Abstract
Nearly 80% of patients with Crohn's disease (CD) require surgical treatment for complications or failure of medical management. We managed a 31-year-old man with CD who presented with a post-operative fistula. The patient had undergone surgery due to multiple strictures and a fistula. However, a new fistula developed that connected to the intraperitoneal abscess. Intravenous antibiotics were started and multiple percutaneous drainage tubes were inserted to treat the abdominal abscess. However, the amount of drainage was consistently high, even one month after the operation. To treat the postoperative fistula, 5 mg/kg of infliximab was started, and the amount of drainage decreased dramatically to less than 10 cc a day. Some studies have reported that infliximab decreases the recurrence of CD after surgery. The effect of infliximab on post-operative fistulas in patients with CD has not been sufficiently studied. Our results indicated that the use of infliximab to treat post-operative fistula should be explored further in future clinical studies.
Crohn's disease (CD) is a chronic IBD that can involve any part of the gastrointestinal tract. Nearly 80% of patients with CD require surgical treatment for complications or failure of medical management.1 However, patients with CD tend to have a high incidence of postoperative complications, including anastomotic leakages, fistulas, bowel obstructions, and wound infections,2 These complications are directly related to mortality rates. One study reported that using infliximab decreased CD recurrence after surgery.3 However, the effect of infliximab therapy on postoperative complications of CD, such as fistulas, is unknown. We present the case of a patient with CD who was treated with infliximab for a postoperative fistula.
A 31-year-old man with CD was admitted to the hospital because of severe abdominal pain and diarrhea. He had been diagnosed with CD 10 years previously, but he was lost to follow-up, during which he experienced repeated exacerbations and remissions. The patient had taken mesalazine 3,000 mg/day and azathioprine 50 mg/day and had started infliximab one year prior to admission. With infliximab, the patient experienced immediate relief of diarrhea and abdominal pain, but obstructive symptoms had gradually worsened. He complained of abdominal pain, increased borborygmus, decreased oral intake, and a decrease in body weight. Abdominal CT scan and small bowel series revealed an ileocolic fistula, multiple ulcers, and severe stricture of the small bowel (Fig. 1). Vital signs (blood pressure, 120/80 mmHg; pulse rate, 80 beats/min; respiratory rate, 20 beats/min; body temperature, 36.9℃) were normal. He has a height of 171 cm, a weight of 53 kg, and a BMI of 18.1 kg/m2. The patient had a chronically ill appearance with pale conjunctiva, mild tenderness in the lower abdomen, and accentuated bowel sounds. Liver and spleen were not palpable. Pitting edema could be seen on both lower limbs. Laboratory testing revealed anemia with a hemoglobin level of 8.7 g/dL, leukocyte count of 3,970/mm3, and platelet count of 265,000/mm3. Serum chemistry tests were consistent with severe malnutrition: AST/ALT 53/29 IU/L, BUN/creatinine 15/0.64 mg/dL, total protein/albumin 4.3/2.2 g/dL, and total cholesterol 88 mg/dL. ESR and CRP level were 35 mm/h and 2.1 mg/dL, respectively. Both anti-Saccharomyces cerevisiae-antibodies IgA and IgG were negative, and the patient's CDAI was about 261 points. He had been experiencing approximately 25 liquid stools per week, severe abdominal pain, and a very poor sense of well-being. To improve the patient's condition, wide resection of involved bowel and colostomy would be needed; however, because of a psychological reaction to personal disfigurement and the need to relearn bowel habits, he strongly refused colostomy. Therefore, we decided to perform a small and large bowel segmental resection and primary repair.
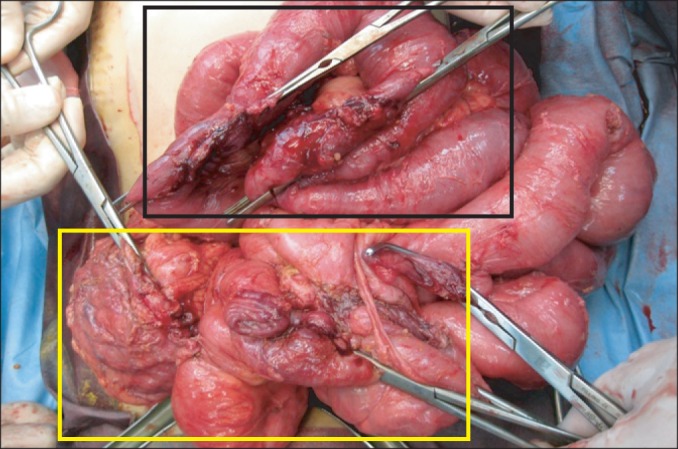
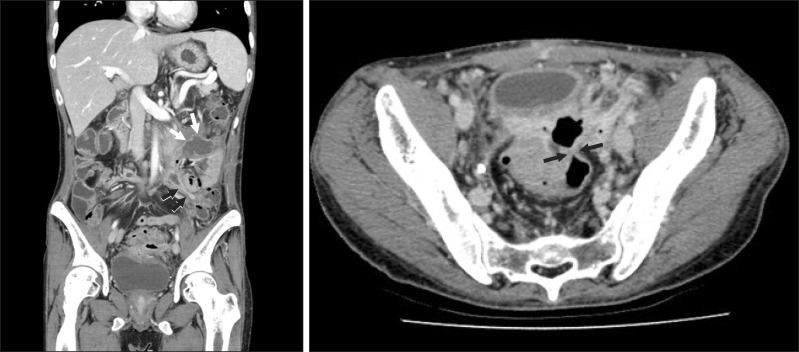
Gross findings during surgery included an abscess connected to the terminal ileum, bladder adhesion, a jejuno-sigmoid fistula, and huge inflammatory masses. An ileocecectomy, jejunal resection, and sigmoid colon resection were performed, followed by primary repair of the jejunum, rectum, and sigmoid colon (Fig. 2). Fortunately, 220 cm of the small bowel remained after surgery. However, one week postoperatively, the patient developed a high fever and abdominal pain. Abdominal CT scan revealed a fistula connected to an intraperitoneal abscess (Fig. 3). The patient was started on intravenous antibiotics, and the abscess was drained percutaneously. A total of four percutaneous drainages were performed. The drainage fluid was dark yellow and highly viscous but gradually cleared after continuous use of antibiotics. However, despite no further evidence of infection (white blood cell count 4,270/mm3 and CRP 0.3 mg/dL), approximately 30-50 cc of fluid issued from every drain daily, even one month after the operation.
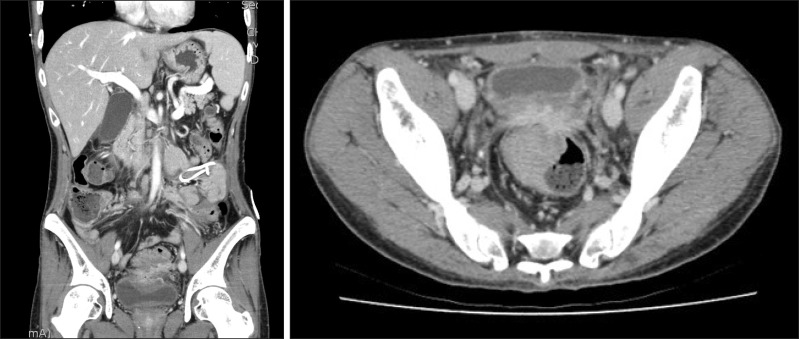
The patient was started on 5 mg/kg of infliximab to treat the postoperative fistula and prevent a recurrence. After infliximab therapy was initiated, drainage decreased dramatically to less than 10 cc a day. In follow-up abdominal CT scans, the abscess in the abdominal cavity and the postoperative fistula disappeared (Fig. 4). The percutaneous drainages were consecutively removed, the patient began receiving oral nutrition, and the intravenous antibiotics were stopped. The patient quit smoking, and infliximab was injected to prevent disease recurrence. Three months after surgery, the patient looked healthy and reported passing stools once or twice a day. His body weight increased by 8 kg, BMI increased to 20.9 kg/m2, and his CDAI decreased to 60. In follow-up laboratory exams, the patient's hemoglobin level was 12.7 g/dL, total protein and albumin were 6.9/3.9 g/dL, and total cholesterol was 130 mg/dL.
Even though advances have been made in the medical care of patients with CD, about 80% of patients with CD undergo several operations in their lifetimes.4 However, these patients have a high rate of complications after surgery (6-45%) due to the presence of abscesses in the abdominal cavity, obstruction, malnutrition, and chronic steroid use. They usually require multiple anastomoses, which results in higher mortality rates (0.5-5.5%) due to complications as compared to patients without CD.5-7 Complications from surgery include wound infections, anastomotic leakages, fistulas, anastomotic site strictures, and sepsis in the pelvis.
Fistulas are relatively frequent postoperative complications in patients with CD, but the underlying mechanism of fistula formation has not yet been determined. In patients with CD, fistulas are generally related to deep mucosal ulcers characterized by transmural inflammation. To repair the mucosal defect, epithelial cells migrate from the ulcer wall into the ulcer base. For faster migration, epithelial cells undergo epithelial-mesenchymal cell transition and develop a mesenchymal cell-like phenotype with loose cell-to-cell contacts that finally penetrate into deep layers of the bowel wall.8 Lamina propria fibroblasts in the mucosa of patients with CD have reduced migratory potential and might therefore, not be able to migrate successfully to the tissue defect. However, different mechanisms may be involved in each fistula type, and each fistula type may respond differently to infliximab treatment. For example, internal fistulas usually occur immediately proximal to the stricture and wall thickening, causing high intraluminal pressure with distension and increased wall tension of the prestenotic bowel segments. Fistulas formed by these mechanisms may react less to anti-inflammatory agents due to fixed fibrotic tissues and muscular hyperplasia.9
Infliximab is a widely used monoclonal antibody against tumor necrosis factor α that seems to be effective for treating fistulas in patients with CD. There is some dispute as to whether infliximab use preoperatively increases the risk of postoperative complications. Appau et al. reported that infliximab use within 3 months prior to surgery is associated with increased postoperative sepsis, abscess, and readmissions in patients with CD.10 Marchal et al. found no significant difference between patients who received infliximab before surgery and those who did not, based on the occurrence of complications and the period of hospitalization.11 The effect of infliximab on postoperative fistulas in patients with CD has not been studied sufficiently. Endoscopic recurrence rates after surgery have been reported to be 65-90% in the first 12 months, 80-100% in the first 3 years, and 20-25% every year after ileocecal resection.12 Some studies have reported that using infliximab after surgery was effective in preventing CD recurrence.13-16 Sorrentino et al. performed a prospective cohort study of 12 consecutive patients who were treated immediately after surgery with maintenance infliximab (5 mg/kg). Three years after surgery, none of the patients had clinical or endoscopic evidence of CD recurrence. However, discontinuation of infliximab resulted in endoscopic recurrence after 4 months in 10 of the 12 patients (83%).13 Furthermore, Regueiro et al. reported a one-year, randomized, double-blind, placebo-controlled trial of 24 patients who had undergone ileocolonic resection and found that the endoscopic recurrence rate of the patient group managed with 5 mg/kg of infliximab (9.1%) was significantly lower than that of the placebo group (84.6%).14 Moreover, the histological recurrence rate in the infliximab group (27.3%) was lower than that in the placebo group (84.6%). However, no large-scale, randomized, controlled studies that have followed patients for an extended period have been reported. Our case of successful treatment of a patient with CD with infliximab to resolve a postoperative fistula indicates that this is a promising treatment option for postoperative fistulas.
In Korea, the incidence and prevalence of IBD are increasing rapidly. Although the incidence is still low compared to Western countries, the mean annual incidence rate of CD per 100,000 inhabitants was 0.53 in Seoul for a 20-year period.16 The number of operations performed is expected to increase in the future. Therefore, additional clinical studies on the role of infliximab in treating postoperative fistulas in patients with CD are required.
References
1. Olaison G, Sjodahl R, Tagesson C. Glucocorticoid treatment in ileal Crohn's disease: relief of symptoms but not of endoscopically viewed inflammation. Gut. 1990; 31:325–328. PMID: 2323598.
2. Gardiner KR, Dasari BV. Operative management of small bowel Crohn's disease. Surg Clin North Am. 2007; 87:587–610. PMID: 17560414.

3. Yamamoto T. Factors affecting recurrence after surgery for Crohn's disease. World J Gastroenterol. 2005; 11:3971–3979. PMID: 15996018.

4. Thia KT, Loftus EV Jr, Sandborn WJ, Yang SK. An update on the epidemiology of inflammatory bowel disease in Asia. Am J Gastroenterol. 2008; 103:3167–3182. PMID: 19086963.

5. Lindhagen T, Ekelund G, Leandoer L, Hildell J, Lindstrom C, Wenckert A. Pre- and post-operative complications in Crohn's disease with special reference to duration of preoperative disease history. Scand J Gastroenterol. 1984; 19:194–203. PMID: 6719032.

6. Post S, Betzler M, von Ditfurth B, Schurmann G, Kuppers P, Herfarth C. Risks of intestinal anastomoses in Crohn's disease. Ann Surg. 1991; 213:37–42. PMID: 1985536.
7. Subramanian V, Saxena S, Kang JY, Pollok RC. Preoperative steroid use and risk of postoperative complications in patients with inflammatory bowel disease undergoing abdominal surgery. Am J Gastroenterol. 2008; 103:2373–2381. PMID: 18616660.

8. Nielsen OH, Rogler G, Hahnloser D, Thomsen OØ. Diagnosis and management of fistulizing Crohn's disease. Nat Clin Pract Gastroenterol Hepatol. 2009; 6:92–106. PMID: 19153563.

9. Miehsler W, Reinisch W, Kazemi-Shirazi L, et al. Infliximab: lack of efficacy on perforating complications in Crohn's disease. Inflamm Bowel Dis. 2004; 10:36–40. PMID: 15058525.
10. Appau KA, Fazio VW, Shen B, et al. Use of infliximab within 3 months of ileocolonic resection is associated with adverse postoperative outcomes in Crohn's patients. J Gastrointest Surg. 2008; 12:1738–1744. PMID: 18709420.

11. Marchal L, D'Haens G, Van Assche G, et al. The risk of post-operative complications associated with infliximab therapy for Crohn's disease: a controlled cohort study. Aliment Pharmacol Ther. 2004; 19:749–754. PMID: 15043515.
12. Ye BD, Yang SK, Shin SJ, et al. Guidelines for the management of Crohn's disease. Intest Res. 2012; 10:26–66.

13. Sorrentino D, Paviotti A, Terrosu G, Avellini C, Geraci M, Zarifi D. Low-dose maintenance therapy with infliximab prevents postsurgical recurrence of Crohn's disease. Clin Gastroenterol Hepatol. 2010; 8:591–599.e1. PMID: 20139033.

14. Regueiro M, Schraut W, Baidoo L, et al. Infliximab prevents Crohn's disease recurrence after ileal resection. Gastroenterology. 2009; 136:441–450.e1. PMID: 19109962.

15. Sorrentino D, Terrosu G, Avellini C, Beltrami CA, Bresadola V, Toso F. Prevention of postoperative recurrence of Crohn's disease by infliximab. Eur J Gastroenterol Hepatol. 2006; 18:457–459. PMID: 16538123.

16. Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008; 14:542–549. PMID: 17941073.
Fig. 1
Small bowel series (A) and abdominal CT scan (B) findings. They revealed ileocolic fistulas (arrows), multiple small bowel stenosis, and dilated small bowel loops with abundant fecal material.
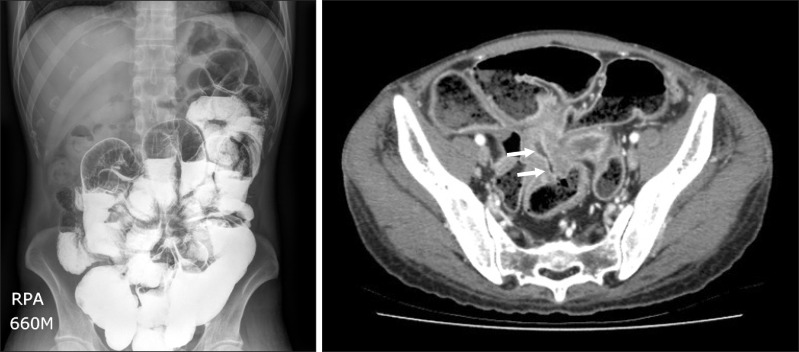
Fig. 2
Gross findings during surgery. Ileocecectomy, rectal repair (yellow square), and small bowel and sigmoid resection (black square) were performed.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download