Abstract
Purpose
The robotic platform, an extension of minimally invasive procedures, is distributed nationwide and readily available. However, its application in inguinal hernia repair seems rare in Korea. This report aims to share our initial experience with robotic inguinal hernia repair.
Methods
The patients who underwent robotic inguinal hernia repair by 2 different surgeons with different experiences at a single center were retrospectively analyzed. The surgical procedures were performed on all patients using the Da Vinci Xi robotic platform (Intuitive Surgical Inc). Patient demographics, operation variables, and postoperative outcomes were analyzed.
Results
A total of 35 patients underwent robotic inguinal hernia repairs consecutively. The mean age was 55.03 ± 18.20 years. The majority of patients were male. The overall mean operation time was 103.98 ± 47.92 minutes for unilateral hernia surgery and 139.28 ± 46.07 minutes for bilateral surgery. None of the patients experienced intraoperative complications. However, postoperative complications were noticed in 8 patients: 3 with seroma formation, 1 with hematoma, 1 with superficial surgical site infection, and 3 with persistent pain at the operation site.
Conclusion
This report demonstrates an early experience of hernia surgery using the robotic platform. The robotic approach for transabdominal preperitoneal hernia repair was completed without any significant intraoperative or postoperative complications. It may be a viable option as a minimally invasive technique. Cost-effectiveness, optimal procedural steps, and indications for the robotic approach remain to be further investigated.
Inguinal hernia repair is one of the most common surgeries, with over 20 million cases annually worldwide [1]. In Korea, over 35,000 inguinal hernia surgeries are performed annually [2]. Open hernia repair with mesh has dominated for 30 years and is still the most preferred method in North America [3]. However, the laparoscopic approach for inguinal hernia repair was introduced in 1990 [4]. As minimally invasive surgical technique evolves, the laparoscopic procedure of transabdominal preperitoneal (TAPP) or total extraperitoneal (TEP) approach has gained popularity, accounting for approximately 30% of inguinal hernia repairs in Korea in 2015 [2].
The robotic approach for inguinal hernia repair is another platform for minimally invasive surgery. Based on its enhanced 3-dimensional visualization and articulating instrument, robotic inguinal hernia repair is rapidly expanding in the United States [5]. Surgical outcomes of the robotic approach for inguinal hernia repair have started to appear in the literature, although no conclusive results have been drawn.
Minimally invasive surgical techniques are widely applied in the field of general surgery in Korea. The robotic platform, an extension of minimally invasive procedures, is distributed nationwide and readily available. However, its application in inguinal hernia repair seems rare. Currently, a report on robotic inguinal hernia repair is unavailable in Korea. This report aims to share our initial experience of robotic inguinal hernia repair.
This study was approved by the Institutional Review Board of the Catholic University of Korea, St. Vincent Hospital (No. VC21RASI0194). The need for informed consent was waived because of the retrospective design. The analysis used anonymous clinical data and involved no additional procedure besides routine practices in a clinical setting, presenting no risk of harming the patients.
The patients who underwent robotic inguinal hernia repair by 2 different surgeons from April 2021 to April 2022 were retrospectively analyzed. Two surgeons exhibit a difference in the experience of hernia surgeries; one with over 1,000 cases of inguinal hernia repair (surgeon A) and the other with over 100 cases of inguinal hernia repair (surgeon B). Patient data were collected and constructed from patient medical records. All operations were conducted by the 2 surgeons who had finished the robot platform training program.
Patient demographics, operation variables, and postoperative outcomes were extracted from the electronic medical record. Patient demographics include age, sex, body mass index (kg/m2), American Society of Anesthesiologists physical status classification, Charlson comorbidity index score, previous operation history, laterality of the hernia, and its size. Operation variables include the laterality of the inguinal hernia and the time from skin incision to skin closure. The mean operation time was calculated for patients who underwent surgery solely for hernia repair. Patients who received other surgical procedures, such as prostatectomy, nephrectomy, or adrenalectomy, were excluded in order to get an accurate operation time. Postoperative outcomes were assessed by a visual analog scale assessing postoperative pain, episodes of urinary difficulty, postoperative wound complications, and other postoperative 30-day morbidities.
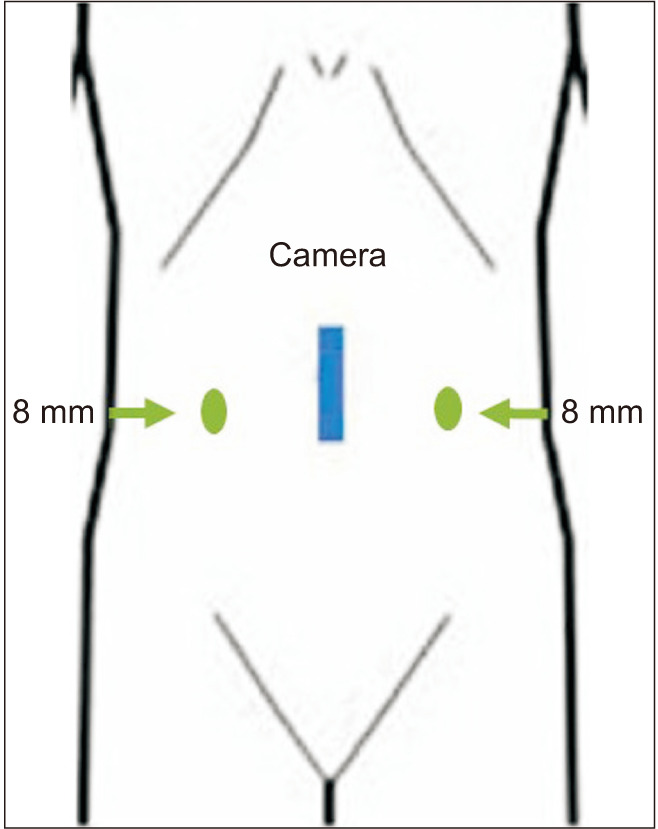
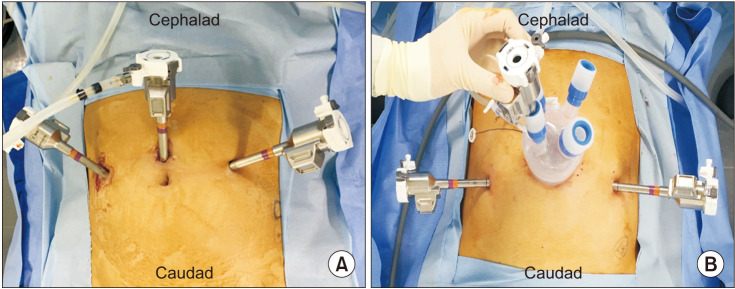
The surgical procedures in all patients were conducted using the Da Vinci Xi robotic platform (Intuitive Surgical Inc.). Under general anesthesia, patients were in the Trendelenburg position. Both surgeons used similar port sites—a transumbilical or supraumbilical incision for the camera port and 2 working arms at the right and left sides of the abdomen in the midclavicular line, as shown in Fig. 1. Although both surgeons used similar trocar sites, surgeon B used the double cannulation method with single port access through the transumbilical incision. In contrast, surgeon A used a robotic cannula through the supraumbilical incision, as shown in Fig. 2A for surgeon A and Fig. 2B for surgeon B. A 2 cm-sized transumbilical incision was created for the single port access, and a single port (LapSINGLE, Sejong Medical) was placed. Because surgeon B lacked experience in the robotic platform and procedure for TAPP, the single port was used for the additional port entry to get assistance instead of using the fourth arm. Then, two 8-mm working ports were placed on the right and left sides of the abdomen in the midclavicular lines, parallel to the umbilicus. The robot was docked between the patient’s legs on the caudal side. The robotic camera was introduced using the double cannulation method, with the robotic cannula inserted into a single port. The more experienced surgeon used only a robotic cannula for instrument access.
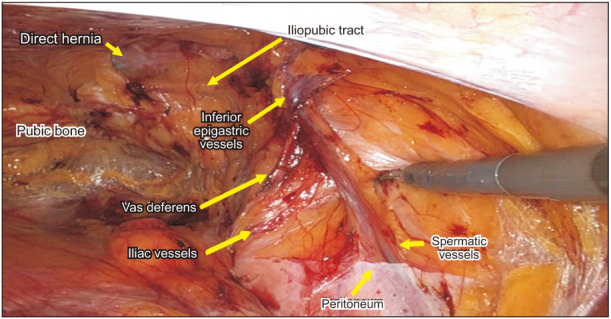
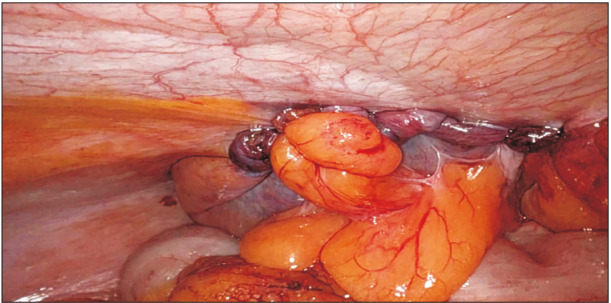
Once the robot was docked, and instruments were inserted, the peritoneal flap was created between the medial umbilical ligament and the anterior superior iliac spine, as shown in Fig. 3. Next, the dissection was conducted into the retroinguinal spaces until the anatomical landmarks, including the epigastric vessels, Cooper and lacunar ligaments, the corona mortis, and external iliac vessels, were fully exposed, as shown in Fig. 4. Then, dissection and reduction of the hernia sac were performed. The lateral dissection was performed until the iliopsoas muscle was exposed and the spermatic vessels were detached from the sac and peritoneum. After a proper mesh size was determined by a surgeon depending on the extent of the peritoneal flap and a patient’s body size, a prosthetic mesh (3DMax Mesh, BD) was placed over the internal ring, femoral ring, and Hesselback’s triangle, as shown in Fig. 5. Surgeon A fixed the mesh by suturing with Vicryl 3-0 at the different sites in the transversalis fascia. Surgeon B used non-absorbable tackers (CapSure, BD) for the mesh fixation at Cooper’s ligament. The peritoneal flap was closed with a continuous suture (MONOFIX, Hanmi Science), as shown in Fig. 6. After completing the peritoneal flap closure, 8 mm port sites were closed using a wound closure to prevent incisional hernia. The transumbilical incision was closed with Vicryl 2-0 continuously. The subcuticular suture was performed to approximate the skin. Then a topical skin adhesive was applied over the incision.
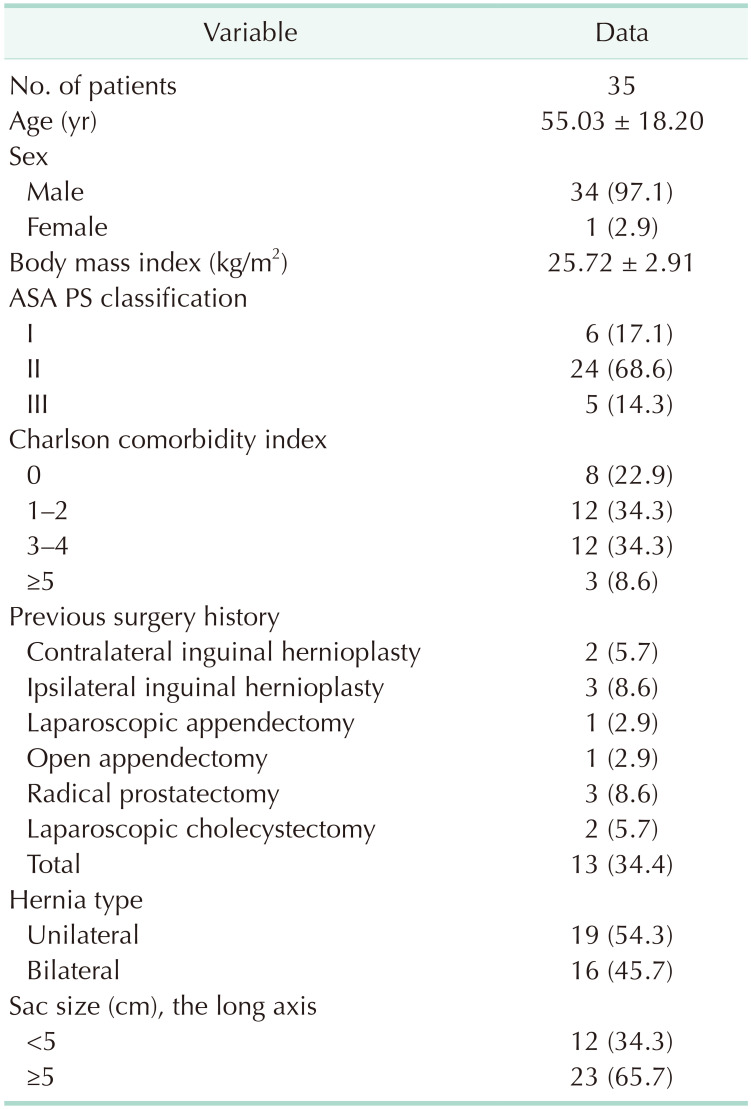
A total of 35 patients underwent robotic inguinal hernia repair consecutively. Thirty-four patients were male, and the mean age was 55.03 ± 18.20 years old, ranging from the youngest at 19 years to the oldest at 78 years. Table 1 demonstrates the patient demographics and previous abdomen operation history. Three patients, 2 with previous open hernioplasty with mesh and plug and 1 with laparoscopic TEP, underwent robotic inguinal hernia surgery due to recurrence. In addition, the patient with a previous open appendectomy underwent robotic TAPP for bilateral hernia—direct type on the right and indirect type on the left sides. The mean operation time is shown in Table 2. The overall mean operation time was 103.98 ± 47.92 minutes for unilateral hernia surgery and 139.28 ± 46.07 minutes for bilateral surgery.
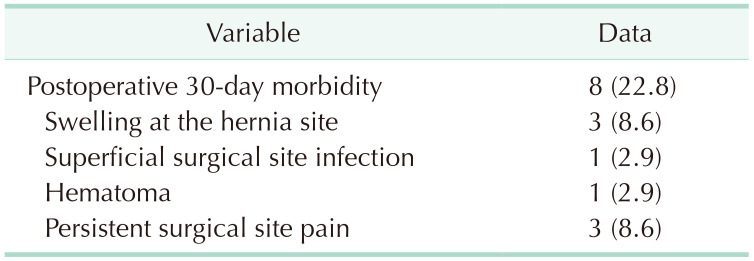
None of the patients experienced intraoperative complications, and urinary retention was not observed immediately postoperatively. Table 3 demonstrates the 30-day postoperative complication, which includes inguinal and scrotal swelling, superficial surgical site infection, hematoma, and persistent surgical site pain. Persistent pain was resolved with pain medication within 1 month.
This report demonstrates an early experience with robotic hernia surgery by 2 different surgeons; one with proficient skills and abundant experience in hernia surgery and another with relatively little experience. However, both surgeons were relatively new to the robotic platform. According to the European Hernia Society guideline, the learning curve for laparoscopic hernia repair begins to flatten after experiencing 50 to 100 cases [6]. Therefore, both surgeons acquired proficiency in performing laparoscopic inguinal hernia repairs, either using the TEP approach or the TAPP approach. Both surgeons successfully performed the robotic TAPP hernia repair without intraoperative complications. Only minor postoperative complications were reported. Thus, a surgeon who gained proficiency in laparoscopic hernia surgery can easily adapt to robotic hernia surgery without experiencing significant difficulty.
Creating a peritoneal flap and intracorporeal suturing in a laparoscopic procedure is demanding and considered an advanced laparoscopic skill. However, three-dimensional vision and articulating instruments in a robotic system make such procedures less arduous than in the laparoscopic approach, allowing the TAPP to be desirable even to an inexperienced, novice surgeon. Indeed, a previous report evaluating learning curves for suturing in robots and laparoscopy demonstrated that even for laparoscopically inexperienced surgeons using a robotic platform, the learning curve was relatively short [7].
Furthermore, the robotic instruments’ strength of grasp and pull can overcome difficult dissection and reduce the hernia sac for complex hernia, which is challenging in a laparoscopic approach. Several studies evaluating the feasibility and safety of robotic hernia repair indicated that a robotic approach successfully completed complex cases without conversion to an open procedure [89]. In addition, a recent study evaluating the feasibility of minimally invasive techniques for hernia repair in patients with a history of previous transabdominal prostatectomy indicates that robotic TAPP demonstrates comparable outcomes in terms of postoperative complications to open inguinal hernia repair, although the operation time was significantly longer in the robotic approach [10]. Therefore, the authors believe that the robotic approach may play a role in dealing with complex laparoscopic cases, such as obese patients, incarcerated hernia, large inguinal scrotal hernia, a history of previous transabdominal surgery, and recurrent hernia.
Long operation times and exorbitant medical expenses are 2 critical concerns regarding robotic hernia repair. For the total operation time, the inexperienced surgeon required nearly 3 hours for bilateral inguinal hernia repair. Despite the fact that the last bilateral inguinal hernia case required less than 150 minutes, the operation time was considerably long. Previous studies also reported that the robotic approach for TAPP hernia repair takes longer than the laparoscopic approach [511]. Kudsi et al. [8] explain that the time needed to prepare the preperitoneal space determines the total surgical time, similar to the laparoscopic approach. Considering that the robotic platform to perform TAPP is relatively new, further evaluation of its efficacy and optimal procedural steps to reduce operation time is necessary.
As for the medical expenses, this report does not include an analysis of medical expenses for robotic hernia repair. However, previous studies reported the high cost of robotic inguinal hernia surgery compared to the laparoscopic approach [511]. As it is well-known that the robotic approach is more expensive than the laparoscopic approach in other fields of surgery, robotic surgery for inguinal hernia repair is not an exception. Therefore, it is necessary to assess the cost-effectiveness of the robotic approach for inguinal hernia repair.
The major limitation of this study is its retrospective design, which is based on the experiences of 2 surgeons at a single center. Operation time and the occurrence of complications may vary significantly, depending on the experience of other surgeons. Additionally, this report did not include a comparative arm of the open or laparoscopic approach; thus, it could not assess the difference between different operative methods.
Our early experience with the robotic TAPP for inguinal hernia repair demonstrates that the robotic approach can be a viable option as a minimally invasive technique to perform inguinal hernia repair. In addition, the robotic platform may be beneficial when dealing with complex hernia cases. However, the cost-effectiveness and optimal procedural steps for the robotic platform must be investigated further.
Notes
References
1. Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet. 2003; 362:1561–1571. PMID: 14615114.
2. Han SR, Kim HJ, Kim NH, Shin S, Yoo RN, Kim G, et al. Inguinal hernia surgery in Korea: nationwide data from 2007-2015. Ann Surg Treat Res. 2019; 97:41–47. PMID: 31297352.
3. Trevisonno M, Kaneva P, Watanabe Y, Fried GM, Feldman LS, Lebedeva E, et al. A survey of general surgeons regarding laparoscopic inguinal hernia repair: practice patterns, barriers, and educational needs. Hernia. 2015; 19:719–724. PMID: 25079224.
4. Ger R, Monroe K, Duvivier R, Mishrick A. Management of indirect inguinal hernias by laparoscopic closure of the neck of the sac. Am J Surg. 1990; 159:370–373. PMID: 2138432.
5. Sheetz KH, Claflin J, Dimick JB. Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open. 2020; 3:e1918911. PMID: 31922557.
6. Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009; 13:343–403. PMID: 19636493.
7. Leijte E, de Blaauw I, Van Workum F, Rosman C, Botden S. Robot assisted versus laparoscopic suturing learning curve in a simulated setting. Surg Endosc. 2020; 34:3679–3689. PMID: 31754849.
8. Kudsi OY, McCarty JC, Paluvoi N, Mabardy AS. Transition from laparoscopic totally extraperitoneal inguinal hernia repair to robotic transabdominal preperitoneal inguinal hernia repair: a retrospective review of a single surgeon’s experience. World J Surg. 2017; 41:2251–2257. PMID: 28337532.
9. Escobar Dominguez JE, Ramos MG, Seetharamaiah R, Donkor C, Rabaza J, Gonzalez A. Feasibility of robotic inguinal hernia repair, a single-institution experience. Surg Endosc. 2016; 30:4042–4048. PMID: 26718359.
10. Dewulf M, Aspeslagh L, Nachtergaele F, Pletinckx P, Muysoms F. Robotic-assisted laparoscopic inguinal hernia repair after previous transabdominal prostatectomy. Surg Endosc. 2022; 36:2105–2112. PMID: 33796906.
11. Prabhu AS, Carbonell A, Hope W, Warren J, Higgins R, Jacob B, et al. Robotic inguinal vs transabdominal laparoscopic inguinal hernia repair: the RIVAL randomized clinical trial. JAMA Surg. 2020; 155:380–387. PMID: 32186683.
Table 2
The mean operation time
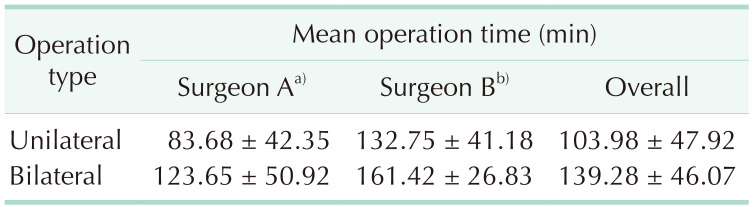
Values are presented as mean ± standard deviation.
Patients with co-operation are excluded: 3 with robot-assisted radical prostatectomy, 1 with robotic partial nephrectomy, 1 with robotic adrenalectomy, and 1 with Holmium laser enucleation of the prostate.
a)Experience of 1,000 hernia surgeries; b)experience of 100 hernia surgeries.




 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download