccination survey in patients with rheumatoid arthritis: a cross-sectional study. Rheumatol Int. 2012; 32:1533–1539. PMID: 21327432.

19. Parker S, Chambers White L, Spangler C, et al. A quality improvement project significantly increased the vaccination rate for immunosuppressed patients with IBD. Inflamm Bowel Dis. 2013; 19:1809–1814. PMID: 23714677.

20. Chae BJ, Song BJ, Kim SS, et al. Use of complementary and alternative medicine by gastric cancer patients. J Korean Surg Soc. 2007; 72:369–378.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download