Abstract
Purpose
Studies in western countries have shown a decline in the incidence of ruptured abdominal aortic aneurysm (rAAA) with advancements in endovascular repair and screening. However, according to health insurance data in Korea based on rAAA code (I71.3), overall rAAA has been increasing. This study aimed to validate the I71.3 code for rAAA and attempt to define the true incidence of rAAA in Korea.
Methods
A 20-year multicenter retrospective review of rAAA was undertaken from the period of January 1, 2000 to December 31, 2020. All patients were diagnosed with the rAAA code I71.3 in each of the 4 hospitals. The CT images and surgical records of these patients were reviewed to differentiate true rAAA and misdiagnosis. Further data on true rAAA patient outcomes including mortality and treatment success were also collected.
Results
A total of 305 rAAA (I71.3) codes were identified in the 4 centers. However, medical record review showed true rAAA in only 131 (43.0%). The remaining 174 cases (57.0%) were misdiagnosed. Impending ruptures were the most common misdiagnoses (37.9%). The total in-hospital mortality including deaths before treatment was 38.9% (n = 51), while mortality of treated patients was 24.4% (n = 15).
Go to : 
Ruptured abdominal aortic aneurysm (rAAA) is a lethal disease with overall mortality of over 30%–50% [1]. Studies in western countries have reported a distinct decrease in the incidence of rAAA over the last 1 to 2 decades. The advancements in endovascular repair and increased screening have resulted in early intervention, which has ultimately led to decreased incidence and lowered mortality from rAAA [123456]. In contrast, eastern countries have reported increasing incidences of rAAA with varying reports in outcome [789]. Despite the increasing incidence and high mortality, true incidence reports and review of treatment outcomes are limited.
Furthermore, unlike the United Kingdom or the United States, Korea lacks nationwide registries, and epidemiologic studies are based on health insurance data. In nations without such systemized registries, disease related groups (DRG) statistics can provide an indirect and estimated overall picture of disease patterns [10]. However, without proper validation, there is a risk of over or underestimation of disease prevalence and incidence. The code for abdominal aortic aneurysm (AAA) is relatively simple and has not had any major changes over the last few updates in both the International Classification of Diseases (ICD) and the Korean Classification of Diseases [9]. There exist only 2 codes pertaining to AAA which are I71.3, which is the ruptured AAA code, and I71.4, which is AAA without rupture. The rupture code covers a wide range of various clinical situations and etiologies. As a result, there exists a discrepancy between the real-world disease and diagnosis claimed by healthcare providers. This resultantly has an effect on the outcome of the disease.
This study aimed to validate the I71.3 code for rAAA and attempt to define the true incidence of rAAA in Korea.
Go to : 
The current study was conducted in accordance with the ethical principles that have their origins in the Declaration of Helsinki. The study protocol was approved by the Institutional Review Board of Seoul National University Hospital (No. 1803-015-926) and the need for informed consent was waived due to the retrospective nature of the study.
In South Korea, the National Health Insurance (NHI) system is an obligatory universal health insurance system that covers 98% of the population. The Health Insurance and Review Assessment (HIRA) database is a government-operated organization that reviews and assesses NHI claims. Data from the year 2010 onwards are publicly accessible online and include sociodemographic information, utilization of inpatient and outpatient services, medical dispensing claims, and as well as diagnoses according to the ICD 10th revision, clinical modification (ICD-10) code.
All patients diagnosed with rAAA from the HIRA database by ICD-10 code I71.3 from January 1, 2010 to December 31, 2020 were identified and reviewed.
To assess the diagnostic accuracy of the rAAA I71.3 code, a detailed retrospective review of patients was undertaken from the following centers located in various regions of Seoul: Seoul National University Hospital, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Korea University Guro Hospital, and Korea Kyunghee Medical Center. All ICD-10 code I71.3 diagnosed patients from the period of January 1, 2000 to December 31, 2020 at each center were identified. The CT images and surgical records of these patients were reviewed by at least 2 physicians at each center.
True rAAA was defined as degenerative AAA with anterior intraperitoneal rupture, posterior retroperitoneal rupture, or aortic fistula to surrounding organs including inferior vena cava, duodenum, or renal vessels [11]. The code cases of I71.3 that did not fit the above definition were categorized as misdiagnoses. This included patients with nondegenerative AAA ruptures due to infection or aortitis, thoracic aorta aneurysms, non-ruptures such as impending ruptures, and patients with uncertain data. Uncertain data includes patients with missing CT images and discordant surgical records that state intact AAA without rupture, despite diagnosis with I71.3 code.
The procedure code system in Korea is based on the Korean Health Insurance Classification of Procedures in Medicine. Unlike the ICD-10, it is complex and there are multiple treatment codes that are applicable to the treatment of AAA. The open repair codes for AAA are O0023, Resection of Aneurysm-Abdominal Aorta (suprarenal and juxtarenal); O0224, Resection of Aneurysm-Abdominal Aorta (infrarenal); and O02034, Resection of Aneurysm-Abdominal Aorta and Iliac Artery. The endovascular aneurysm repair (EVAR) codes for AAA are M6603, Percutaneous Intravascular Installation of Metallic Stent-Aortic; M6611, Percutaneous Intravascular Installation of Stent Graft-Aortic; and M6612, Percutaneous Intravascular Installation of Stent Graft-Aortic and Iliac.
An additional operational definition combining both I71.3 code and treatment codes for both EVAR and open repair were added to extract rAAA patients at each hospital was performed. The addition of this operational definition was attempted to increase diagnostic specificity. The CT images and surgical records of these patients were reviewed to identify true rAAA according to the same definitions as above.
The demographic and clinical variables including age, sex, body mass index, past medical history, and comorbidities were collected. Specific comorbidities included diabetes mellitus, hypertension, chronic obstructive pulmonary disease, pneumonia, cerebrovascular disease, coronary artery disease, dyslipidemia, peripheral arterial disease, other aneurysms, congestive heart failure within <30 days, malignancy, chronic kidney disease, and rheumatoid arthritis.
Among true rAAA patients, the in-hospital mortality outcome was reviewed. The total in-hospital mortality was defined as the mortality combing both the treatment group and deaths before treatment group. Deaths before treatment included death on arrival and futile patients that died before treatment could be offered. The in-hospital mortality of the treatment group was defined as any death within 30 days of rAAA treatment by either EVAR or open repair.
Go to : 
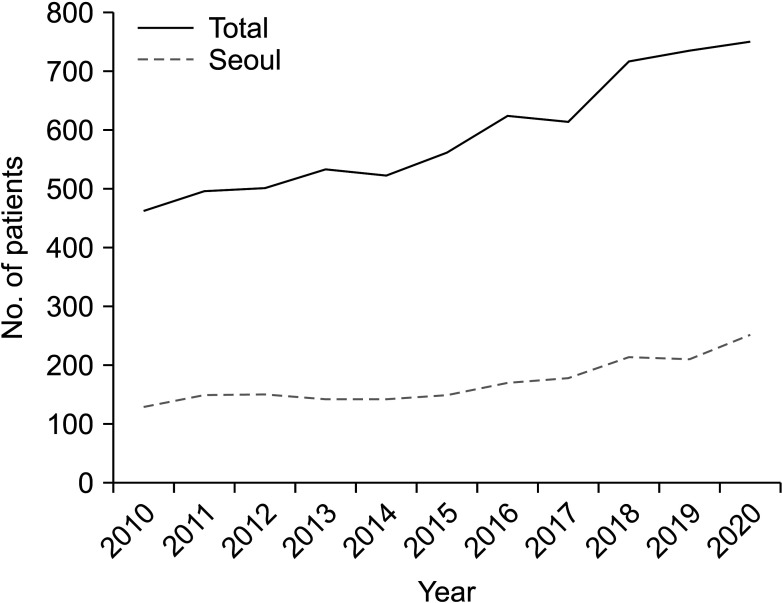
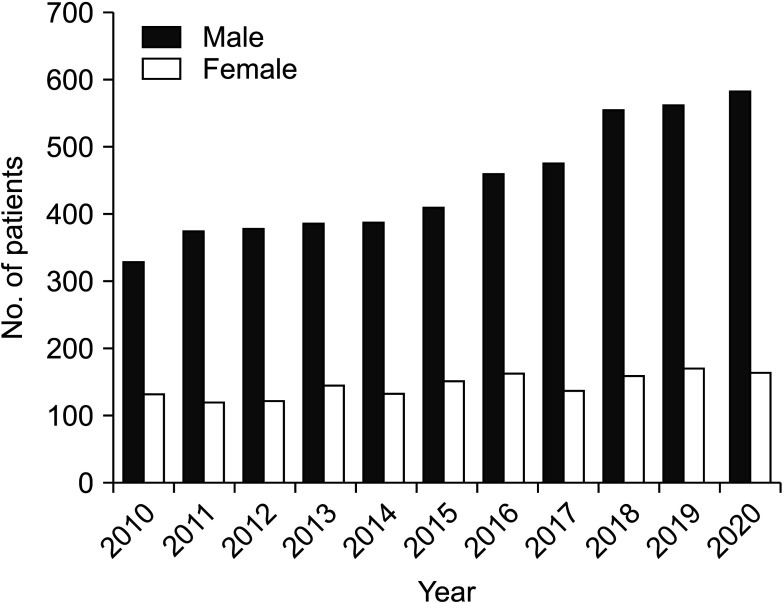
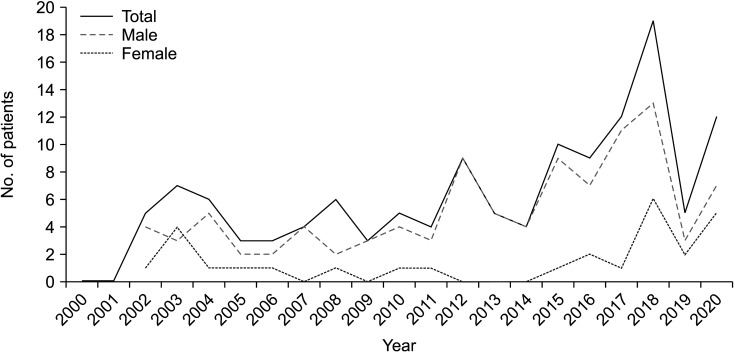
The newly diagnosed case number of rAAA according to the HIRA database has increased annually (Fig. 1). A total of 6,516 cases were observed over the last decade. Of these cases, 28.9% (n = 1,885) occurred in Seoul, the capital of South Korea, and the location of the centers involved in this study. The annual incidence according to sex shows an increase in rAAA cases in male patients while female patients did not significantly increase over time (Fig. 2).
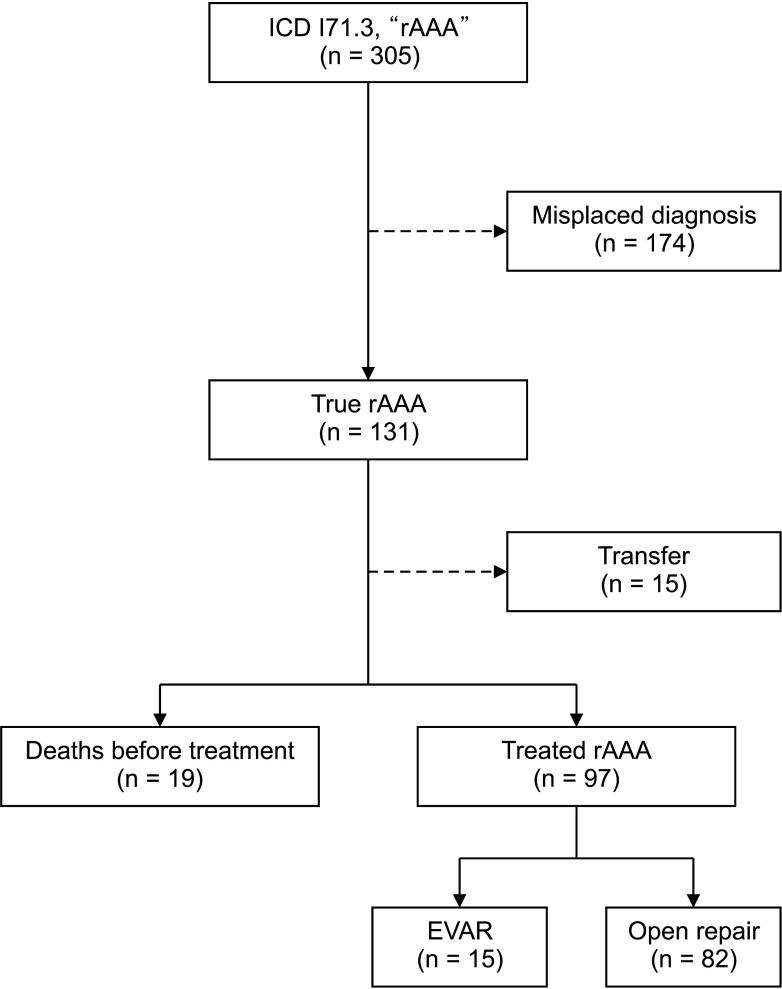
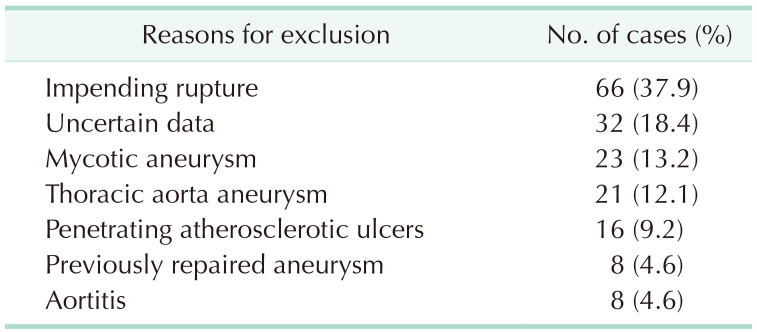
A total of total 305 patients were diagnosed with I71.3 code during the study period of 2000 to 2020 in the 4 centers. Upon review of each patient, only 131 patients (43.0%) were true rAAA. The remaining 174 cases (57.0%) were misdiagnoses (Fig. 3). Impending ruptures were the most common misdiagnoses (37.9%), followed by uncertain data (18.4%), mycotic aneurysm (13.2%), thoracic aortic aneurysm (12.1%), penetrating aortic ulcer (9.2%), previously repaired aneurysm (4.6%), and aortitis (4.6%) (Table 1).
The combination of I71.3 code and operational codes resulted in a total of 126 patients. A review of each patient showed that 39 (31.0%) were true rAAA.
The case number of true rAAA over the 20-year study period in the centers varies annually, but there is a clear increasing trend over the decades (Fig. 4).
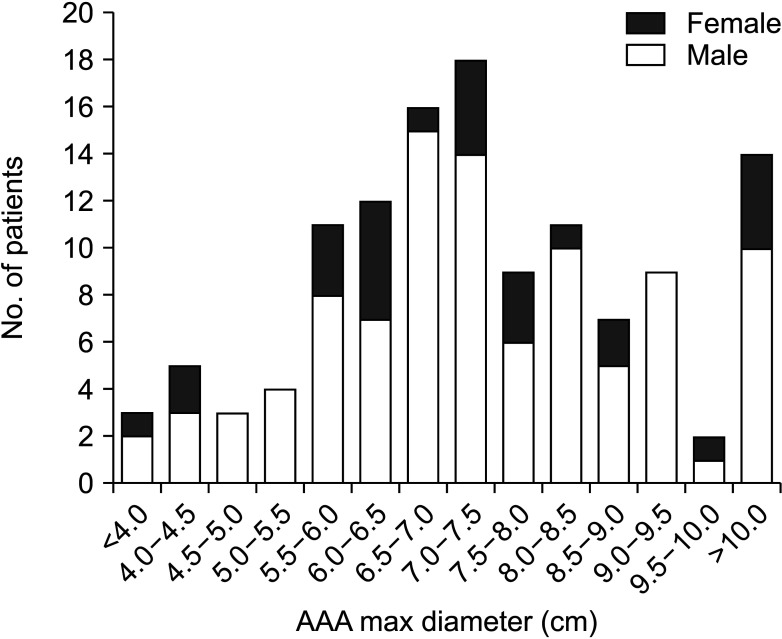
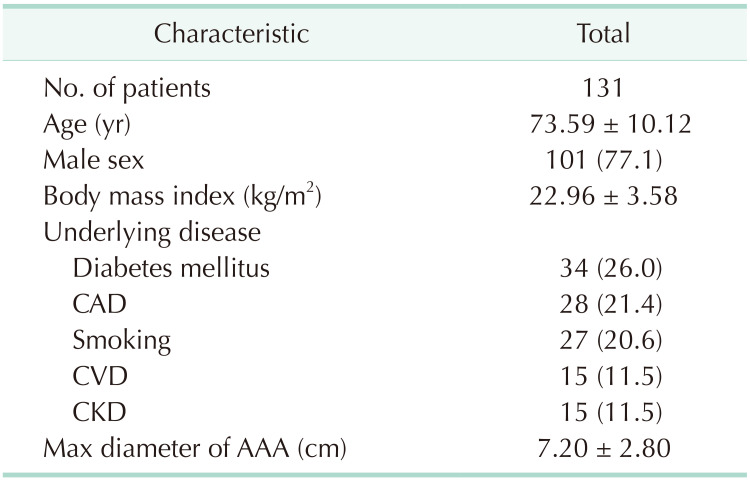
The patient demographics and baseline characteristics are summarized in Table 2. The mean (standard deviation, SD) age of the patients was 73.6 (±10.12) years and 77.1% were males. The most common underlying diseases were diabetes mellitus (26.0%), coronary artery disease (21.4%), and smoking (20.6%). The mean (SD) AAA max diameter was 7.2 (±2.8) cm (Fig. 5).
Among the true rAAA patients, death before treatment occurred in 19 (14.5%); 15 (11.5%) were transferred to other centers; and 97 (74.0%) were treated with either open repair (n = 82, 62.6%) or EVAR (n = 15, 11.5%).
The total in-hospital mortality was 38.9% (n = 51), while in-hospital mortality of treated patients was 24.4% (n = 15). This included 1 EVAR patient and 31 open repair patients.
Go to : 
According to the HIRA database, the national incidence of rAAA in Korea has been annually increasing over the last decade. However, this 20-year multicenter retrospective analysis of I71.3 code for rAAA showed that only 43.0% were true rAAA and the remaining 57.0% were misdiagnoses, of which the most common misdiagnosis was impending rupture (37.9%). This indicates that the I71.3 code is overestimated in the NHI-based data and that the true incidence of rAAA could be much lower.
In an attempt to lower false positives in incidences using only diagnostic I71.3 code, procedure codes for both open and endovascular repair were added. The combination resulted in a total of 126 patients, of which only 39 (31.0%) were true rAAA incidences. Such discrepancies may be due to the lack of standard procedure code classification. There exist multiple treatment codes in the treatment of AAA and delineations for each are not clear. Furthermore, death before treatment, which occurred in 19 (14.5%), and transfers, which occurred in 15 (11.5%), are not accounted for in this operational definition and results in an underestimation of true incidence.
The 2 types of most common misdiagnoses, impending ruptures and inflammatory diseases such as mycotic aneurysm and aortitis, have different outcomes from true rAAA. Due to obscure definitions and ambiguousness of CT findings of “impending ruptures,” it is often classified as rAAA and is responsible for a significant portion of overestimation in rAAA. In this study, impending ruptures accounted for 37.9% of misdiagnoses. Although these diseases also require urgent action, these are not precisely ruptured aneurysms and treatment outcomes of such patients are naturally better than rAAA. Including such patients would have a false positive effect on mortality of rAAA. Inflammatory rAAA, a very minor part of rAAA, has different etiologies from degenerative rAAA and requires different treatments [1213]. However, AAA data whether degenerative, congenital, traumatic, or infectious are collected equally under a single code.
In this study, out of the 305 patients with the I71.3 code, mycotic aneurysms were found in 23 patients (7.5%) and aortitis were found in 8 patients (2.6%). This finding is within the range of 5%–10% infectious rAAA prevalence found by Hellmann et al. [14]. Morphologically, these inflammatory aneurysms show marked fibrosis and extensive inflammation of the adventitia compared to most lymphocyte and plasma cells seen in atherosclerotic aneurysms [13]. The progression of these inflammatory aneurysms is also different, and often growth and ruptures are more rapid and morbid [1315]. Thus, these aneurysms should be classified differently and studied separately. However, due to the infrequency of these nondegenerative rAAAs, it is not accurately subdivided in HIRA and is collected under a single code. This is an inherent limitation of any research performed using the current ICD code system on rAAA.
The total in-hospital mortality including deaths before treatment was 38.9%, while in-hospital mortality of treated patients only was 24.4%. This 1.5-fold difference, in addition to misdiagnosis, may reflect the varying mortality outcomes in different studies of rAAA. In reporting of in-hospital mortality, many futile and untreated rAAA patients are often not included and mortality is underestimated. According to a recent study in Germany using DRG data, in-hospital mortality including deaths before treatment was higher than that of treatment group [10]. Similar results were also found in Switzerland and Belgium [1617]. To select patients for treatment and evaluate risk factors, mortality from rAAA should accurately reproduce real-world data that includes both futile and salvageable patients.
Although the HIRA database is a quite complete registry covering 98% of the total Korean population, the diagnostic codes for diseases need to be further evaluated to be utilized as a source of medical research. The I71.3 code of rAAA in HIRA is nonhomogeneous information based on reimbursement and includes misdiagnosis and aneurysms with several etiologies. HIRA data is useful for understanding the big picture, but it is not a magic bullet that reflects all the details of real-world disease.
There are several limitations to this study. First, the validating data sets provided by the 4 centers are all located in Seoul, the capital of South Korea, and thus are not a nationwide representation. According to studies by Choi et al. [9] and Kim et al. [18], there are significant differences in variables such as patient characteristics, code sensitivity, and management protocols among different regions of Korea. However, more than 20% of the total population lives in Seoul and, similarly, the prevalence of rAAA in Seoul over the last decade was 28.9% of the total rAAA incidence. The incidences of rAAA were higher in metropolitan cities, including Seoul, but no regional difference was seen in overall mortality [9]. Therefore, as the single city with the highest incidence and population density, the dataset is sufficient representation to illustrate the significant inaccuracies in incidence and morality of the I71.3 code. Second, the anterior to posterior diameter of the aneurysms was potentially underestimated, because CT images were obtained after the aneurysms were already ruptured. Moreover, unlike current trends, there were too few cases of EVAR than open repair. These few cases were probably the reason that EVAR showed better outcomes than open repair, which was inconsistent with previous studies conducted in western countries [19]. Yet, this study is the first to validate the I71.3 code for rAAA in Korea.
In conclusion, this study shows that misclassification is a potential source of bias when using diagnostic codes for claims data and that caution needs to be taken before making any conclusive statements. Overreporting of incidence and underestimation of mortality can result. It is imperative to make an effort to increase external validity of claims data. Furthermore, for prospective improvements in treatment protocols and health policies of rAAA in Korea, there should be a prospective nationwide registry and review with sensitive operational definitions.
Go to : 
References
1. IMPROVE Trial Investigators. Comparative clinical effectiveness and cost effectiveness of endovascular strategy v open repair for ruptured abdominal aortic aneurysm: three year results of the IMPROVE randomised trial. BMJ. 2017; 359:j4859. PMID: 29138135.
2. Sampson UK, Norman PE, Fowkes FG, Aboyans V, Song Y, Harrell FE Jr, et al. Global and regional burden of aortic dissection and aneurysms: mortality trends in 21 world regions, 1990 to 2010. Glob Heart. 2014; 9:171–180. PMID: 25432126.
3. Mota L, Marcaccio CL, Dansey KD, de Guerre LE, O’Donnell TFX, Soden PA, et al. Overview of screening eligibility in patients undergoing ruptured AAA repair from 2003 to 2019 in the Vascular Quality Initiative. J Vasc Surg. 2022; 75:884–892. PMID: 34695553.
4. Kontopodis N, Galanakis N, Akoumianakis E, Ioannou CV, Tsetis D, Antoniou GA. Editor’s choice: systematic review and meta-analysis of the impact of institutional and surgeon procedure volume on outcomes after ruptured abdominal aortic aneurysm repair. Eur J Vasc Endovasc Surg. 2021; 62:388–398. PMID: 34384687.
5. Budtz-Lilly J, Björck M, Venermo M, Debus S, Behrendt CA, Altreuther M, et al. Editor’s choice: the impact of centralisation and endovascular aneurysm repair on treatment of ruptured abdominal aortic aneurysms based on international registries. Eur J Vasc Endovasc Surg. 2018; 56:181–188. PMID: 29482972.
6. Anjum A, von Allmen R, Greenhalgh R, Powell JT. Explaining the decrease in mortality from abdominal aortic aneurysm rupture. Br J Surg. 2012; 99:637–645. PMID: 22473277.
7. Wu CY, Chan CY, Huang SC, Chi NS, Wang SS, Wu IH. Outcomes following endovascular or open repair for ruptured abdominal aortic aneurysm in a Chinese population. Heart Vessels. 2014; 29:71–77. PMID: 23306827.
8. Tam G, Chan YC, Chong KC, Lee KP, Cheung GC, Cheng SW. Epidemiology of abdominal aortic aneurysms in a Chinese population during introduction of endovascular repair, 1994 to 2013: a retrospective observational study. Medicine (Baltimore). 2018; 97:e9740. PMID: 29489676.
9. Choi C, Ahn S, Min SI, Ahn M, Ha J, Yoon HJ, et al. Nationwide epidemiologic study of abdominal aortic aneurysms in Korea: a cross-sectional study using National Health Insurance Review and Assessment Service Data. Vasc Specialist Int. 2019; 35:193–201. PMID: 31915663.
10. Kuehnl A, Salvermoser M, Erk A, Trenner M, Schmid V, Eckstein HH. Spatial analysis of hospital incidence and in hospital mortality of abdominal aortic aneurysms in Germany: secondary data analysis of nationwide hospital episode (DRG) data. Eur J Vasc Endovasc Surg. 2018; 55:852–859. PMID: 29685677.
11. Starnes BW, Mehta M, Veith FJ. Ruptured abdominal aortic aneurysm. Springer;2016.
12. van Walraven C, Wong J, Morant K, Jennings A, Jetty P, Forster AJ. Incidence, follow-up, and outcomes of incidental abdominal aortic aneurysms. J Vasc Surg. 2010; 52:282–289. PMID: 20541348.
13. Ladich E, Yahagi K, Romero ME, Virmani R. Vascular diseases: aortitis, aortic aneurysms, and vascular calcification. Cardiovasc Pathol. 2016; 25:432–441. PMID: 27526100.
14. Hellmann DB, Grand DJ, Freischlag JA. Inf lammatory abdominal aortic aneurysm. JAMA. 2007; 297:395–400. PMID: 17244836.
15. Golledge J. Abdominal aortic aneurysm: update on pathogenesis and medical treatments. Nat Rev Cardiol. 2019; 16:225–242. PMID: 30443031.
16. Durieux R, Lardinois MJ, Albert A, Defraigne JO, Sakalihasan N. Outcomes and predictors of mortality in a belgian population of patients admitted with ruptured abdominal aortic aneurysm and treated by open repair in the contemporary era. Ann Vasc Surg. 2022; 78:197–208. PMID: 34416280.
17. Meuli L, Menges AL, Steigmiller K, Kuehnl A, Reutersberg B, Held U, et al. Hospital incidence and mortality of patients treated for AAA in Switzerland. Br J Surg. 2022; 109(Supplement_3):znac189–znac001.
18. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32:718–728. PMID: 28378543.
19. Powell JT, Wanhainen A. Analysis of the differences between the ESVS 2019 and NICE 2020 guidelines for abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2020; 60:7–15. PMID: 32439141.
Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download