Abstract
Background/Aims
Inflammatory bowel disease (IBD) is a chronic disabling gastrointestinal disorder that diminishes the quality of life of the affected individuals. Limited data are available regarding the impact of IBD on the daily life of Koreans.
Methods
Self-administered, computer-aided, internet-based questionnaires were distributed to members of a Korean patient organization for IBD from March to April 2013, by the Korean Association for the Study of Intestinal Diseases.
Results
A total of 599 patients with IBD (387 with Crohn's disease [CD] and 212 with ulcerative colitis [UC]) were enrolled. The majority of patients (81%) expressed feelings of fatigue, weakness, and being worn out in their daily lives during times of flare; this percentage was reduced to 61% during remission. Respondents were absent from work or school for an average period of 18 days because of illness, within the first 6 months; the majority of respondents (64%) felt stressed about their absence. Forty-six percent of the respondents reported having received unfair comments at work, or having suffered discrimination. Forty-seven percent of the respondents felt that IBD had negatively affected their income and earnings. Compared with patients with UC, those with CD reported a more frequent negative impact of IBD on work, or more economic burden. More than half of the respondents (61%) reported that IBD had prevented them from making or keeping friends.
Although the incidence rate of IBD in Asian countries is considerably lower than the rate in Western countries, the burden of IBD has been rapidly increasing in Korea.123 However, public awareness about IBD is still low in Korea. Delay in the diagnosis of IBD could delay therapy, which can worsen the outcome.4567
IBD mainly consists of UC and CD. These are chronic disabling gastrointestinal disorders that diminish the quality of life (QOL) of the patient.58910 Patients with IBD more frequently receive disability allowances than those received by age-matched individuals from the general population,5610 which proves the detrimental effects of IBD on healthrelated QOL and productivity.58 A recent large-scale study (comprising 4,670 patients with IBD from 25 countries) conducted by the European Federation of Crohn's and Ulcerative Colitis Associations (EFCCA) reported the detrimental effects of IBD on intimate relationships, and the unfair comments received by the patients with regard to their work performance. 8
However, limited studies have assessed the impact of IBD on the life of patients in Korea, with the majority of studies having been conducted in Western cohorts.568910 In addition, there is little public knowledge regarding IBD and the chronic suffering of patients in Korea.
To overcome these issues, the Korean Association for the Study of Intestinal Diseases (KASID) has been conducting the “Happy Bowel Campaign” since 2013 to raise public awareness of IBD in general and to provide accurate information regarding the importance of early diagnosis and proper treatment to patients with IBD. In addition, the KASID is a promoter of World IBD Day, held every year on May 19.
This study reports the findings of a KASID-sponsored survey that aimed to investigate the impact of IBD on the daily lives of patients in Korea.
Patients with UC or CD were enrolled. Self-administered, computer-aided, internet-based questionnaires were distributed to them by the KASID, from March to April 2013. The KASID advertised the study through the Korean IBD patient advocacy and support group newsletter and website, and through online advertisements during the Happy Bowel Campaign. The purpose of the study was explained to patients at the time of enrollment. The survey was anonymous and the data were analyzed without revealing the personal details of the patients. Patients who had no Internet access were excluded, since the survey was only available online. Responding to the survey questions was considered consent to participate.
The survey was designed by KASID members of the International Affairs Committee Secretary of Liaison & Public Relations in cooperation with a communications company “Communication Works.” The survey was based primarily on the IMPACT survey of the EFCCA and on previously published reports8 on the QOL of patients with IBD. The survey consisted of 68 questions divided into 6 categories: (1) demographics, (2) experience with IBD, (3) overall impact on life, (4) overall impact on work, (5) overall economic impact, and (6) impact on relationships (Supplementary Material 1).
Some questions regarding “flare” and “remission” were short-answer questions. Most questions were closed ended, and participants were allowed to select one applicable option. The extent of “flare” and “remission” was open to patient interpretation. The questions concerning the overall impact of IBD were measured using a 5-point Likert scale (strongly agree, 5; agree, 4; neither agree nor disagree, 3; disagree, 2; strongly disagree, 1). In these cases, disagree or strongly disagree represented “no” and the other responses represented “yes.”
The collected data were analyzed using SPSS for Windows version 22.0 statistical software (IBM Corp., Armonk, NY, USA). With regard to statistical accuracy, a range of ±2.53% (95% CI limits) was set. Descriptive statistics and multiple linear regression analysis were used to analyze the responses, with subanalyses of patients with CD and UC. Subgroup differences were calculated using the chi-square test.
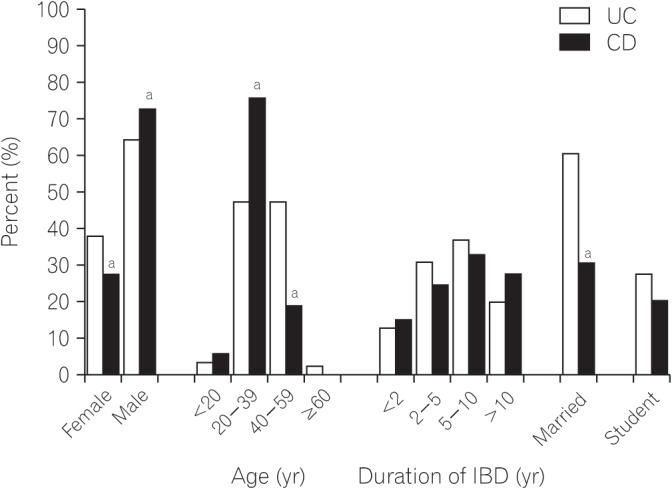
A total of 599 patients with IBD (387 [64.6%] with CD and 212 [35.4%] with UC) completed the survey. Demographic and baseline data for all respondents are shown in Fig. 1. The majority of respondents were male (69.6%) in both the CD and UC subgroups. The majority of participants (59%) reported a period of more than 5 years since the diagnosis of IBD (60% of the patients in the CD subgroup and 57% of the patients in the UC subgroup).
Most respondents (84%) from the CD and UC groups reported IBD being chronically active, whereas 16% reported being in remission. Sixty-five percent of the patients had been admitted to a hospital for IBD within the 5 years preceding the study; however, the proportion of patients with CD was significantly higher than the proportion of patients with UC (76%, P <0.001), with regard to the hospitalization. Thirty-eight percent of the patients received emergency care before being diagnosed with IBD. Eighteen percent of the respondents had experienced a surgical procedure because of IBD. More patients with CD than with UC reported this experience (P <0.001) (Table 1).
Forty-one percent of the respondents reported visiting a hospital 6 months after they noticed the first symptoms related to IBD. The time before the first hospital visit was significantly longer in patients with CD (P <0.001). The reasons for delayed hospital visit were lack of knowledge about IBD (75%), mild symptoms (13%), inconvenient hospital access (3%), economic burden (3%), and others (6%). Most respondents (75%) received a final diagnosis within a year after they first noticed the symptoms. The other 25% patients received a final diagnosis after more than a year; in 3% of these, IBD was diagnosed after 5 years from their first symptoms. The time required for final diagnosis was also significantly longer in patients with CD (P <0.001) (Table 1).
About three-quarters of the respondents reported undergoing current treatment by a gastroenterologist (75%), while 13% reported undergoing current treatment by a primary physician. The most commonly taken drug among the respondents was 5-aminosalicylates (69%), followed by immunosuppressive agents (48%), corticosteroids (15%), and biological drugs (11%). More patients with CD than with UC were being treated with biological drugs (15% and 5%, respectively) at the time of conducting the study. Sixty-one percent of the patients had experienced side effects from corticosteroids, and 87% of the patients were concerned about the long-term effects of corticosteroids.
The majority of patients (81%) expressed feelings of fatigue, weakness, and being worn out in their daily lives during times of flare; this percentage was reduced to 61% during remission. Most patients (68%) felt stressed and were psychologically affected even during remission. Thirty-seven percent of the patients reported that they felt like committing suicide (CD 41% vs. UC 30%, P =0.01). Multiple linear regression analysis revealed that previous emergency care (P =0.021), previous hospitalizations (P =0.036), previous surgeries (P =0.035), experience of abdominal pain (P=0.008), and using biologics (P =0.020) were associated with the feeling of committing suicide. Most patients (74%) were anxious about their future (Table 2). Young age (P =0.047), low income (P =0.026), and experience of abdominal pain (P <0.001) were associated with anxiety about the future, as per multivariable regression analysis.
More than half (52%) of the respondents reported absence from work or school because of illness within the past 6 months (mean, 18 days). Younger patients and patients with CD had had more sick days; the mean period absence owing to sickness was 10 days for those >40 years of age and 23 days for those <40 years of age (P <0.001), and 20 days versus 14 days for patients with CD and UC, respectively (P <0.001). The absence from work/school owing to IBD caused stress in 64% of the respondents. Compared to patients with UC, those with CD reported a more frequent negative impact of IBD on work (Table 3). The use of biologics (P =0.007) and steroids (P =0.001), previous hospitalization (P =0.043), previous surgeries (P =0.009), and abdominal pain (P =0.001) were associated with the negative impact of IBD on work, as per multiple linear regression analysis.
Forty-one percent of the respondents reported decreased QOL owing to the economic burden caused by IBD. Twenty-one percent of the respondents had stopped medical treatment because of the economic burden. Those with CD reported an economic burden more often than those with UC (Table 4). Male gender (P =0.001), old age (P =0.011), low income (P =0.008), use of steroids (P =0.039) and biologics (P =0.023), previous hospitalization (P =0.048), and previous surgeries (P =0.002) were associated with high economic burden, as per multivariable regression analysis.
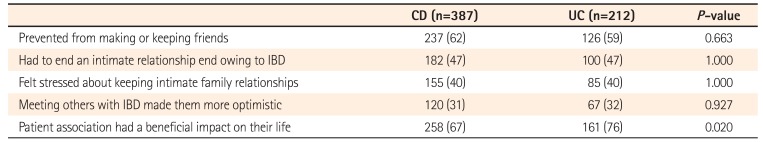
Sixty-one percent of the patients reported that IBD had prevented them from making or keeping friends. Nearly half of the respondents (47%) reported having had to end an intimate relationship owing to IBD. Most of the respondents (70%) reported that the patient association had a beneficial impact on their life (Table 5). Young age (P =0.002), previous surgeries (P =0.003), and previous hospitalization (P =0.038) were associated with the negative impact of IBD on relationships, as per multivariable regression analysis.
IBD is typically diagnosed in childhood or early adulthood, and is a lifelong condition.58910 Although IBD does not reduce life expectancy, it has a substantial impact on health-related QOL.81112 The present study reports the experience of IBD among Korean patients and the impact of IBD on their daily life. Most patients with IBD were tired, weak and worn out in their daily life during a remission as well as during flareups. A large number of patients reported that IBD adversely affected their QOL. This negative impact of IBD was more severe in patients with CD than in those with UC. A previous experience of surgeries, and hospitalization due to IBD were associated with this negative impact. In general, chronic fatigue has been found to be more prevalent in patients with IBD than in healthy subjects,91314 which, in turn, diminishes the health-related QOL in IBD.9 Accordingly, physicians should remember that fatigue is an important symptom of IBD that impacts the health-related QOL of the patients.
In this study, the time from onset of symptoms of IBD to hospital visit was long; over 41% of the patients had been symptomatic for at least 6 months before visiting a clinician. The most common cause of delayed hospital visit was lack of patient's knowledge about the disease. In addition, although most responders reported establishment of a final diagnosis within 12 months after noticing the first symptoms, 25% of the patients waited for more than a year for the final diagnosis. The delay in meeting a specialist and emergency department visit was more striking for patients with CD than for those with UC. Population-based cohort studies reported that one-fifth to one-third of the patients with CD have complications such as stricture, abscess and/or fistula at the time of diagnosis.1516 Functional gastrointestinal disorders such as IBS often mimic early manifestations of IBD, and infectious diseases such as intestinal tuberculosis, which mimic IBD, can hinder accurate assessment of the disease in Korea, thereby delaying hospital visit or referral to IBD specialists.71718 In the IMPACT survey, only 54% of the 4,670 patients received a final diagnosis within 1 year after noticing the first symptoms. About 20% of the patients received a final diagnosis after more than 5 years. The majority of patients (67%) had visited an emergency department at least once before their diagnosis.8 Timely diagnosis and treatment would help reduce the health care burden of hospitals, including prediagnosis hospital visits or admissions.819 Patients with IBD tend to require emergency room or primary clinic care prior to diagnosis; thus, awareness about IBD is necessary among emergency care staff or primary physicians. 8
About 15% of the respondents received corticosteroid therapy, which was a concern for most of them. Corticosteroid use should be consistent with the guidelines, and the advantages and possible detrimental effects should be discussed with patients.8202122
The fluctuations and unpredictable exacerbations of IBD symptoms have a significant psychological impact on the patient's life. Fears related to the long-term effects of treatments, and the progression of the disease can exacerbate anxiety and depression.11232425 In the present study, 37% of the patients reported having felt like committing suicide. Most patients were anxious about their future. The prevalence of anxiety and/or depression in patients with IBD has been reported to be 35% during remission;24 the prevalence of anxiety and depression during relapse has been reported to be 80% and 60%, respectively.25 In a recent study, Korean patients with IBD showed higher levels of depression and impaired health-related QOL than those shown by healthy controls.26 The negative perceptions of IBD among patients and the depressive mood can increase treatment nonadherence, leading to a poorer outcome.19 Integrating psychological interventions with conventional medical treatment seems prudent.11
IBD had a considerable impact on work and economic burden in the present study. Many patients, especially young respondents and those with CD, had missed school or work in the 6 months prior to the study, consistent with other reports,827 which, for many patients, is a source of stress and can be the basis for hurtful comments or employment problems. Accordingly, medical discussions should consider work and economic burden as important facets of treatment among Korean patients with IBD.
With regard to building human relationships, IBD can lead to decreased physical intimacy and social activity.2829 Being able to talk about IBD-related problems in a supportive group setting was helpful for many respondents, as was the awareness created by health care professionals regarding the influence of IBD on these aspects of life.
This study had several limitations. Firstly, the survey was a self-completed instrument and was only available online, so individuals without Internet access could not participate. Thus, the results cannot be generalized to the entire population. Secondly, the survey questionnaire was not validated. Finally, self-assessment introduces the possibility of recall bias concerning aspects such as medication use and emergency care. Some patients might have overestimated the negative impact of IBD on their lives.
Despite the limitations, our study is meaningful because it is the first large-scale study to investigate the effects on IBD on the daily life of Korean patients. The results would be valuable in devising strategies of care, and campaigns to increase the awareness of IBD in Korea.
In conclusion, IBD considerably affects the daily life of the patients, including their work, school, and social relationships. Treatment that addresses that full spectrum of a patient's life would be more effective.
References
1. Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008; 14:542–549. PMID: 17941073.

2. Lee JW, Im JP, Cheon JH, Kim YS, Kim JS, Han DS. Inflammatory bowel disease cohort studies in Korea: present and future. Intest Res. 2015; 13:213–218. PMID: 26130995.

3. Choi JH, Kim ES, Cho KB, et al. Old age at diagnosis is associated with favorable outcomes in Korean patients with inflammatory bowel disease. Intest Res. 2015; 13:60–67. PMID: 25691844.

4. Sewell JL, Velayos FS. Systematic review: the role of race and socioeconomic factors on IBD healthcare delivery and effectiveness. Inflamm Bowel Dis. 2013; 19:627–643. PMID: 22623078.
5. Peyrin-Biroulet L, Cieza A, Sandborn WJ, et al. Development of the first disability index for inflammatory bowel disease based on the international classification of functioning, disability and health. Gut. 2012; 61:241–247. PMID: 21646246.

6. Peyrin-Biroulet L, Billioud V, D'Haens G, et al. Development of the Paris definition of early Crohn's disease for disease-modification trials: results of an international expert opinion process. Am J Gastroenterol. 2012; 107:1770–1776. PMID: 23211844.

7. Hu PJ. Inflammatory bowel disease in Asia: the challenges and opportunities. Intest Res. 2015; 13:188–190. PMID: 26130991.

8. Lönnfors S, Vermeire S, Greco M, Hommes D, Bell C, Avedano L. IBD and health-related quality of life: discovering the true impact. J Crohns Colitis. 2014; 8:1281–1286. PMID: 24662394.
9. Romberg-Camps MJ, Bol Y, Dagnelie PC, et al. Fatigue and health-related quality of life in inflammatory bowel disease: results from a population-based study in the Netherlands: the IBD-South Limburg cohort. Inflamm Bowel Dis. 2010; 16:2137–2147. PMID: 20848468.

10. Haapamäki J, Roine RP, Sintonen H, Turunen U, Färkkilä MA, Arkkila PE. Health-related quality of life in inflammatory bowel disease measured with the generic 15D instrument. Qual Life Res. 2010; 19:919–928. PMID: 20361263.

11. Sajadinejad MS, Asgari K, Molavi H, Kalantari M, Adibi P. Psychological issues in inflammatory bowel disease: an overview. Gastroenterol Res Pract. 2012; 2012:106502. PMID: 22778720.

12. Hall NJ, Rubin GP, Dougall A, Hungin AP, Neely J. The fight for ‘health-related normality’: a qualitative study of the experiences of individuals living with established inflammatory bowel disease (IBD). J Health Psychol. 2005; 10:443–455. PMID: 15857873.

13. Jelsness-Jørgensen LP, Bernklev T, Henriksen M, Torp R, Moum BA. Chronic fatigue is associated with impaired health-related quality of life in inflammatory bowel disease. Aliment Pharmacol Ther. 2011; 33:106–114. PMID: 21083587.

14. Yoo S, Jung YS, Park JH, et al. Fatigue severity and factors associated with high fatigue levels in Korean patients with inflammatory bowel disease. Gut Liver. 2014; 8:148–153. PMID: 24672655.

15. Thia KT, Sandborn WJ, Harmsen WS, Zinsmeister AR, Loftus EV Jr. Risk factors associated with progression to intestinal complications of Crohn's disease in a population-based cohort. Gastroenterology. 2010; 139:1147–1155. PMID: 20637205.

16. Kim YS. What is the important issue to prevent the postoperative Crohn's disease? Intest Res. 2014; 12:85–86. PMID: 25349572.

17. Danese S, Fiorino G, Mary JY, et al. Development of red flags index for early referral of adults with symptoms and signs suggestive of Crohn's disease: an IOIBD initiative. J Crohns Colitis. 2015; 9:601–606. PMID: 25908718.

18. Kim ES, Kim WH. Inflammatory bowel disease in Korea: epidemiological, genomic, clinical, and therapeutic characteristics. Gut Liver. 2010; 4:1–14. PMID: 20479907.

19. Devlen J, Beusterien K, Yen L, Ahmed A, Cheifetz AS, Moss AC. The burden of inflammatory bowel disease: a patient-reported qualitative analysis and development of a conceptual model. Inflamm Bowel Dis. 2014; 20:545–552. PMID: 24407484.
20. Dignass A, Van Assche G, Lindsay JO, et al. The second European evidence-based consensus on the diagnosis and management of Crohn's disease: current management. J Crohns Colitis. 2010; 4:28–62. PMID: 21122489.

21. Ye BD, Yang SK, Shin SJ, et al. Guidelines for the management of Crohn's disease. Intest Res. 2012; 10:26–66.

22. Choi CH, Kim YH, Kim YS, et al. Guidelines for the management of ulcerative colitis. Intest Res. 2012; 10:1–25.

23. Walker JR, Ediger JP, Graff LA, et al. The Manitoba IBD cohort study: a population-based study of the prevalence of lifetime and 12-month anxiety and mood disorders. Am J Gastroenterol. 2008; 103:1989–1997. PMID: 18796096.

24. Mittermaier C, Dejaco C, Waldhoer T, et al. Impact of depressive mood on relapse in patients with inflammatory bowel disease: a prospective 18-month follow-up study. Psychosom Med. 2004; 66:79–84. PMID: 14747641.

25. Addolorato G, Capristo E, Stefanini GF, Gasbarrini G. Inflammatory bowel disease: a study of the association between anxiety and depression, physical morbidity, and nutritional status. Scand J Gastroenterol. 1997; 32:1013–1021. PMID: 9361174.

26. Kim ES, Cho KB, Park KS, et al. Predictive factors of impaired quality of life in Korean patients with inactive inflammatory bowel disease: association with functional gastrointestinal disorders and mood disorders. J Clin Gastroenterol. 2013; 47:e38–e44. PMID: 23090047.
27. Bernklev T, Jahnsen J, Henriksen M, et al. Relationship between sick leave, unemployment, disability, and health-related quality of life in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2006; 12:402–412. PMID: 16670530.

28. Daniel JM. Young adults' perceptions of living with chronic inflammatory bowel disease. Gastroenterol Nurs. 2002; 25:83–94. PMID: 12055376.

29. Kemp K, Griffiths J, Lovell K. Understanding the health and social care needs of people living with IBD: a meta-synthesis of the evidence. World J Gastroenterol. 2012; 18:6240–6249. PMID: 23180944.

Table 1
Experience with IBD
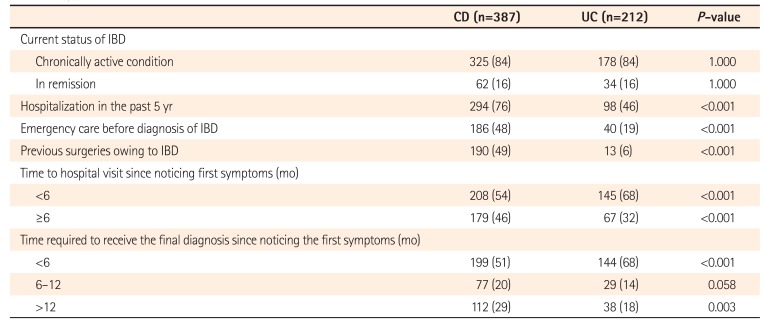
Table 2
Overall Impact of IBD on Daily Life
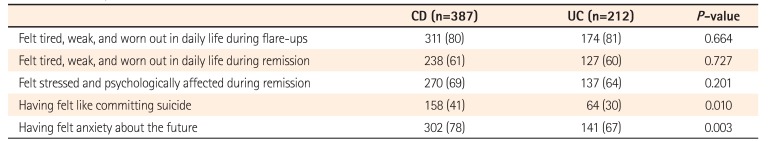
Table 3
Overall Impact of IBD on Work
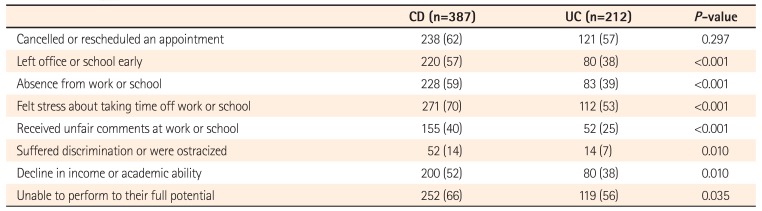
Table 4
Overall Economic Impact of IBD
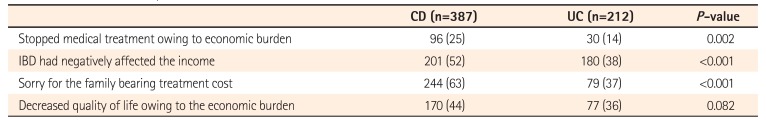
Table 5
Impact of IBD on Relationships




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download