INTRODUCTION
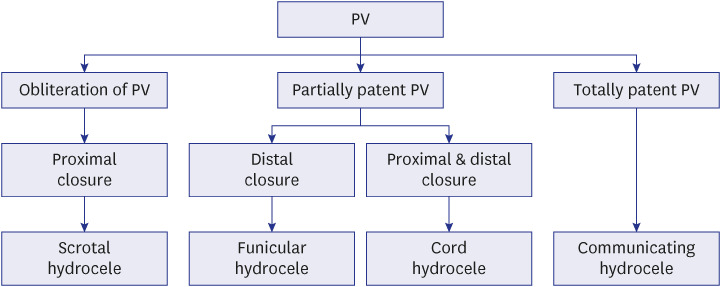
A hydrocele is a fluid collection within the tunica vaginalis around the testicle or within the spermatic cord. When the fluid travels from the abdominal cavity through a patent processus vaginalis (PV), it is a communicating hydrocele. In contrast, a noncommunicating hydrocele has no connection to the abdominal cavity. These PVs can be classified into obliterated, partially patent, and totally patent PVs.
1
Hydrocelectomy is one of the most common operations in children.
2 Conventional open hydrocelectomy is simple and safe, providing fast recovery and low morbidity. The laparoscopic approach can be practical in bilateral communication cases.
3 Although patent PV can be easily detected with laparoscopic surgery, noncommunicating hydrocele is unsuitable for laparoscopic surgery.
Communicating hydroceles are essentially associated with inguinal hernias, sharing a common etiology
4 and a similar method of surgical repair.
5 Both diseases occur due to the patent PV or the patency of the internal inguinal ring. Several studies have examined metachronous contralateral inguinal hernia, especially in infants.
67891011 Metachronous contralateral hydroceles are uncommon compared to inguinal hernias, and this topic has not been widely explored.
Many studies of hydroceles with patent PVs have been investigated along with inguinal hernias. However, the two entities have distinct natural courses; inguinal hernias do not improve naturally after development, whereas hydroceles with patent PVs can resolve spontaneously. Therefore, it would be meaningful to separate hydroceles with patent PVs from inguinal hernias and investigate surgical findings and metachronous contralateral hydroceles of hydroceles in these patients.
There are also few reports in the literature explicitly targeting hydrocelectomy, although it appears that the classic treatment of hydrocele using an inguinal approach still represents the standard of care.
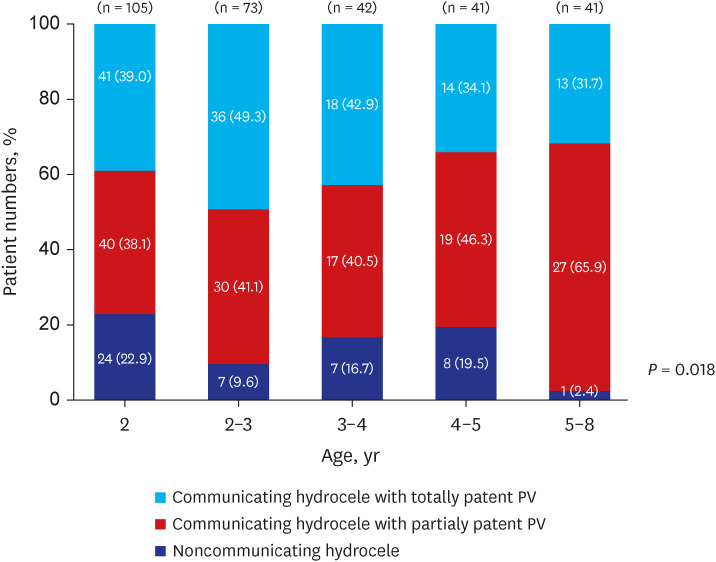
We aim to report the distribution of hydrocele types according to age and analyze the incidence and risk factors of metachronous contralateral hydroceles in children under 8 years old.
Go to :

METHODS
Data acquisition
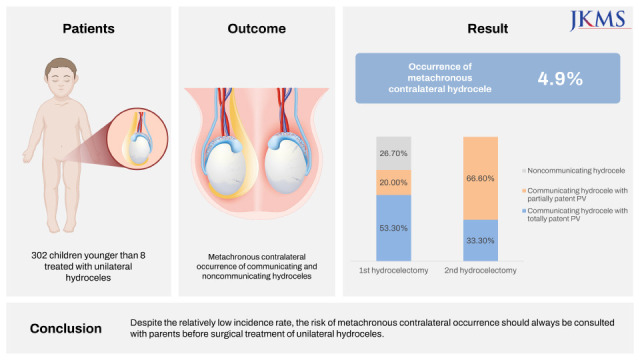
From January 2017 through June 2020, 302 children younger than 8 years were treated with unilateral hydrocelectomy without contralateral exploration by a single surgeon. Patients were excluded from the study if they had a bilateral hydrocele, had clinical evidence of an inguinal hernia containing abdominal contents (bowel or omentum), an associated undescended testis, or had previously undergone inguinal surgery on either side.
Diagnosis
The diagnosis of hydrocele was based on clinical presentation, physical examination, and ultrasonographic findings. Ultrasonography was used to determine complex cases or suspected cases of bilateral hydroceles. We suspected the presence of communicating hydrocele when there was a change in hydrocele size during a Valsalva maneuver or straining or crying and during direct manual palpation.
Surgery
Hydrocelectomy was performed using the inguinal or scrotal approach, depending on the initial impression of communicating or noncommunicating hydrocele. We chose inguinal incision for cases of suspected communicating hydrocele and scrotal incision for suspected noncommunicating hydrocele. Communication was confirmed inside the surgical field by examining the PV directly for a defect in communicating in hydroceles.
Follow-up
All patients revisited our institution 6 months after the first hydrocelectomy to check for postoperative conditions. Patients were recommended to revisit before age 8 when they entered school. When there was a new onset hydrocele on the opposite side during follow-up, they were detected the same way as the initial diagnosis. The second surgery was done at least after a postoperative period of 6 months.
Outcome analysis
We performed a cross-sectional study to obtain clinical data, including age at first visit and operation, weight and height at the time of surgery, body mass index, laterality, incision method, type of hydrocele, patent PV status, and hydrocele wall thickening (visually determined intraoperatively), and operation time. Transient scrotal edema, transient postoperative hydrocele, and ipsilateral recurrence of hydrocele were excluded from the study. We defined the types of PV as obliterated, partially patent, and totally patent types. Hydrocele was categorized into communicating (with partially or totally patent PV) and noncommunicating (with obliterated PV) according to the type of PV (
Fig. 1). Communicating hydroceles with patent PV was determined by directly examining open communication between the scrotal sac and the peritoneum in the surgical field. If the PV was partially obliterated inside the inguinal canal, it was defined as communicating hydroceles with partially patent PV. This category includes funicular hydrocele with cord hydrocele or funicular hydrocele with scrotal hydrocele. Noncommunicating hydroceles had no connection between the abdominal cavity and the scrotal sac.
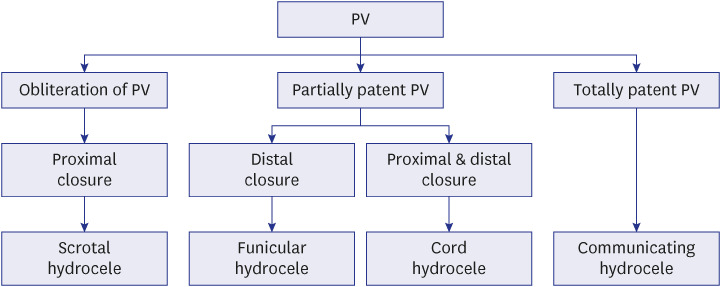 | Fig. 1
Classification of PV-related disorders.
PV = processus vaginalis.

|
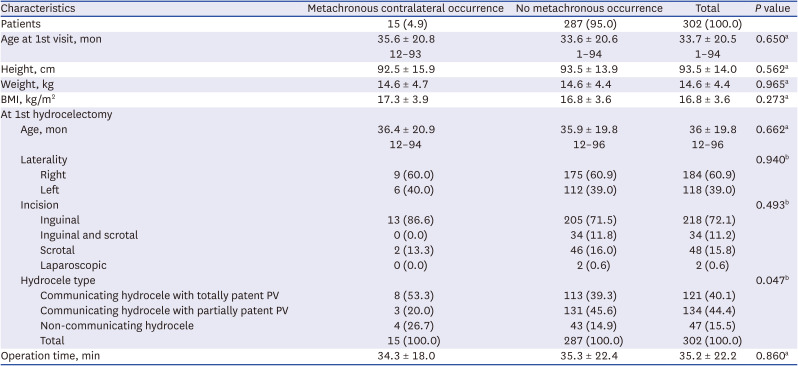
We divided the patients into two groups according to the presence of metachronous contralateral hydroceles and analyzed the differences between the two groups.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics (v. 26.0; IBM Co., Armonk, NY, USA) with the Mann-Whitney test, Fisher’s exact test, or Spearman’s correlation. The patients’ data were analyzed using nonparametric tests, and a P value less than 0.05 was considered statistically significant.
Ethics statement
After obtaining approval from Institutional Review Board of Pusan National University Yangsan Hospital (IRB No. 05-2020-265), we performed a retrospective chart review for all children who underwent unilateral hydrocelectomy at our institution. The board waived submission of informed consents.
Go to :

DISCUSSION
Most hydroceles resolve with age, and surgery is considered when the hydrocele persists until the age of 2 years and does not decrease in size.
12 The surgery for a communicating hydrocele is essentially the same as repairing an inguinal hernia.
13 Hydrocelectomy involves an inguinal approach to make sure that there is a patent PV or inguinal hernia. Once the high ligation of the patent PV has been completed, the distal part of the hydrocele is widely opened to avoid injury to the testicle instead of completely removing the hydrocele sac to prevent recurrence, which is the method we chose in our study. Noncommunicating hydroceles are distinct from communicating hydroceles and inguinal hernias and require a scrotal incision.
According to several studies on inguinal hernia, which share a common pathophysiology with communicating hydroceles, the risk of contralateral inguinal hernia after unilateral inguinal hernia repair has been 5 to 20%.
1114 Kemmotsu et al.
8 found that the overall incidence of contralateral inguinal hernia was 11.6% (116 of 1,001). In boys, the incidence was 13.1%, 13.7%, and 11.7% in those under 1 year, under 2 years of age, and in total, respectively. In children, the incidence of contralateral inguinal hernia was lower (7.6%). Given this low incidence of contralateral inguinal hernia after unilateral inguinal hernia repair, the authors do not recommend contralateral exploration for infants and children with unilateral inguinal hernia.
The risk of metachronous contralateral hydrocele after unilateral hydrocelectomy may be even lower than that of inguinal hernia. There are also few reports in the literature specifically targeting hydrocelectomy, although it appears that the classic treatment of hydrocele using an inguinal approach still represents the standard of care.
12 Lym et al. investigated the risk of contralateral hydrocele and inguinal hernia after unilateral hydrocelectomy in 85 children 5 to 107 months old (median age, 37). Contralateral hydrocele or inguinal hernia developed in 6 of the 89 patients (7%) 6 to 15 months (median, 12) postoperatively. They do not recommend routine contralateral exploration in children undergoing unilateral hydrocelectomy.
11 We limited the present study to hydroceles only and excluded inguinal hernias. Metachronous contralateral occurrence is lower (4.9%) in hydrocele compared to inguinal hernia (7.6–11.6%) proposed in other recent studies.
Most cases of pediatric hydroceles can be diagnosed with history taking and adequate physical examination. Few patients require further radiological investigation for aid in diagnosis. Ultrasound study is known to detect contralateral patent PVs. It uses the 7.5 MHz transducer and currently is the modality of choice to aid the diagnosis of patent PVs, with a reported accuracy of 91.7%.
15 Detection of the inflow of peritoneal fluid within the inguinal canal is diagnostic for a hydrocele. Preoperative ultrasound with selective contralateral patent PV closure in children can be an alternative to routine laparoscopy in detecting contralateral inguinal hernia or hydrocele development. However, the sensitivity of ultrasound detection of patent PVs have been questioned. Yip investigated the usefulness of ultrasound for detecting the closure of contralateral patent PV in 322 pediatric patients with unilateral inguinal hernia and hydrocele.
16 In 96 cases (30%), contralateral patent PV was identified with ultrasound, 95% of which were affirmed intraoperatively. In this study, an inguinal ultrasound study is a valuable tool as an adjunct in pediatric inguinal hernia management by detecting contralateral patent PV with high accuracy.
To prevent metachronous contralateral occurrence after hydrocelectomy, a surgeon can offer bilateral hydrocelectomy according to the ultrasound finding. In our study, bilateral surgery was performed in cases in which bilaterality of disease was confirmed by ultrasound or physical examination at the first visit. However, metachronous contralateral occurrence also occurred in patients diagnosed with unilateral hydrocele by ultrasound study at the first visit. Therefore, we found that not all metachronous occurrences can be predicted by ultrasound study. Since it may vary depending on the experience and ability of the ultrasound examiner, clinicians should pay attention to the ultrasound findings.
Laparoscopy has been widely used to evaluate contralateral patent PV. It has been proved to be both sensitive (99.4%) and specific (99.5%) in its use.
17 Bhatia et al.
18 performed a total of 284 unilateral inguinal hernia repairs with laparoscopic explorations. They discovered positive findings during explorations in 65 of 171 (38%) children less than 2 years of age, 19 of 101 (20%) of children 2 to 8 years of age, and 1 of 12 children greater than 8 years of age (8%). However, the false-negative incidence of laparoscopic contralateral patent PV evaluation was low.
17 Also, not every contralateral patent PV would develop into a clinically apparent inguinal hernia.
1920 This led to the contralateral exploration after a unilateral inguinal hernia repair to be a controversial topic in pediatric surgery. Likewise, we do not recommend laparoscopic exploration of contralateral patent PV in communicating hydrocele patients due to the low incidence of contralateral hydroceles and the controversy in performing this method.
There are several limitations to our study. First, as this study was conducted retrospectively, our analysis may have potential biases. Because our data include only patients that need surgical treatment, cases of subclinical hydroceles and mild hydroceles that do not require surgery could be overlooked. Second, because this study was conducted in a single center, collecting cases of contralateral occurrence was challenging due to the low rate of occurrence. Because there was a great difference in sample size (15 vs. 287), the outcomes of our analysis is underpowered. For proper analysis of risk factors of metachronous occurrence, multicenter research will be beneficial. Finally, routine ultrasonography is not conducted preoperatively in our clinic, and 32.1% of patients were checked in our study. Thus, we may have overlooked contralateral hydroceles, and some cases may have been misdiagnosed as unilateral hydroceles.
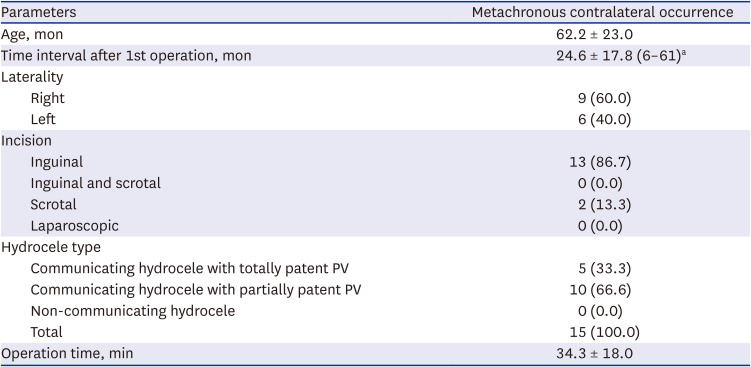
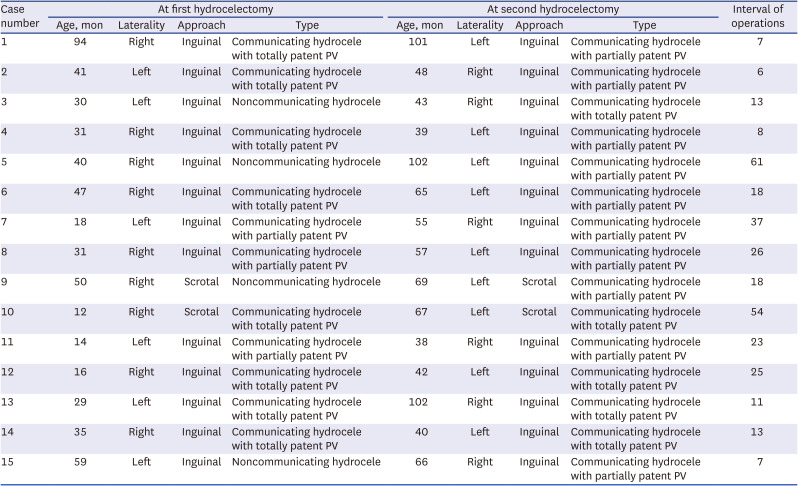
In conclusion, the clinically evident risk of metachronous contralateral hydrocele after unilateral hydrocelectomy in children younger than 8 years was 4.9%. The hydrocele type of the metachronous occurrence was not always identical to the previous type of hydrocele. Regardless of the first hydrocele type, a latent communicating hydrocele on the opposite side can manifest later in life. Metachronous contralateral occurrence manifested as communicating hydroceles, including hydroceles that were initially noncommunicating. Due to the small incidence of metachronous contralateral hydrocele compared with metachronous contralateral inguinal hernia, contralateral exploration with laparoscopy or ultrasound is unnecessary. However, during the surveillance, physical examination is essential for metachronous contralateral occurrence after unilateral hydrocelectomy in children. Despite the low incidence, the possibility of metachronous contralateral hydrocele should always be consulted with parents before operation.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download