This article has been
cited by other articles in ScienceCentral.
Abstract
We report 2 cases of arrested pneumatization of the sphenoid sinus, a normal variant commonly misdiagnosed as a serious condition of the skull base. A 65-year-old man visited a local clinic for regular checkups. Brain CT showed a non-expansile lesion of the soft tissue with a well-defined sclerotic margin in the clivus but without destruction or mass effect on the surrounding bony structures. Subsequent brain MRI revealed that the lesion within the clivus was a high-signal lesion on the T2-weighted image, containing a low-signal round mass seen on a high-intensity signal on the T1-weighted image without contrast enhancement. Thus, the lesion was considered to contain internal fat. A 70-year-old woman diagnosed with a tumor in the greater sphenoid bone visited our hospital. Her brain CT revealed a non-expansile lesion of mixed density and a well-demarcated lesion and internal curvilinear calcification in the left greater wing of the sphenoid bone. The margin was osteosclerotic and the adjacent bony structure was intact. Her brain MRI showed that the lesion within the greater sphenoid bone had multiple low-signal lesions within a high-signal lesion on the T2-weighted image, suggesting internal fat contents. The lesions were diagnosed as arrested pneumatization of the sphenoid sinus and no further examination or treatment was performed. Arrested pneumatization of the sphenoid sinus should be considered in the presence of non-expansile lesion with an osteosclerotic boundary and internal fat component in the skull base.
Go to :

Keywords: Bone, Diagnosis, Skull, Sphenoid sinus
INTRODUCTION
Arrested pneumatization of the sphenoid sinus is a normal development variant. The process of pneumatization begins in the uterus and proceeds through puberty [
1]. Accessory and absent or hypoplastic sphenoid sinuses are common anatomical variants, but arrested pneumatization is rare and occurs through another process, and leads to errors in the diagnosis of skull base lesions [
2]. The sphenoid bones undergo fatty marrow conversion before the normal pneumatization occurs [
34567]. In rare cases for no specific reason, the pneumatization fails before the respiratory mucosa fully extends into the site of fatty marrow conversion. In this case, atypical fatty marrow remains permanently around the sphenoid sinus even in adulthood, thus called arrested pneumatization. In a non-expansile, non-eroded lesion with sclerotic margins, internal curvilinear calcification, and no destruction of surrounding structures on brain CT of the skull base, internal fat component on brain MRI is characteristic for diagnosis of arrested pneumatization. If the brain CT or MRI findings for this variant are not recognized, it is likely to be mistaken for a serious disease in the skull base. Therefore, we report 2 rare cases of arrested pneumatization prone to misdiagnosis for other skull base diseases leading to unnecessary examination or surgical biopsy or treatment.
Go to :

CASE REPORT
Case 1
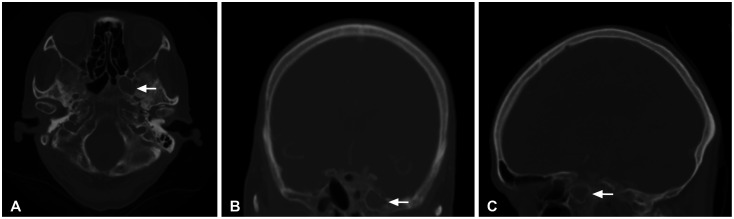
A 65-year-old man diagnosed with clivus tumor was referred to our hospital by a private clinic for further assessment and treatment. The patient regularly visited the clinic for checkups. He was initially diagnosed with a chordoma or a chondrosarcoma in the clivus, but without specific neurological symptoms. His brain CT revealed a non-expansile lesion of the soft tissue with a non-eroded, well-defined sclerotic margin and internal curvilinear calcification in the clivus, without destruction or mass effect on the surrounding bony structures (
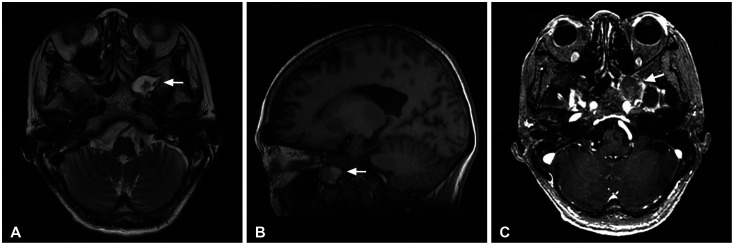
Fig. 1). As the first impression, this bone tumor was considered to be benign by a radiologist, such as hemangioma or fibrous dysplasia. Malignant tumors at the skull base, such as chordomas, chondrosarcomas, and metastases were also included in the differential diagnosis. Chest, abdomen, pelvis CT revealed no evidence of primary tumor of metastases. Subsequently, his brain MRI showed that the lesion within the clivus was a high-signal lesion on the T2-weighted image containing a low-signal round mass observed as a high-signal mass on the T1-weighted image without contrast enhancement, which was then suspected as internal fat (
Fig. 2). Given the typical radiological appearances in the brain CT and MRI, the lesion was diagnosed as arrested pneumatization of the sphenoid sinus in the clivus. Since this is a normal development variant, no additional examination or treatment was performed.
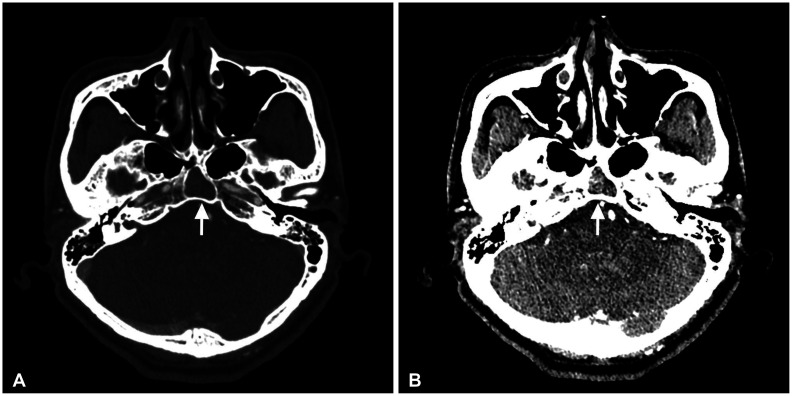 | Fig. 1Brain CT images (A: bone window, B: non-enhanced) show a non-expansile lesion (arrows) with a well-defined sclerotic margin and internal curvilinear calcification in the clivus. No destruction or mass effect on the surrounding bony structures is visible.
|
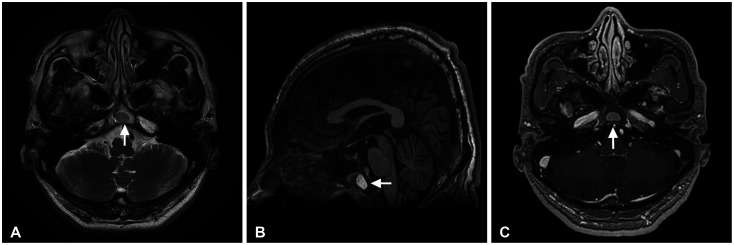 | Fig. 2Characteristic internal fat component (arrows) has a low signal on T2-weighted MR image (A) and a high signal on T1-weighted MR sagittal image (B). No contrast enhancement is seen on T1-weighted MR image with contrast (C).
|
Case 2
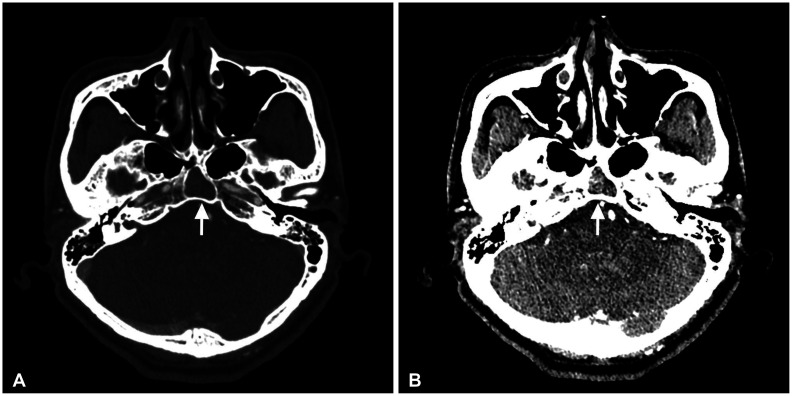
A 70-year-old woman diagnosed with a tumor in the greater sphenoid bone visited our hospital for further assessment and treatment. She was accidentally discovered with a sphenoid bone tumor during a regular checkup. Initial diagnosis was a chordoma or metastasis. The patient had no specific neurological symptoms, but her brain CT revealed a non-eroded, non-expansile lesion of mixed density with a well-demarcated lesion and internal curvilinear calcification in the left greater wing of the sphenoid bone (
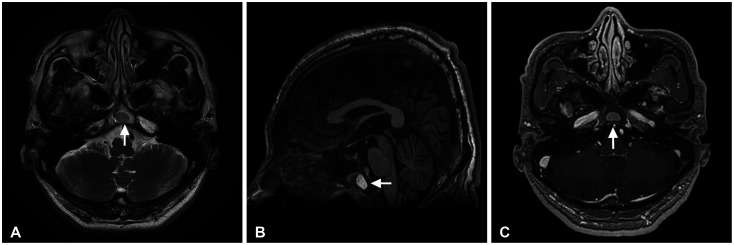
Fig. 3). The margin was osteosclerotic, and the adjacent bony structure was intact and showed no mass effect. Differential diagnosis was undertaken to distinguish between benign bone and malignant bone tumors. The chest, abdomen, and pelvis CT revealed no evidence of primary tumor of metastases. Subsequently, her brain MRI showed that the lesion within the greater sphenoid bone had multiple low-signal lesions within a high-signal lesion on the T2-weighted image (
Fig. 4). The multiple masses were observed as a high-signal entities on the T1-weighted image without contrast enhancement, thereby suggesting internal fat contents. The lesion was diagnosed as arrested pneumatization of the sphenoid sinus and no further examination or treatment was performed.
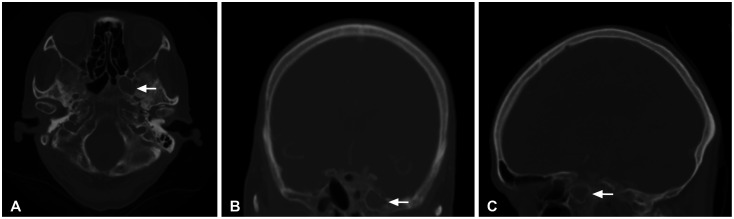 | Fig. 3Brain CT bone window (A: axial, B: coronal, C: sagittal) shows a non-expansile lesion (arrows) with a well-demarcated lesion and internal curvilinear calcification in the left greater wing of the sphenoid bone. The margin is osteosclerotic. There is no destruction or mass effect on the adjacent bony structure.
|
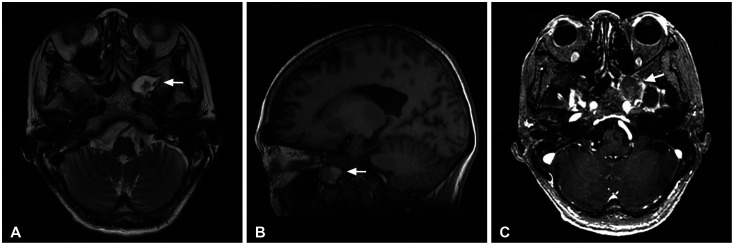 | Fig. 4Brain MRI shows that the lesion (arrows) within the greater sphenoid bone has multiple low-signal lesions within a high-signal lesion on the T2-weighted image (A), suggesting internal fat contents. It has a high signal on T1-weighted MR sagittal image (B). No contrast enhancement is seen on T1-weighted MR image with contrast (C).
|
The Institutional Review Board of Kyungpook National University Hospital exempted the requirement for informed consent due to the retrospective nature of the study and the minimal risk for the patient. This report was conducted according to the guidelines of the Declaration of Helsinki for biomedical research.
Go to :

DISCUSSION
Arrested pneumatization is a rare development and anatomical variant and is the most common around the sphenoid sinus. Normally, conversion from red marrow to the fatty marrow occurs in the sphenoid bones prior to the normal pneumatization [
3456]. Marrow conversion in the sphenoid sinus starts at the presphenoidal region anteriorly and proceeds to the clivus posteriorly. Although not clear, factors such as temperature, bone composition, and vascularization are involved in the arrest of pneumatization [
7]. The failure of normal pneumatization causes the fatty marrow to remain permanently even in adults, thus called arrested pneumatization. Arrested pneumatization is asymptomatic and usually discovered radiographically by accident. There are no specific symptoms associated with this variation. Knowledge on this variation would aid in establishing a differential diagnosis radiologically and thus avoid unnecessary examination or surgery.
Arrested pneumatization is usually observed in areas surrounding the sphenoid sinus, such as the floor of the sphenoid sinus, pterygoid process, and clivus [
56]. The brain CT and MRI findings are crucial for diagnosis of arrested pneumatization. On brain CT, it appears as a non-eroded, non-expansile lesion with curvilinear calcification and with sclerotic margins. On brain MRI, the lesion contains internal fat and microcysts, and no mass effect [
589]. In T1-weighted MRI, the internal fat appears as high-signal, and a low-signal microcyst without enhancement. On T2-weighted MRI, the microcyst is hyperintense. In addition, the best marker of non-expansile nature of arrested pneumatization on brain CT and MRI is that there is no displacement or morphological disruption in the vidian canal and inferior orbital sinus [
10].
Arrested pneumatization should be differentiated from variable skull base lesions as in our 2 cases. Differential diagnosis of arrested pneumatization include fibrous dysplasia, ossifying fibroma, hemangioma, chordoma, chondrosarcoma, metastasis, and osteomyelitis. Discussing the typical radiological findings of arrested pneumatization are of great help in differentiating arrested pneumatization from other diseases, which can reduce unnecessary examinations such as surgical biopsies. Characteristic radiological findings in arrested pneumatization include sclerotic, well-circumscribed margins, non-expansile lesion, internal fat component, internal curvilinear calcification, no destruction of surrounding structures, and no enhancement of contrast [
5]. The lesion must be located at a site of normal or accessory pneumatization.
Fibrous dysplasia usually shows a ground-glass marrow pattern on CT and is expansile, therefore often compressing the surrounding neural foramen, allowing differentiation from arrested pneumatization [
589]. Ossifying fibroma is another expansile lesion and non-fat containing lesion. Intraosseous hemangioma is an expansile lesion with marked enhancement. Chordomas and chondrosarcomas are very destructive and expansile. Metastasis is markedly enhanced in contrast to the arrested pneumatization without enhancement. Osteomyelitis has decreased signal intensity on T1-weighted MRI.
In our patients, surgery was not required. The accurate diagnosis of arrested pneumatization was achieved through characteristic brain CT and MRI without pathological examination. A good understanding and a close examination of the images can lead to the correct diagnosis of arrested pneumatization.
In conclusion, we report rare 2 cases of arrested pneumatization of the sphenoid sinus in the greater sphenoid bone and clivus, respectively, which are often misdiagnosed as a serious disease in the skull base. An accurate brain CT and MRI review is essential to differentiate arrested pneumatization of the sphenoid sinus from other skull base diseases. The diagnosis of arrested pneumatization of the sphenoid sinus should be considered if a soft tissue lesion with a non-eroded, non-expansile nature, and sclerotic boundary in the skull base has internal fat on brain MRI.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download