Abstract
Background/Aims
Although multiple treatment options exist for the management of sigmoid colon volvulus, no study has examined the factors associated with successful endoscopic detorsion. This study aimed to examine the clinical course of patients with sigmoid colon volvulus and to identify factors related to successful endoscopic detorsion.
Methods
This study included 30 cases (21 patients) of sigmoid volvulus from among 545 cases of intestinal obstruction at a single center. We retrospectively examined the clinical course and the factors associated with the possibility of endoscopic detorsion of sigmoid colon volvulus.
Results
The rate of laxative use among the study participants was 76.2%; the rate of comorbid neuropsychiatric disorders was 61.9%; and 57.1% of patients had a history of open abdominal surgery. All patients were initially treated with endoscopic detorsion, and this procedure had a 61.9% success rate. The recurrence rate after detorsion was as high as 46.2%, but detorsion during revision endoscopy was possible in all cases. Statistical analysis revealed that the absence of abdominal tenderness (P=0.027), the use of laxatives (P=0.027), and a history of open abdominal surgery (P=0.032) were factors predictive of successful endoscopic detorsion.
Conclusions
The results of our study are consistent with previous reports with respect to the success rate of endoscopic detorsion, the subsequent recurrence rate, and the proportion of patients requiring surgical treatment. In addition, we identified the absence of abdominal tenderness, the use of laxatives, and history of open abdominal surgery as factors predicting successful endoscopic detorsion of sigmoid colon volvulus.
Acute colonic volvulus occurs most commonly in the sigmoid colon.12 Although sigmoid colon volvulus (SCV) is a relatively rare disease, its epidemiology, symptoms, diagnostic methods, treatments, and outcomes have been well researched.34 SCV can compromise the blood supply of the involved segment, leading to ischemia, gangrene, perforation, and death in the absence of optimal treatments.56 Therefore, SCV should be considered an emergent condition.
Although multiple treatment options exist for the management of SCV, nonsurgical reduction with endoscopic detorsion is recommended as the first-line of treatment in patients without bowel gangrene or peritonitis.7 However, no study to date has examined the factors associated with successful endoscopic detorsion. To address this gap in the literature, we reviewed cases of SCV seen in our center and aimed to identify factors associated with successful endoscopic detorsion.
We identified 545 cases of intestinal obstruction at Muroran City General Hospital between January 2008 and December 2014. From among these, the present study included 30 cases (21 patients) of SCV, which were diagnosed based on physical examinations and imaging findings (abdominal radiography, abdominal CT, and lower gastrointestinal endoscopy). All patients without bowel gangrene or peritonitis were initially treated with endoscopic detorsion. When the treatment was unsuccessful, surgical treatment was performed.
This was a retrospective study conducted in a single center. First, we examined the clinical course of the 21 patients with SCV and evaluated the indications for endoscopic detorsion, the incidence rate of SCV recurrence, and the need for follow-up emergency or elective surgery.
Based on patient characteristics (sex; age; general condition [American Society of Anesthesiologists Physical Status, ASA PS]; rate of laxative use; rate of comorbidity with diabetes mellitus, hypertension, cardiac disorders, or neuropsychiatric disorders; and presence or absence of history of open abdominal surgery), white blood cell (WBC) count, levels of AST, LDH, creatine phosphokinase, and CRP at the onset of the disease, and the presence or absence of abdominal tenderness, comparisons were performed between patients who were successfully treated with endoscopy and those who were not. Factors associated with the possibility of endoscopic detorsion were examined. The Muroran City General Hospital Institutional Review Board approved this study.
Data were recorded and analyzed using StatView version 5.01 (SAS Institute Inc., Cary, NC, USA). Results were reported as median and SD for variables with a normal distribution, and as median, minimum, and maximum for variables with a nonnormal distribution. Statistical analysis was conducted with the chi-square test for nominal variables, with nonparametric tests (Mann-Whitney U test, Kruskal-Wallis test) for variables with a non-normal distribution, and with Student t-test for variables with a normal distribution. Two-sided hypothesis testing was used, with a P-value of less than 0.05 considered statistically significant.
Baseline characteristics of the study participants were as follows: 15 men and six women; median age, 76 years (range, 54–90 years); ASA PS (1–2), 16 patients; ASA PS (3–5), five patients; rate of laxative use, 76.2% (16/21); rate of comorbidity with diabetes mellitus, hypertension, cardiac disorders, or neuropsychiatric disorders; 33.3% (7/21), 57.1% (12/21), 23.8% (5/21), and 61.9% (13/21), respectively; and history of open abdominal surgery, 57.1% (12/21). At the time of diagnosis, the median WBC count was 8,910/µL (range, 3,400–17,600/µL), and the median CRP level was 1.80 mg/dL (range, 0.01–11.9 mg/dL).
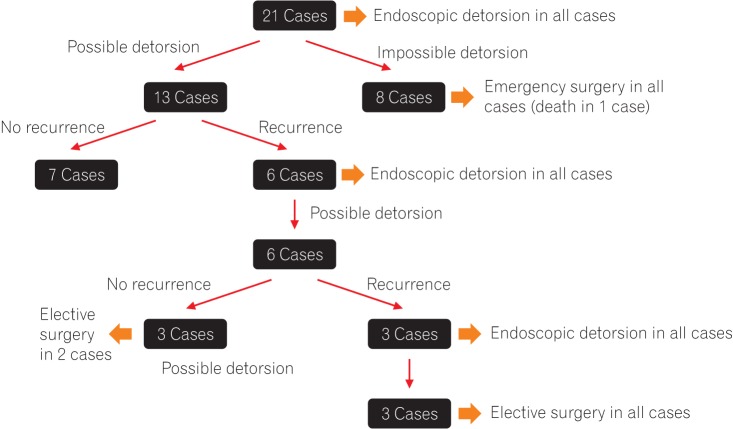
We performed CT before endoscopy in all cases, and observed the findings indicating SCV such as bent inner tube sign (Fig. 1A) and whirl pattern (Fig. 1B). There were no cases demonstrating apparent strangulation signs on CT scan, and thus all patients were initially treated with endoscopic detorsion through lower gastrointestinal endoscopy. This approach was successful in 13 cases. In the remaining eight cases, which required surgical treatment, we observed ischemic mucosal change during sigmoidoscopy in one case (Fig. 2). However, detection was not possible in the remaining seven cases because the endoscope could not reach the point of the volvulus owing to the long and dilated sigmoid colon. Emergency surgery was required in eight cases on the day of admission; the surgery consisted of either sigmoidectomy with intestinal anastomosis (n=4) or sigmoidectomy with colostomy (n=4). There was one case of intraoperative mortality, secondary to septic shock, in this group. Of the 13 cases successfully treated with endoscopic detorsion on the first attempt, there was no recurrence in seven cases, while repeat endoscopic detorsion for SCV recurrence was required in six cases. In the six cases treated endoscopically following SCV recurrence, no further episodes of recurrence were noted in three cases, while a further episode of recurrence was noted in the other three. The latter cases were again treated with endoscopic detorsion, followed by eventual elective sigmoidectomy to definitively prevent any future episodes of recurrence (Fig. 3).
Based on the results described above, the success rate of endoscopic detorsion was 61.9% (13/21). The rate of emergency surgery was 38.1% (8/21). The recurrence rate after detorsion was as high as 46.2% (6/13), and the mean duration from the first endoscopic detorsion to recurrence was 11.8 months (range, 1–36 months). Repeat endoscopic detorsion was achievable in all patients who experienced recurrence. To prevent further episodes of recurrence, all but one patient were treated with elective sigmoidectomy. This procedure was sufficient to prevent further episodes of SCV, and no subsequent recurrence was observed in patients who underwent emergent surgery or in those who underwent elective surgery. Interestingly, all patients who underwent surgery showed excessively elongated intestines.
To identify factors associated with successful endoscopic detorsion, we compared baseline characteristics between patients treated successfully with endoscopic detorsion and those who experienced recurrence. No significant differences in terms of sex; age; general condition; rate of comorbidity with diabetes mellitus, hypertension, cardiac disorders, and neuropsychiatric disorders; or WBC, AST, LDH, creatine phosphokinase, and CRP levels at the time of disease onset were observed between the two groups. Our findings showed that factors associated with endoscopic success were the absence of abdominal tenderness (P=0.027) and the presence of use of laxatives (P=0.027) and history of open abdominal surgery (P=0.032) (Table 1).
This single-center retrospective study followed the clinical course of patients with SCV in detail. The success rate of endoscopic detorsion was 61.9% (13/21) and the recurrence rate was 46.2% (6/13), with 38.1% (8/21) of patients requiring emergency surgical treatment. Of note, the present study is the first to demonstrate that the absence of abdominal tenderness, presence of use of laxatives, and history of open abdominal surgical history are factors predicting successful endoscopic detorsion.
Volvulus, which refers to torsion of a segment of the alimentary tract, is a dangerous condition that often leads to bowel obstruction. The most common site of volvulus is the sigmoid colon, followed by the cecum.1 This condition tends to occur in long redundant colonic segments with elongated mesenteries and a narrow base.8 Volvulus is rare in developed countries and accounts for only 1.90% of all cases of bowel obstruction in the United States, but it is a major cause of bowel obstruction in Africa, the Middle East, and South America.9 SCV usually occurs in older adults, with a mean age of 70 years at presentation.3 Patients are often institutionalized and debilitated due to underlying neurologic or psychiatric disease, and tend to have a history of constipation.7 Some case series have reported that the disease is more prevalent in men, while others have found no gender difference in incidence rates.110 A potential explanation for the increased likelihood of SCV in men is that they are more likely to have a long sigmoid colon and mesentery, and this is especially true in men of Black African descent.
In the present study, the median age of enrolled patients was over 70 years, with a male predominance. All of the patients in our study who were treated with surgical colectomy had longer sigmoid colons, and SCV contributed to 3.9% of all cases of intestinal obstruction. These findings were consistent with those of previous reports.
The goal of treatment of SCV is to reduce the volvulus and to prevent recurrent episodes. Sigmoidoscopy can release SCV when the scope is advanced through the twisted segment of the colon, and the procedure aids in the restoration of blood supply. An additional advantage of sigmoidoscopy is that it permits an assessment of colonic viability.
Some reports in the 21st century have described the management of SCV (Table 2).3711121314 It has been reported that the success rate of endoscopic detorsion of SCV ranges from 55% to 90%, but this procedure is rarely recommended as a definitive treatment because it is associated with a high rate of recurrence of SCV, which approximates 35% to 85%. In addition, the mortality rate of patients presenting with recurrent SCV is as high as 5% to 20%. These data suggest that complications such as gangrene, sepsis, and peritonitis secondary to compromised intestinal blood supply in patients with SCV with recurrent disease are not as rare as has been previously suggested. Therefore, in light of the risks highlighted above, many physicians recommend surgical treatment as the definitive management strategy for SCV following initial colonoscopic decompression. In the present study, relapse did not occur in seven of 21 cases (33%), and surgical treatment was performed in the majority of the remaining cases in which relapse did occur. Considering that more than 30% of elderly patients with SCV did not experience relapse in the current study, we propose that endoscopic detorsion is a safe and effective first-line treatment option in this patient population.
The identification of patient characteristics that predict successful endoscopic detorsion is of great clinical value. In this study, we evaluated the relationship between endoscopic detorsion and several clinical factors. We found that the absence of abdominal tenderness, habitual laxative use, and history of open abdominal surgery were associated with successful endoscopic detorsion of SCV.
The absence of abdominal tenderness may indicate the presence of early stage SCV that has not yet been complicated by bowel gangrene or peritonitis. This finding highlights the importance of taking a thorough clinical history and performing a comprehensive physical examination prior to endoscopic detorsion. Furthermore, it suggests that in elderly patients with SCV with abdominal tenderness, surgical treatment should be considered the first-line approach.
In cases in which the intestinal tract is likely to be extended due to chronic laxative use, endoscopic detorsion is likely to be effective. Interestingly, previous reports have suggested that constipation and laxative use actually predispose to SCV,1516 but these studies have not investigated whether these two factors affect the success rate of endoscopic detorsion. Our data showed that habitual laxative use positively affected the endoscopic success rate, despite the fact that it increases the risk of SCV. A possible explanation for this phenomenon is that endoscopic detorsion is technically challenging in patients with sudden-onset SCV who did not have slightly distended colons secondary to habitual laxative use.
Finally, the present study demonstrated that the success rate of endoscopic detorsion is positively related to a history of open abdominal surgery. However, this finding is inconsistent with previous reports. The reason for this positive relationship is unclear. Nonetheless, considering the possibility that direct torsion of the colon affects the severity of SCV, adhesions occurring because of open abdominal surgery might result in restriction of lower torsion.
The current study has several limitations. First, this was a retrospective study conducted at a single center. Second, the number of cases was relatively small. In this regard, our results should be evaluated with caution. Therefore, future large scale studies are warranted to further investigate the patient characteristics as well as other clinical factors associated with the success rate of endoscopic detorsion in SCV.
In conclusion, the results described in this study are consistent with those previously reported regarding the success and recurrence rates of endoscopic detorsion, as well as the proportion of patients with SCV requiring surgical treatment. In cases in which endoscopic detorsion was possible, the success rate was significantly associated with (1) absence of abdominal tenderness, (2) laxative use, and (3) history of open abdominal surgery.
ACKNOWLEDGEMENTS
All authors helped to perform the research; T.I. wrote the paper; all authors have approved the final draft of the manuscript.
References
1. Påhlman L, Enblad P, Rudberg C, Krog M. Volvulus of the colon: a review of 93 cases and current aspects of treatment. Acta Chir Scand. 1989; 155:53–56. PMID: 2929205.
2. Oncü M, Pískín B, Calik A, Yandi M, Alhan E. Volvulus of the sigmoid colon. S Afr J Surg. 1991; 29:48–49. PMID: 1882313.
3. Halabi WJ, Jafari MD, Kang CY, et al. Colonic volvulus in the United States: trends, outcomes, and predictors of mortality. Ann Surg. 2014; 259:293–301. PMID: 23511842.
4. Kasten KR, Marcello PW, Roberts PL, et al. What are the results of colonic volvulus surgery? Dis Colon Rectum. 2015; 58:502–507. PMID: 25850837.

5. Brothers TE, Strodel WE, Eckhauser FE. Endoscopy in colonic volvulus. Ann Surg. 1987; 206:1–4. PMID: 3606228.

6. Hiltunen KM, Syrjä H, Matikainen M. Colonic volvulus: diagnosis and results of treatment in 82 patients. Eur J Surg. 1992; 158:607–611. PMID: 1363066.
7. Oren D, Atamanalp SS, Aydinli B, et al. An algorithm for the management of sigmoid colon volvulus and the safety of primary resection: experience with 827 cases. Dis Colon Rectum. 2007; 50:489–497. PMID: 17205203.

8. Akinkuotu A, Samuel JC, Msiska N, Mvula C, Charles AG. The role of the anatomy of the sigmoid colon in developing sigmoid volvulus: a case-control study. Clin Anat. 2011; 24:634–637. PMID: 21322064.

9. Asbun HJ, Castellanos H, Balderrama B, et al. Sigmoid volvulus in the high altitude of the Andes: review of 230 cases. Dis Colon Rectum. 1992; 35:350–353. PMID: 1582356.
11. Safioleas M, Chatziconstantinou C, Felekouras E, et al. Clinical considerations and therapeutic strategy for sigmoid volvulus in the elderly: a study of 33 cases. World J Gastroenterol. 2007; 13:921–924. PMID: 17352024.

12. Tan KK, Chong CS, Sim R. Management of acute sigmoid volvulus: an institution's experience over 9 years. World J Surg. 2010; 34:1943–1948. PMID: 20372894.

13. Atamanalp SS. Treatment of sigmoid volvulus: a single-center experience of 952 patients over 46.5 years. Tech Coloproctol. 2013; 17:561–569. PMID: 23636444.

14. Larkin JO, Thekiso TB, Waldron R, Barry K, Eustace PW. Recurrent sigmoid volvulus: early resection may obviate later emergency surgery and reduce morbidity and mortality. Ann R Coll Surg Engl. 2009; 91:205–209. PMID: 19335969.

15. Dülger M, Cantürk NZ, Utkan NZ, Gonullu NN. Management of sigmoid colon volvulus. Hepatogastroenterology. 2000; 47:1280–1283. PMID: 11100333.
16. Khanna AK, Kumar P, Khanna R. Sigmoid volvulus: study from a north Indian hospital. Dis Colon Rectum. 1999; 42:1081–1084. PMID: 10458135.
Fig. 1
Abdominal CT findings. Contrast-enhanced CT showed that the bent inner tube sign (A, arrow) was positive, indicating a markedly dilated sigmoid colon, and that the whirl pattern (B, arrow) was also positive, suggesting torsion of the intestinal tract and rotation of the mesentery; the patient was diagnosed with sigmoid colon volvulus. However, there was no clear evidence of intestinal ischemia.
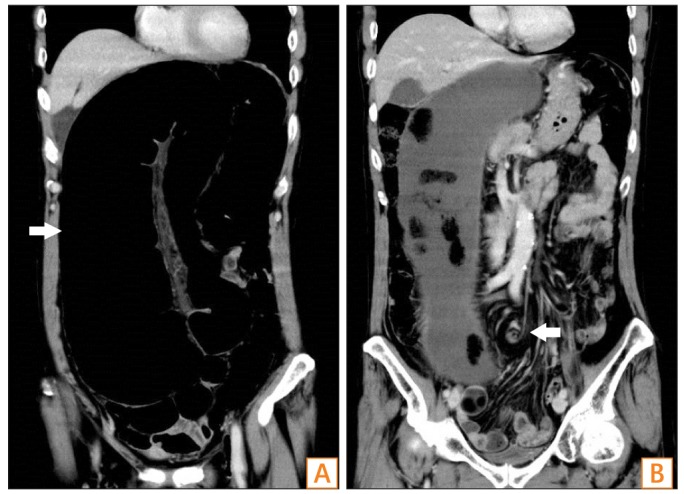
Fig. 2
Sigmoidoscopic findings. Endoscopic detorsion was attempted using lower gastrointestinal endoscopy, but the intestinal lumen was narrowed at a site located 20 cm from the anal verge, and the mucosa displayed a white color, suggesting intestinal ischemia.
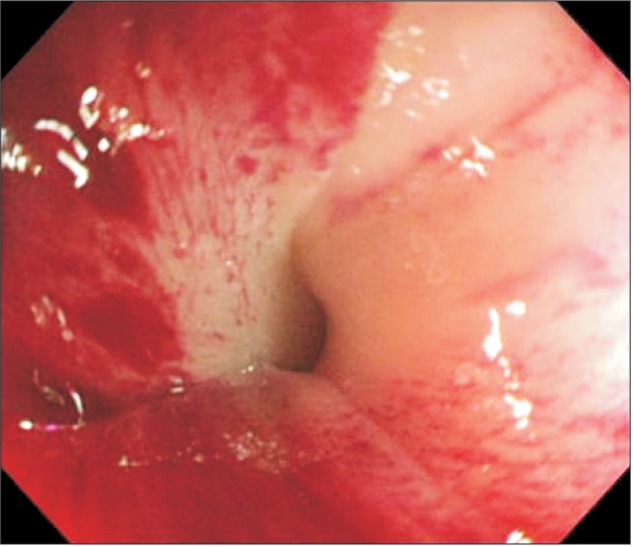
Table 1
Comparison of Baseline Characteristics between Patients Treated Successfully by Endoscopic Detorsion and Those Who Developed Recurrence
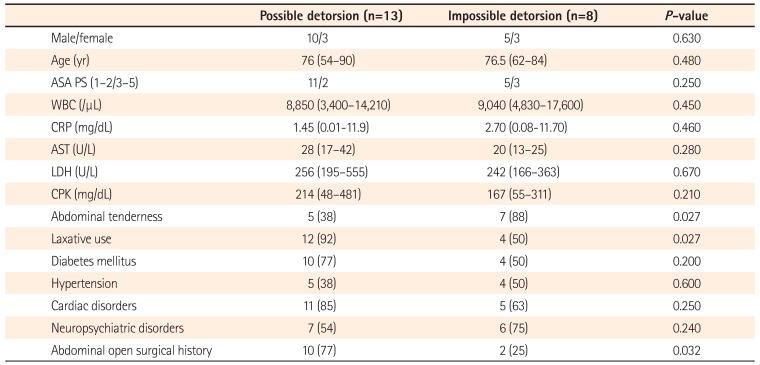
Table 2
Reports Describing the Management of Sigmoid Colon Volvulus
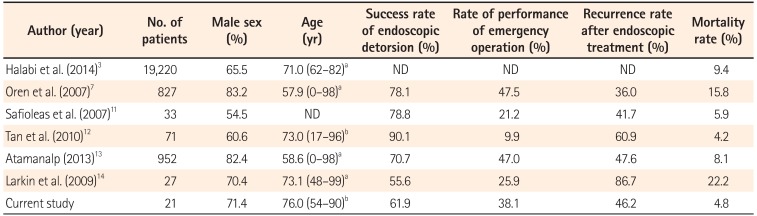
| Author (year) | No. of patients | Male sex (%) | Age (yr) | Success rate of endoscopic detorsion (%) | Rate of performance of emergency operation (%) | Recurrence rate after endoscopic treatment (%) | Mortality rate (%) |
|---|---|---|---|---|---|---|---|
| Halabi et al. (2014)3 | 19,220 | 65.5 | 71.0 (62–82)a | ND | ND | ND | 9.4 |
| Oren et al. (2007)7 | 827 | 83.2 | 57.9 (0–98)a | 78.1 | 47.5 | 36.0 | 15.8 |
| Safioleas et al. (2007)11 | 33 | 54.5 | ND | 78.8 | 21.2 | 41.7 | 5.9 |
| Tan et al. (2010)12 | 71 | 60.6 | 73.0 (17–96)b | 90.1 | 9.9 | 60.9 | 4.2 |
| Atamanalp (2013)13 | 952 | 82.4 | 58.6 (0–98)a | 70.7 | 47.0 | 47.6 | 8.1 |
| Larkin et al. (2009)14 | 27 | 70.4 | 73.1 (48–99)a | 55.6 | 25.9 | 86.7 | 22.2 |
| Current study | 21 | 71.4 | 76.0 (54–90)b | 61.9 | 38.1 | 46.2 | 4.8 |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download