Abstract
Crohn's disease (CD) may involve any part of the gastrointestinal tract, from the mouth to the anus. Approximately >90% of cases occur in the small bowel and colon. Upper gastrointestinal involvement, especially duodenal manifestation, is relatively rare. Therefore, adequate medical treatment for duodenal CD has not yet been established. We report a case of CD with duodenal involvement. A 46-year-old man with Crohn's ileocolitis presented to our hospital with right upper quadrant pain. An endoscopy showed a deep excavated ulcer with deformity at the duodenal bulb, and he was initially treated with azathioprine (1 mg/kg), Pentasa (3.0 g/day), and a proton pump inhibitor for 1 year. However, the deep ulcer did not heal. Therefore, infliximab infusion therapy was initiated, and the duodenal lesion completely resolved on follow-up esophagogastroduodenoscopy. We report a case of duodenal CD that completely resolved following infliximab infusion, with a review of the literature.
Crohn's disease (CD) is defined as the immune-mediated chronic intestinal disorder characterized by non-caseating granuloma and transmural inflammation of unknown etiology.1 Although it may develop anywhere in the gastrointestinal tract, from the mouth to the anus, the most frequent presentation involves the terminal ileum and colon.2 In addition, upper gastrointestinal involvement of CD is relatively infrequent (0.4-3%);3 duodenal involvement is especially rare.2 Hence, medical treatment for duodenal CD has not yet been well documented. According to previous reports, high-dose proton pump inhibitors (PPI), mesalazine, and steroids have been used in similar cases.4 Recently, infliximab, a chimeric monoclonal tumor necrosis factor (TNF)-α antibody, has been used in the management of duodenal CD. We report a case of duodenal CD that was completely resolved with infliximab treatment with a review of the literature.
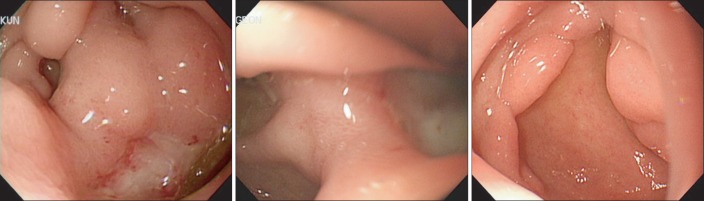
A 46-year-old male patient was admitted to Eulji medical center on November 9, 2009, with a 2-day history of aggravating right upper quadrant pain. The patient's medical history showed that he underwent right hemicolectomy for generalized peritonitis in 1999. Previous pathologic findings included small ulcers, mucosal necrosis, and fissures in both the ileum and right colon. In addition, small granulomas and infiltrations of chronic inflammatory cells were seen in the submusocal, muscular, and serosal layers. Based on the pathologic findings, the patient was diagnosed with CD and treated with Pentasa (3.0 g/day) and intermittent oral steroid for active disease control. In 2006, a colonoscopy showed a cobble stone appearance and partial stenosis at the anastomosis site (Fig. 1A, B). The patient underwent a segmental resection for small bowel stricture in 2007. Subsequently, he was treated with azathioprine (1 mg/kg) and Pentasa (3.0 g/day). On November 14, 2008, he complained of severe epigastric pain. Esophagogastroduodenoscopy showed a deep excavated ulcer in the first duodenal portion (Fig. 2A). Neither granuloma nor Helicobacter pylori (H. pylori) were present on biopsy. PPI treatment was administered for 1 year.
Vital signs were measured at admission, and his blood pressure was 100/60 mmHg, pulse rate was 70 beats/min, respiratory rate was 20 breaths/min, and body temperature was 36.8℃. Physical examination showed mild tenderness on the right upper quadrant with normoactive bowel sound. The laboratory findings revealed a white blood cell count of 2,930/mm3, a hemoglobin level of 11.2 g/dL, and a platelet count of 290,000/mm3. AST level was 19 IU/L, ALT level was 11 IU/L, ALP level was 58 IU/L, amylase level was 79 IU/L, and lipase level was 22 IU/L. BUN level was 14.1 mg/dL, serum creatinine level was 1.0 mg/dL, ESR was 14 mm/h, and CRP level was 1.29 mg/dL.
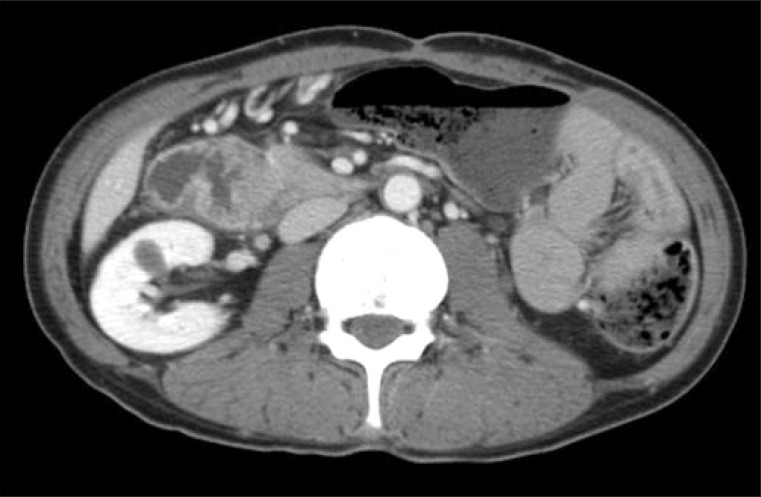
Abdominal CT showed aggravated segmental thickening in the small bowel and ulcer deformity in the duodenum (Fig. 3). The CDAI score was 411. We performed a follow-up endoscopy and that revealed an aggravated duodenal ulcer with partial stenosis (Fig. 2B).
As the patient had previously been treated with azathioprine, Pentasa, and PPI for >1 year, we decided to administer infliximab infusion to treat the aggravated multiple small bowel ulcers and refractory duodenal ulcer. Infliximab was infused (5 mg/kg) on weeks 0, 2, and 6, and follow-up endoscopy showed a decrease in the size and improvement in the depth of the duodenal ulcers, furthermore, the patient did not complain of any abdominal pain. The CDAI score improved to 196.
During regular check-ups at the outpatient department, the patient received an infliximab injection after every 8 weeks. In November 2010, after the eight injection of infliximab, complete resolution of the duodenal ulcer was observed on endoscopy (Fig. 2C), without fistula or stenosis. The patient was followed up with infliximab maintenance therapy, with no abdominal pain.
Duodenal CD is rare and usually progresses to involve extraduodenal organs such as the pancreas or esophagus.5,6 Common presentations of duodenal CD include upper abdominal or epigastric pain and vomiting caused by gastroduodenal obstruction.2 Additionally, weight loss or upper gastro-intestinal bleeding could occur.7 Our patient presented with chronic right upper quadrant pain and mild anemia, without gastric outlet obstruction or bleeding. The gastroduodenoscopy showed that the involved mucosa had a diffuse granular appearance with nodularity and ulcerations, accompanied by a lack of antral and duodenal distensibility.2,8 Occasionally, various degrees of stenosis or marked stricture formation can be observed. Histological presentations include acute and chronic inflammation and fibrosis involving the entire duodenal wall;2,7,8 non-caseating granulomas may be present in any layer of the wall or in the regional lymph nodes.7 In a prospective study9 involving 41 patients with CD, aphthoid erosions, ulcers, thickening of folds, and duodenal stenosis were observed on endoscopy, and granulomas were reported in approximately 19.5% of the biopsy specimens. In our patient, there was a deep excavated ulcer with partial stenosis and bulb deformity in the duodenum. The biopsy indicated acute and chronic inflammation without granuloma or H. pylori.
An initial management strategy for duodenal CD includes treatment with sulfasalazine or 6-ercaptopurine.2,8 In addition, for managing duodenal ulcers, a regimen of corticosteroids and histamine 2 (H2) receptor blockers or PPI is most commonly used.2 In a study of patients with non-obstructing duodenal CD who were treated with corticosteroids at the Lahey Clinic, some patients showed a favorable response.10 However, other studies have reported that treatment using corticosteroids and H2 receptor blockers or PPI was ineffective, and the involved lesion required surgical treatment such as gastrojejunal bypass because of complications and intractable pain.2,11 Many clinicians have reported refractory duodenal Crohn's cases that required invasive treatment following the failure of various pharmaceutical treatment attempts,11,12 and more than one-third of affected patients required surgical procedures.2
After the diagnosis of duodenal ulcer, our patient had taken PPI for 1 year. His symptoms and radiologic and endoscopic findings worsened. Similar to other reports, long-term medical treatment13 with PPI, azathioprine, and mesalazine did not induce mucosal healing.
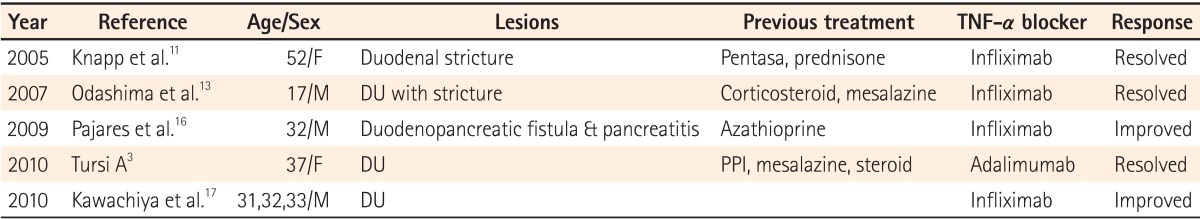
In accordance with the previous literature, infliximab, is not only effective in moderate to severe active fistulizing CD,13,14 but also in refractory luminal inflammation.15 Although the Belgian Inflammatory Bowel Disease Research Group confirmed that a good response often results from the infliximab infusion therapy in fistulizing or refractory CD, the trial and result of infliximab treatment in duodenal CD was not sufficient. Only a few studies have investigated the efficacy of infliximab treatment for refractory duodenal CD, and reported the resolution of duodenal ulcers using infliximab with or without complications (Table 1). Based on these reports, we treated our patient with an anti-TNF-α antibody, infliximab, and noted complete resolution of the intractable duodenal ulcer on follow-up endoscopy following the eight infliximab infusion, without any complication. Other studies and our case suggest that infliximab may be effective in the management of duodenal CD refractory to other medical treatment. We hope that our case can be helpful in managing duodenal CD. Further large-scale studies are required before infliximab can be used for the management of duodenal CD to reduce serious complications and the need for surgery.
References
1. Targan SR, Hanauer SB, van Deventer SJ, et al. Crohn's Disease cA2 Study Group. A short-term study of chimeric monoclonal antibody cA2 to tumor necrosis factor alpha for Crohn's disease. N Engl J Med. 1997; 337:1029–1035. PMID: 9321530.

2. Kimmins MH, Billingham RP. Duodenal Crohn's disease. Tech Coloproctol. 2001; 5:9–12. PMID: 11793253.

3. Tursi A. Duodenal Crohn's disease successfully treated with adalimumab. Endoscopy. 2011; 43(Suppl 2 UCTN):E22. PMID: 21271523.

4. Dignass A, Van Assche G, Lindsay JO, et al. The second European evidence-based consensus on the diagnosis and management of Crohn's disease: current management. J Crohns Colitis. 2010; 4:28–62. PMID: 21122489.

5. Gschwantler M, Kogelbauer G, Klose W, Bibus B, Tscholakoff D, Weiss W. The pancreas as a site of granulomatous inflammation in Crohn's disease. Gastroenterology. 1995; 108:1246–1249. PMID: 7698591.

6. Moribata K, Kato J, Iimura S, et al. Mucosal healing of esophageal involvement of Crohn's disease with granulocyte/monocyte adsorption. J Clin Apher. 2011; 26:225–227. PMID: 21786316.

7. Nugent FW, Richmond M, Park SK. Crohn's disease of the duodenum. Gut. 1977; 18:115–120. PMID: 856671.
8. Ando T, Nobata K, Watanabe O, et al. Abnormalities in the upper gastrointestinal tract in inflammatory bowel disease. Inflammopharmacology. 2007; 15:101–104. PMID: 17464554.

9. Alcantara M, Rodriguez R, Potenciano JL, Carrobles JL, Munoz C, Gomez R. Endoscopic and bioptic findings in the upper gastrointestinal tract in patients with Crohn's disease. Endoscopy. 1993; 25:282–286. PMID: 8330547.

10. Nugent FW, Roy MA. Duodenal Crohn's disease: an analysis of 89 cases. Am J Gastroenterol. 1989; 84:249–254. PMID: 2919581.
11. Knapp AB, Mirsky FJ, Dillon EH, Korelitz BI. Successful infliximab therapy for a duodenal stricture caused by Crohn's disease. Inflamm Bowel Dis. 2005; 11:1123–1125. PMID: 16306777.

12. Gonzalez M, Collaud S, Gervaz P, Frossard JL, Morel P. Surgical treatment of duodenal stenosis in Crohn's disease. Ann Chir. 2006; 131:636–638. PMID: 16836971.
13. Odashima M, Otaka M, Jin M, et al. Successful treatment of refractory duodenal Crohn's disease with infliximab. Dig Dis Sci. 2007; 52:31–32. PMID: 17171444.

14. Present DH, Rutgeerts P, Targan S, et al. Infliximab for the treatment of fistulas in patients with Crohn's disease. N Engl J Med. 1999; 340:1398–1405. PMID: 10228190.

15. Ferrante M, D'Haens G, Dewit O, et al. Efficacy of infliximab in refractory pouchitis and Crohn's disease-related complications of the pouch: a Belgian case series. Inflamm Bowel Dis. 2010; 16:243–249. PMID: 19637335.

16. Pajares JA, Hernandez L, Menchen P, Menchen L. Duodenopancreatic fistula complicating upper gastrointestinal Crohn's disease: successful treatment with infliximab. Am J Gastroenterol. 2009; 104:1863–1864. PMID: 19436276.

17. Kawachiya T, Hara J, Hirata N, Mashimo M, Arakawa T. Successful treatment of duodenal Crohn disease with infliximab: report of 3 cases. Nihon Shokakibyo Gakkai Zasshi. 2010; 107:1933–1940. PMID: 21139362.
Fig. 1
Endoscopic and histopathologic findings of the distal ileum. (A) Endoscopic findings of the distal ileum. A cobble stone appearance on the ileal side of the ileocolostomy site. (B) Non-caseating granuloma seen on biopsy (H&E stain, ×200).
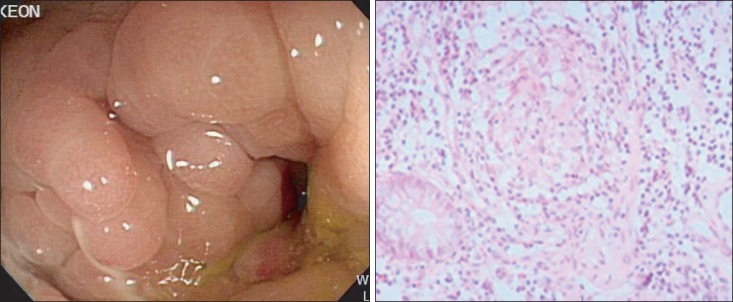
Fig. 2
Endoscopic findings of the duodenum. (A) At initial diagnosis, an active ulcer with bulb deformity is found. (B) After 1 year of proton pump inhibitor treatment, an aggravating deep ulcer with partial stenosis is seen at the superior duodenal angle. (C) After the eight injections of infliximab, complete resolution of the duodenal ulcer is seen with good passage to the second part of duodenum.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download