Abstract
Background/Aims
The natural history of Crohn's disease (CD) is characterized by a remitting and relapsing course and a considerable number of patients ultimately require bowel resection. Moreover, postoperative recurrence is very common. Relatively few studies have investigated the postoperative recurrence of CD in Korea. The aim of the current study was to assess postoperative recurrence rates - both clinical and endoscopic - in CD as well as factors influencing postoperative recurrence.
Methods
Electronic medical records of patients who underwent surgery due to CD were reviewed and analyzed. Patients with incomplete surgical resection, a follow-up period of less than a year, and a history of strictureplasty or perianal surgery were excluded.
Results
Of 112 CD patients, 39 patients had history of bowel resection, and 34 patients met the inclusion criteria. Among them, 26 were male (76%) and the mean age of onset was 32.8 years. The mean follow-up period after operation was 65.4 months. Cumulative clinical recurrence rates were 8.8%, 12.5%, and 33.5% at 12, 24, and 48 months, respectively. Use of immunomodulators for prophylaxis was the only predictor of clinical recurrence in univariate analysis (P=0.042). Of 21 patients who had undergone follow-up colonoscopy after surgery, cumulative endoscopic recurrence rates were 33.3%, 42.9%, and 66.1% at 6, 12, and 24 months, respectively. No significant predicting factor for endoscopic recurrence was detected.
Crohn's disease (CD), a chronic inflammatory bowel disease characterized by a relapsing-remitting disease course, results in bowel resection in approximately 80% of patients.1 Despite bowel resection, recurrence is common. For this reason, follow-up is important after treatment.
Postoperative recurrence of CD can be primarily divided into endoscopic and clinical recurrence. Endoscopic recurrence is a risk factor of clinical recurrence, and more than 60% of all recurrences occur within a year postoperatively. Several previous studies have found that the risk of recurrence increased with smoking, a history of bowel resection, a lack of postoperative immunomodulator therapy, penetrating CD, and bowel resection of more than 25 cm.2,3,4 Clinical recurrence rates have been reported to range from10-30% during the first postoperative year and to be greater than 60% during the first postoperative decade. Additionally, approximately 50% of CD patients require reoperation. For these reasons, some experts have suggested that patients at high risk for recurrence should be identified and that therapeutic methods should be determined based on the severity of endoscopic recurrence to prevent postoperative recurrence. They recommended that postoperative colonoscopy should be performed 6-12 months after intestinal resection and that medical therapy would be started in patients with moderate to severe endoscopic recurrence.5,6,7,8 However, there are no prospective studies or practice guidelines pertaining to the initiation or duration of therapy for the prevention of postoperative recurrence.
A few studies have investigated the postoperative recurrence rate of CD in Korea. In a retrospective study including 160 patients who underwent bowel surgery, symptomatic recurrence rate was 15.9% and 36.4% at 2 and 5 years, and the cumulative surgical recurrence rate was 13.6% at the fifth postoperative year.9 Other smaller study reported cumulative surgical recurrence rates of 15% at the fifth year, 25% at the tenth year, and 60% at the fifteenth year, respectively.10 However, studies on postoperative clinical recurrence and the risk factors for recurrence in CD are few in number, and no studies have been conducted regarding endoscopic recurrence rate in Korea. For these reasons, we conducted this retrospective study to evaluate both clinical and endoscopic recurrence rates in CD patients who underwent bowel resection as well as the risk factors for postoperative recurrence.
We reviewed and analyzed the electronic medical records of patients who underwent surgery due to CD from July 1991 to October 2012 in St. Vincent's Hospital, the Catholic University of Korea. CD was diagnosed in accordance with the Guidelines of the Korean Association for the Study of Intestinal Diseases.11 Patients with incomplete surgical resection, a follow-up period of less than a year, and a history of strictureplasty or perianal surgery were excluded. The current study was performed after obtaining Institutional Review Board approval from St. Vincent's Hospital.
The endoscopic recurrence rate was examined in patients who underwent postoperative follow-up colonoscopy or capsule endoscopy and the clinical recurrence rate was examined in all patients regardless of a history of endoscopy. Clinical recurrence was defined by recurrent CD-related symptoms, taking a new medicine in addition to current medications, or a Crohn's Disease Activity Index (CDAI) score >150.3,4,12 Endoscopic recurrence was defined as grade 1 or higher of Rutgeerts scoring system (0: no aphthous ulcers; 1: less than five aphthous ulcers; 2: more than five aphthous lesions with normal intervening mucosa, skip areas of larger lesions, or lesions confined to ileocolonic anastomosis; 3: diffuse aphthous ileitis with diffusely inflamed mucosa; 4: diffuse inflammation with larger ulcers, nodules, and/or narrowing).13
Statistical analyses were performed using PASW Statistics version 18.0 (IBM Co., Armonk, NY, USA). Continuous variables were presented as the mean±SD. The risk factors for recurrence were analyzed by performing logistic regression analyses. Cumulative recurrence rates were analyzed using Kaplan-Meier survival functions. P-values less than 0.05 were considered statistically significant.
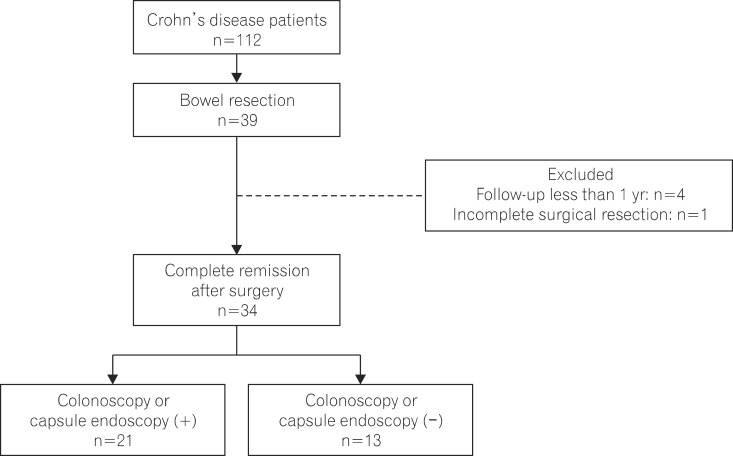
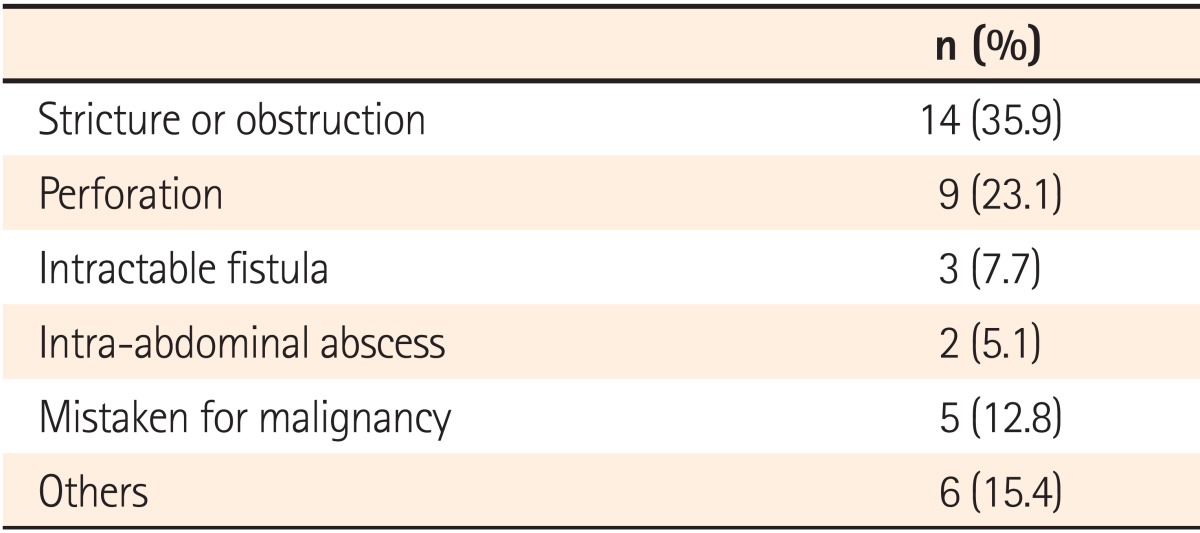
Of 112 CD patients who were regularly followed in St. Vincent's Hospital, 39 (34.8%) underwent bowel resection. Of these patients, 7 underwent bowel resection more than twice. The most common surgical cause was stricture or obstruction in 14 patients (35.9%), followed by perforation in 9 patients (23.1%), mistaken for malignancy in 5 patients (12.8%), fistulas unresponsive to medical treatment in 3 patients (7.7%), and abscess in 2 patients (5.1%). Six patients (15.4%) underwent bowel resections for other reasons including severe bleeding or misdiagnosis as appendicitis (Table 1). Performed surgical procedures were small bowel resection in 14 patients (35.9%), right hemicolectomy in 13 patients (33.3%), ileocecectomy in 6 patients (15.4%), and ileectomy in 2 patients (5.0%). Each of the following surgical procedures had one patient; total colectomy and partial small bowel resection, transverse colectomy, ileocolectomy and partial ascending colectomy, and resection in the anastomotic region. The analysis of clinical recurrence was performed on 34 patients who achieved complete remission by surgery and could be followed-up for more than a year. Of these, 21 patients were included in the analysis of endoscopic recurrence after undergoing follow-up colonoscopy or capsule endoscopy (Fig. 1).
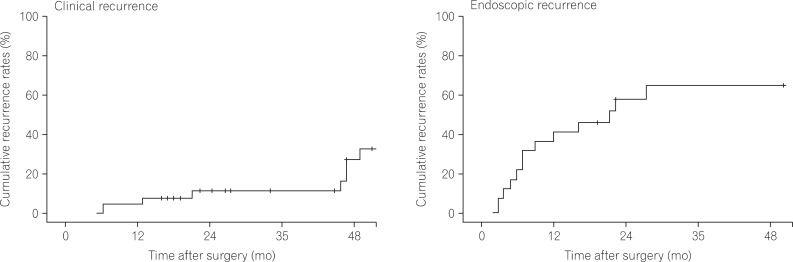
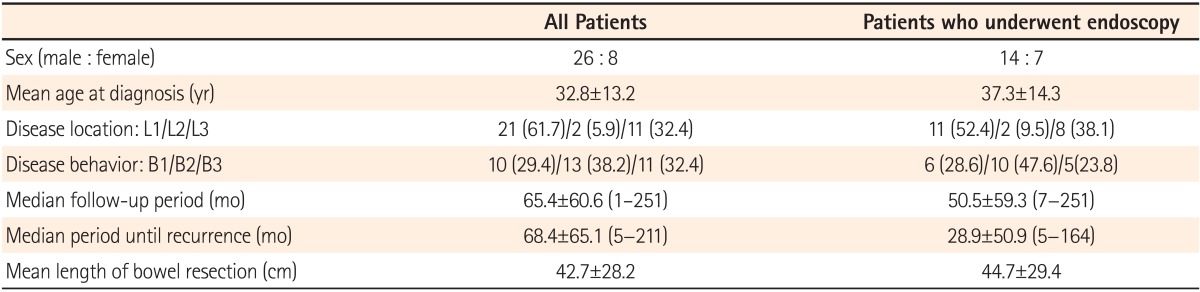
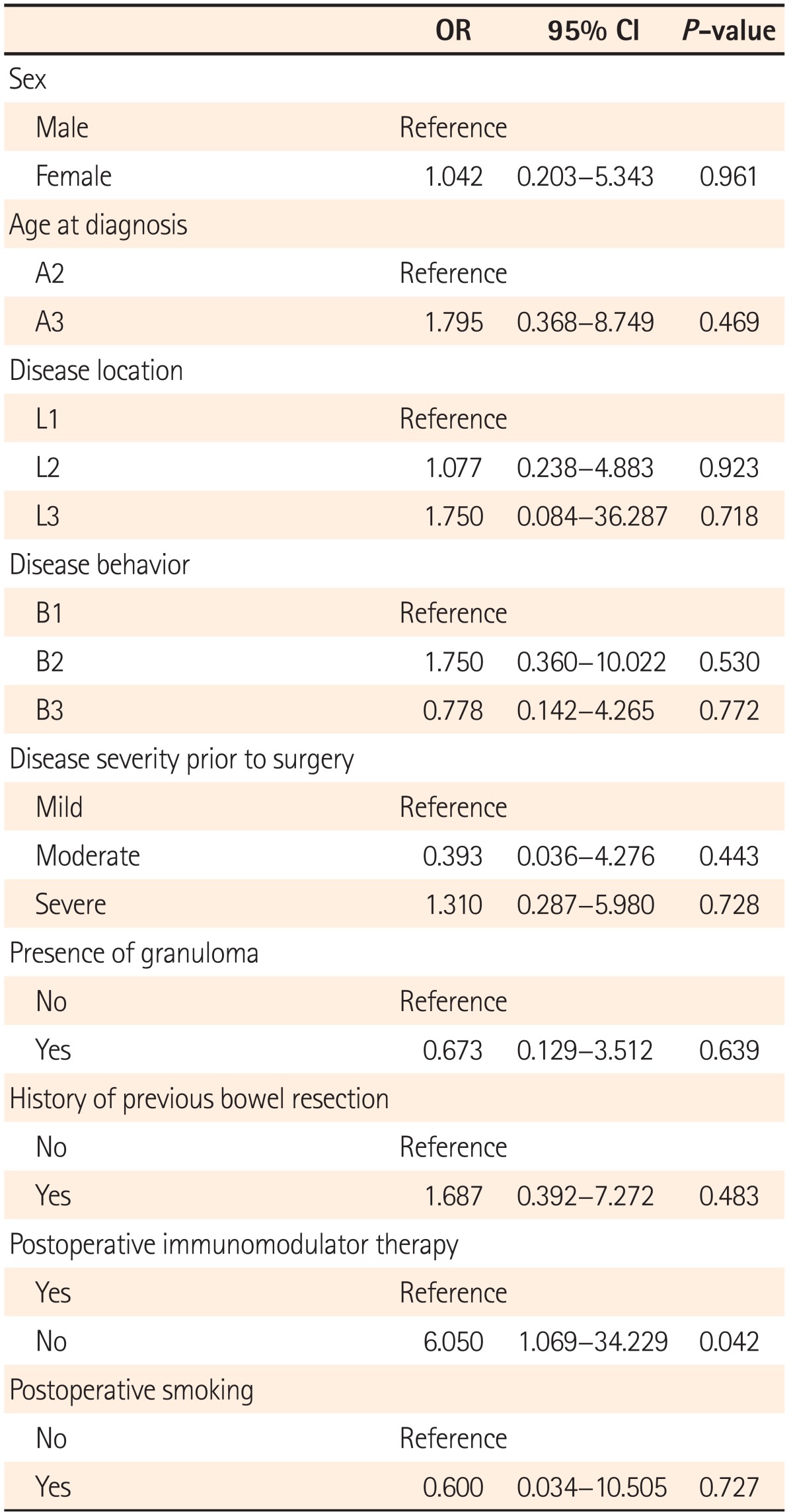
Of 34 patients analyzed for clinical recurrence rate, 26 were male (76%) and the mean age of onset was 32.8±13.2 years. The mean follow-up period was 65.4±60.6 months and the mean length of intestine resected was 42.7±28.2 cm. Clinical recurrence was shown in 13 patients (38.2%) and the median duration to recurrence was 68.4±65.1 months (Table 2). In univariate logistic regression analysis for factors influencing clinical recurrence, there was a significantly higher likelihood of clinical recurrence in patients who had no prophylaxis with immunomodulator (OR 6.050, 95% CI: 1.069-34.229, P=0.042). There was no difference in clinical recurrence rate regarding sex, age at diagnosis, duration of CD before resection, disease behavior, disease location, presence of granuloma, history of previous bowel resection, causes for operation, postoperative smoking status, and disease severity prior to surgery (Table 3). In the multivariate analysis, no factor was found to influence the clinical recurrence rate. According to Kaplan-Meier survival analysis, cumulative recurrence rates were 8.8% at 12 months, 12.5% at 24 months, and 33.5% at 48 months postoperatively (Fig. 2).
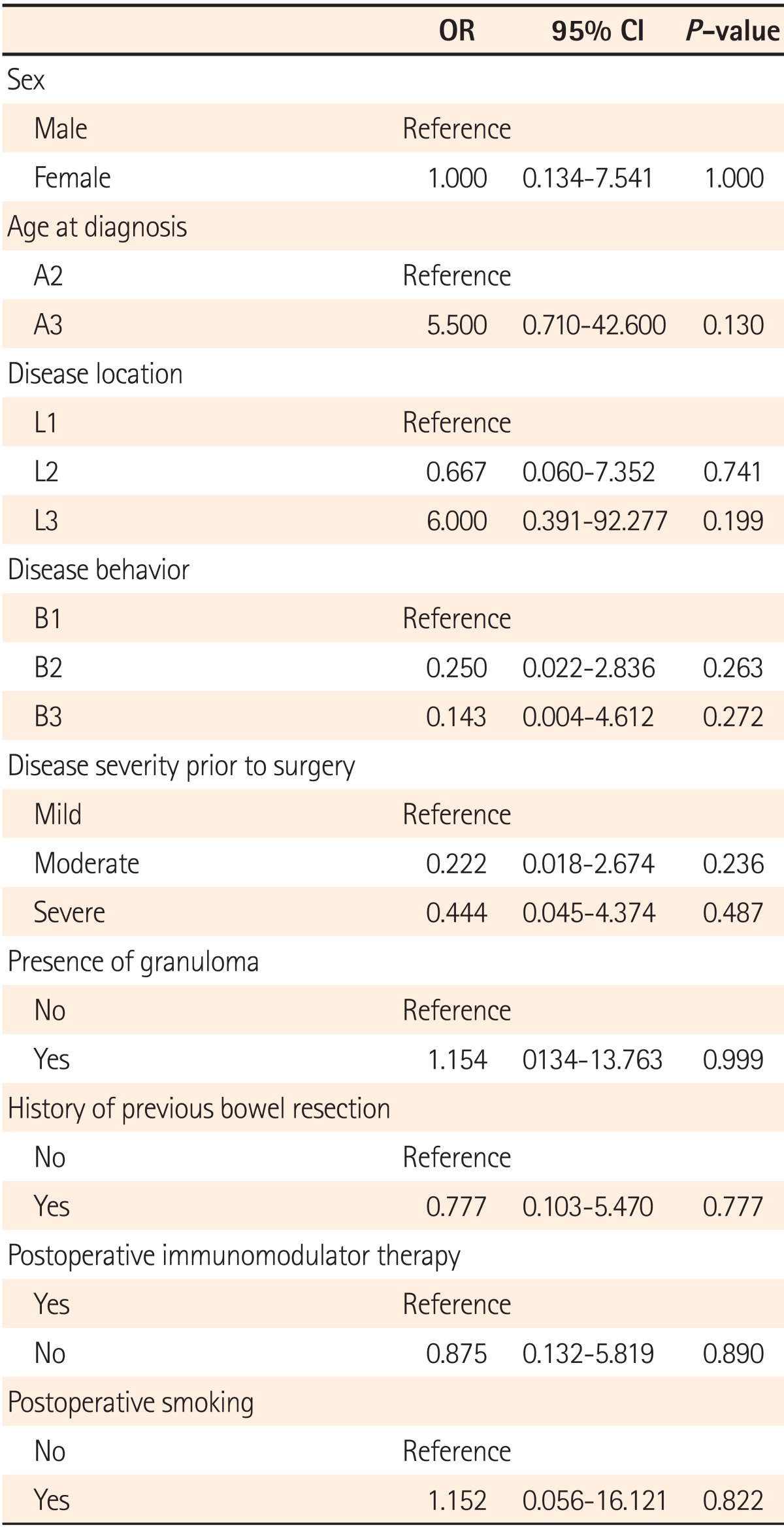
Among 21 patients who underwent follow-up colonoscopy, 14 were male (66.7%) and the mean age of onset was 37.3±14.3 years. The mean follow-up period was 50.5±59.3 months and the mean length of intestine resected was 44.7±29.4 cm. Of these, 15 patients (71.4%) showed endoscopic recurrence and the mean duration before endoscopy was 28.9±50.9 months (Table 1). Of the 15 patients with endoscopic recurrence, 14 showed a Rutgeerts score of grade 2 or higher. In 7 patients who underwent small bowel resection, endoscopic recurrence was detected with capsule endoscopy in 2 patients and with colonoscopy in 5 patients.
The surgical management of CD is not curative. Hence, recurrence is common for most patients with CD despite removal of all visible lesions. As a result, more than 50% of patients undergo re-operation in a 10-year postoperative period. Although a few studies on the postoperative recurrence of CD have been performed in Korea, these were mostly surgical studies pertaining to re-operation rates.9,10 To date, there have been no studies that have investigated the clinical or endoscopic recurrence of CD or the risk factors of postoperative recurrence.
The current study examined postoperative recurrence rates in CD patients who achieved complete remission by surgery and could be followed-up for more than a year. Clinical or endoscopic recurrence was found in 27 (79.1%) out of 34 patients, and recurrence rates were comparable to those of Western studies.14,15 The guidelines for postoperative surveillance of recurrence have not yet been established. However, follow-up endoscopy is recommended as the optimal monitoring method, as the CDAI score alone is insufficient for detecting recurrence.
Postoperative endoscopic recurrence precedes clinical recurrence and is a useful prognostic factor for clinical recurrence. However, in the current study, clinical recurrence was seen in only a single patient among 15 with endoscopic recurrence. This outcome is thought to be attributable to a relatively short follow-up period of 50.5±59.3 months in patients with endoscopic recurrence. With the exception of 2 patients with endoscopic recurrence after a 10-year postoperative period, the mean follow-up period was approximately 2 years (28.1±19.3 months) in 13 patients. Therefore, there are some limitations in verifying the association between endoscopic recurrence and clinical recurrence.
The Rutgeerts scoring system is widely used in evaluating endoscopic recurrence. The risk of clinical recurrence was higher in patients with a Rutgeerts score of grade 2 or greater.13 In the current study, endoscopic recurrence was defined as grade 1 or higher of Rutgeerts score and the observed endoscopic recurrence rate was 71.4%. However, even defining endoscopic recurrence as grade 2 or higher like previous studies, the recurrence rate was not much different (66.7%). Although there are other follow-up methods including abdominal sonography, virtual colonoscopy with abdominal CT, small bowel MRI, enteroscopy, and others, these are uncommonly used due to low sensitivity, high cost, and other problems.
In several Western studies on the risk factors for postoperative recurrence, smoking, penetrating CD, postoperative immunomodulator therapy, age at diagnosis, presence of granuloma, history of bowel resection, and genetic factors were found to be associated with re-operation rates.2,3,4,5,6 In Korean studies, stricturing CD, abdominal abscess, emergency surgery, and delayed postoperative diagnosis were identified to be related with re-operation rate.9,10 However, the use of a postoperative immunomodulator alone was associated with clinical recurrence in the current study. Because biological agents were used in only 2 patients for the prevention of postoperative recurrence, the effects of biological agents were unidentifiable. Although smoking is known as the only independent modifiable factor of all risk factors for recurrence according to previous studies,16 no association was observed between smoking and postoperative recurrence in the current study. This outcome is thought to be attributable to the considerable amount of patients (94.1%) who were not smoking at diagnosis, making an accurate analysis impossible to perform. Moreover, there were some limitations in verifying the association between the duration of CD before resection and recurrence rate, as 23 (67.6%) of 34 patients were first diagnosed with CD at the time of bowel resection.
Buisson et al.15 performed a study on the natural progress of postoperative CD and found that clinical recurrence rates ranged between 10-35% at 1 year and 35-85% at 3 years postoperatively and that endoscopic recurrence rates ranged between 35-85% at 1 year postoperatively. In the current study, cumulative clinical recurrence rates were 8.8% at 1 year, 12.5% at 2 years, and 33.5% at 4 years, all relatively lower than those reported in Western studies. This difference in recurrence rates is thought to be attributable to the genetic difference between Asian and Western CD patients,17 and is in line with more serious natural courses in Western CD cohort studies18,19,20,21 showing higher complication and surgery rates compared to those in Korean studies.9,10 Large-scale cohort studies in Korea are crucial to further investigate the natural progress and postoperative recurrence in CD patients for more accurate analyses.
Unlike clinical recurrence, cumulative endoscopic recurrence rates were 42.9% at 1 year and 66.1% at 2 years, results in alignment from those of Western studies. Taking into consideration the fact that endoscopic recurrence precedes clinical recurrence, these outcomes would imply that the postoperative clinical recurrence rate in Korea may increase to the degree seen in Western countries as well. Therefore, the identification of patients at high risk for recurrence and the devising of appropriate preventive measures should gradually emerge as critical issues to clinical physicians. Prophylaxis with mesalazine showed little benefit on preventing postoperative recurrence.22 In a meta-analysis, clinical recurrence rates decreased to 2-24% at 1 year and 1.8-25% at 2 years in thiopurine-treated patients compared to non-thiopurine treated subjects.23 Regarding the effects of biological agents on postoperative recurrence prevention, Yamamoto et al.24 reported that the improvement in inflamed intestinal mucosa almost doubled in the infliximab-treated group as compared to the thiopurine-treated group (75% vs. 38%) postoperatively. Moreover, Savarino et al.25 suggested that clinical recurrence was 12.5% and endoscopic recurrence was 6.3% after the first postoperative year in adalimumab-treated patients and was significantly lower than clinical and endoscopic recurrence rates observed for the thiopurine- or 5-ASA-treated group. Therefore, the use of an immunomodulator is thought to be crucial for the prevention of postoperative recurrence, although further investigation is required.
Although there are some limitations such as single-center retrospective design, relatively small sample size and short follow-up period, current study is unique as the first Korean study to examine both clinical and endoscopic recurrence rates and risk factors in CD patients who underwent bowel resection.
In conclusion, postoperative recurrence of CD is common in Korea, and endoscopic recurrence rates are comparable to those detected in Western studies. For the prevention of postoperative recurrence in patients with CD, identifying patients at high risk for recurrence and adequate surveillance and medication management are crucial. In addition, postoperative immunomodulator therapy may be useful in preventing postoperative recurrence.
References
1. Peyrin-Biroulet L, Loftus EV Jr, Colombel JF, Sandborn WJ. The natural history of adult Crohn's disease in population-based cohorts. Am J Gastroenterol. 2010; 105:289–297. PMID: 19861953.

2. Khoury W, Strong SA, Fazio VW, Kiran RP. Factors associated with operative recurrence early after resection for Crohn's disease. J Gastrointest Surg. 2011; 15:1354–1360. PMID: 21626229.

3. Li Y, Zhu W, Zuo L, et al. Frequency and risk factors of postoperative recurrence of Crohn's disease after intestinal resection in the Chinese population. J Gastrointest Surg. 2012; 16:1539–1547. PMID: 22555673.

4. Gao X, Yang RP, Chen MH, et al. Risk factors for surgery and postoperative recurrence: analysis of a south China cohort with Crohn's disease. Scand J Gastroenterol. 2012; 47:1181–1191. PMID: 22845663.

5. De Cruz P, Kamm MA, Prideaux L, Allen PB, Desmond PV. Postoperative recurrent luminal Crohn's disease: a systematic review. Inflamm Bowel Dis. 2012; 18:758–777. PMID: 21830279.

6. Spinelli A, Sacchi M, Fiorino G, Danese S, Montorsi M. Risk of postoperative recurrence and postoperative management of Crohn's disease. World J Gastroenterol. 2011; 17:3213–3219. PMID: 21912470.
7. Caprilli R, Gassull MA, Escher JC, et al. European evidence based consensus on the diagnosis and management of Crohn's disease: special situations. Gut. 2006; 55(Suppl 1):i36–i58. PMID: 16481630.

8. Regueiro M. Management and prevention of postoperative Crohn's disease. Inflamm Bowel Dis. 2009; 15:1583–1590. PMID: 19322907.

9. Hong DH, Yu CS, Kim DD, et al. Postoperative complications and recurrence in patients with Crohn's disease. J Korean Soc Coloproctol. 2008; 24:13–19.

10. Lee KY, Yu CS, Cho YB, et al. Risk factors for repeat abdominal surgery in Korean patients with Crohn's disease: a multi-center study of a Korean inflammatory bowel disease study group. J Korean Soc Coloproctol. 2012; 28:188–194. PMID: 22993704.

11. Ye BD, Jang BI, Jeen YT, Lee KM, Kim JS, Yang SK. Diagnostic guideline of Crohn's disease. Korean J Gastroenterol. 2009; 53:161–176. PMID: 19835218.
12. Caprilli R, Andreoli A, Capurso L, et al. Gruppo Italiano per lo Studio del Colon e del Retto (GISC). Oral mesalazine (5-aminosalicylic acid; Asacol) for the prevention of post-operative recurrence of Crohn's disease. Aliment Pharmacol Ther. 1994; 8:35–43. PMID: 8186345.

13. Rutgeerts P, Geboes K, Vantrappen G, Beyls J, Kerremans R, Hiele M. Predictability of the postoperative course of Crohn's disease. Gastroenterology. 1990; 99:956–963. PMID: 2394349.

14. Ng SC, Lied GA, Arebi N, Phillips RK, Kamm MA. Clinical and surgical recurrence of Crohn's disease after ileocolonic resection in a specialist unit. Eur J Gastroenterol Hepatol. 2009; 21:551–557. PMID: 19182680.

15. Buisson A, Chevaux JB, Allen PB, Bommelaer G, Peyrin-Biroulet L. Review article: the natural history of postoperative Crohn's disease recurrence. Aliment Pharmacol Ther. 2012; 35:625–633. PMID: 22313322.

16. Reese GE, Nanidis T, Borysiewicz C, Yamamoto T, Orchard T, Tekkis PP. The effect of smoking after surgery for Crohn's disease: a meta-analysis of observational studies. Int J Colorectal Dis. 2008; 23:1213–1221. PMID: 18762954.

17. Kim ES, Kim WH. Inflammatory bowel disease in Korea: epidemiological, genomic, clinical, and therapeutic characteristics. Gut Liver. 2010; 4:1–14. PMID: 20479907.

18. Solberg IC, Vatn MH, Hoie O, et al. Clinical course in Crohn's disease: results of a Norwegian population-based ten-year follow-up study. Clin Gastroenterol Hepatol. 2007; 5:1430–1438. PMID: 18054751.

19. Hovde Ø, Kempski-Monstad I, Smastuen MC, et al. Mortality and causes of death in Crohn's disease: results from 20 years of follow-up in the IBSEN study. Gut. 2013; doi:10.1136/gutjnl-2013-304766. Published online ahead of print 6 June 2013.
20. Kappelman MD, Farkas DK, Long MD, et al. Risk of cancer in patients with inflammatory bowel diseases: a nationwide population-based cohort study with 30 years of follow-up evaluation. Clin Gastroenterol Hepatol. 2014; 12:265–273. PMID: 23602821.
21. Tottrup A, Erichsen R, Svaerke C, Laurberg S, Srensen HT. Thirty-day mortality after elective and emergency total colectomy in Danish patients with inflammatory bowel disease: a population-based nationwide cohort study. BMJ Open. 2012; 2:e000823.

22. Rutgeerts P. Little benefit from mesalazine taken prophylactically after surgery for Crohn's disease. Gut. 2001; 48:452–453. PMID: 11247886.

23. Peyrin-Biroulet L, Deltenre P, Ardizzone S, et al. Azathioprine and 6-mercaptopurine for the prevention of postoperative recurrence in Crohn's disease: a meta-analysis. Am J Gastroenterol. 2009; 104:2089–2096. PMID: 19568226.

24. Yamamoto T, Umegae S, Matsumoto K. Impact of infliximab therapy after early endoscopic recurrence following ileocolonic resection of Crohn's disease: a prospective pilot study. Inflamm Bowel Dis. 2009; 15:1460–1466. PMID: 19266566.

25. Savarino E, Bodini G, Dulbecco P, et al. Adalimumab is more effective than azathioprine and mesalamine at preventing postoperative recurrence of Crohn's disease: a randomized controlled trial. Am J Gastroenterol. 2013; 108:1731–1742. PMID: 24019080.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download