Abstract
Unexpected bleeding is a common complication that can occur during surgery. This unexpected bleeding can be managed by checking the patients' preoperative hemodynamic state or by autologous transfusion of an appropriate volume during surgery depending on the amount of blood loss and hemodynamic condition. However, patients like Jehovah's Witnesses, who refuse autologous transfusions for religious reasons even in life-threatening situations, present a predicament for treating physicians. The author reports on a large meningioma on the posterior fossa of a Jehovah's Witness patient who underwent surgery without autologous blood transfusion. There were no major problems other than the fear of unexpected massive bleeding. The surgeon's attention and efforts to minimize bleeding during surgery seemed to be the most important factors for success.
Unexpected bleeding is a common complication that can occur during surgery. This unexpected bleeding can be managed by checking the patients' preoperative hemodynamic state or by autologous transfusion of an appropriate volume during surgery depending on the amount of blood loss and hemodynamic condition [1]. In cases of surgery in which massive bleeding is expected, blood can be prepared in advance to anticipate the possible risks to the patient. However, patients like Jehovah's Witnesses, who refuse to receive autologous transfusions for religious reasons even in life-threatening situations, present a predicament for the treating surgeon and anesthesiologist [2]. Therefore, to reduce the conflict between doctors and patients, the “Hospital Liaison Committee for Jehovah's Witnesses” recommends acute normovolemic hemodilution or intraoperative blood cell salvage as an alternative method to autologous transfusion. However, Jehovah's Witnesses make personal decisions on what they can accept in good conscience [3]. Therefore, it is important to discuss in advance what alternative products or procedures are acceptable to each patient. The author reports and reviews the related contents of a large meningioma on the posterior fossa of a Jehovah's Witness patient who underwent surgery without autologous blood transfusions.
The study was approved by the Institute Ethical Committee and in compliance with institute's requirements (202011004). A 67-year-old man was admitted with a 1-month history of dizziness and gait disturbance. He was 175 cm tall and 67 kg in weight and was taking hypertension drugs. Preoperative evaluations including electrocardiogram, cardiac sonography, pulmonary function test, and chest radiography revealed no abnormalities. Three days before surgery, laboratory evaluation revealed a normal hemoglobin concentration of 15.9 (normal range: 13–18 g/dL), hematocrit of 40% (36–48%), activated partial thromboplastin time of 29.3 seconds (23–35 seconds), prothrombin time of 107% (70–120%), international normalization ratio of 0.96 (0.92–1.17), and a platelet count of 230,000/µL (140,000–400,000/µL). The patient did not receive medication that may have impaired hemostasis or platelet function. Cranial MRI revealed a strong homogeneous contrast-enhancing mass with a broad base in the tentorium of the left posterior fossa. The tumor measured 55×50×50 mm and was compressing the fourth ventricle. The tumor showed increased relative cerebral blood volume on perfusion MRI (Fig. 1). An angiogram of the left external carotid artery revealed diffuse tumor straining supplied by the posterior branch of the middle meningeal artery and posterior auricular artery. The venous phase of the left internal carotid artery revealed left transverse and straight sinus occlusion due to a large tumor and normal venous drainage through the dominant right transverse sinus (Fig. 2). Before the operation, the patient asked the doctors to refuse blood transfusion; thus, the doctors decided not to perform the transfusion. Since the patient's health was good before surgery and the various preoperative evaluations including laboratory findings were normal, after full consultation, the patient and his family decided to use only blood-free volume expansion without performing acute normovolemic hemodilution. The anesthesiologist performed hypotensive anesthesia and the patient's systolic blood pressure was maintained at 80–90 mm Hg and the mean arterial blood pressure was maintained at 55–65 mm Hg during the operation. The patient's heart rate was maintained between 70 and 100 beats per minute. Surgical removal of the mass via left suboccipital craniectomy was performed in the prone position (Simpson II). The authors performed the surgery with great care and tried to minimize bleeding by performing hemostasis in the bleeding area quickly and thoroughly. The operation time was 7 hours and the intraoperative course was uneventful. Postoperative laboratory evaluation revealed a hemoglobin concentration of 12.8 g/dL, hematocrit of 37.3%, and platelet count of 194,000/µL. The histological diagnosis was transitional meningioma. The postoperative course was uneventful and the patient was discharged without any neurological defect 10 days after the operation. MRI performed 6 months after the operation revealed that the meningioma had been removed completely and no recurrence was observed (Fig. 3). The patient has been doing well in the 1 year since the operation.
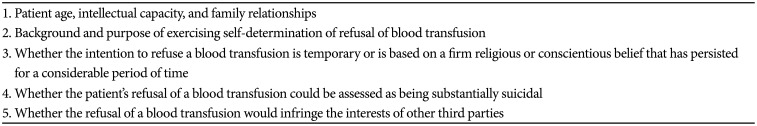
The most important purpose of blood transfusion during surgery is to supply adequate oxygen to major organs through the stabilization of hemoglobin levels [14]. Treatment of acute bleeding during surgery consists of maintaining intravascular volume [4]. Moderate blood loss of up to 20% of the total blood volume is managed by replacing the crystalloid such as Hartmann's solution and/or colloid solutions such as gelatin solution, dextran, and hydroxyethyl starches. Autologous blood is usually transfused in cases of severe blood loss [13]. Although blood-free volume expansion is administered to temporarily increase the effective circulating volume in the early stage of the shock caused by acute bleeding, the transfusion of blood and blood components is required to increase oxygen supply to the peripheral tissues in cases of massive bleeding [4]. On the premise of the intact compensatory mechanism of the cardiovascular system, young patients generally tolerate a hemoglobin value of 6–7 g/dL, while elderly patients can tolerate a value of 8–9 g/dL as a lower limit [5]. Hemoglobin values of 4.5–5 g/dL are critical and require urgent replacement [6]. However, in patients who refuse blood for religious reasons, such as Jehovah's Witnesses, the transfusion of autologous blood is not possible. This refusal of blood transfusions by patients who are Jehovah's Witnesses causes a conflict between the physician's duty to save the patient's life and the obligation to respect the patient's self-determination and religious freedom [2]. In the past, there seems to have been prejudice not only in the medical profession but also in the Korean legal profession that the duty of life-saving doctors is more important than the patient's self-determination and religious conviction. However, as the Korean Supreme Court precedents show, the prejudice of the past legal profession to prioritize life unconditionally seems to be gradually shifting toward respecting the self-determination of Jehovah's Witnesses. On June 26, 2014, the Korean Supreme Court presented five criteria to be determined in the event of a conflict between the obligations to respect the patient's right to self-determination and to protect the patient's life and recommended that these criteria be applied in the event of a similar lawsuit in the first-line lower court (Table 1) [7].
When a Jehovah's Witnesses patient in need of surgery refuses blood transfusion, several possible alternatives to transfusion should be considered [2]. The position of “Hospital Liaison Committee for Jehovah's Witnesses” on allogeneic and autologous blood does not accept whole blood (e.g., red cells, white cells, platelets, and plasma) from allogeneic blood and preoperative autologous blood collection and storage for later reinfusion using autologous blood. Fractions from red cells (e.g., hemin and hemoglobin), white cells, platelets, and plasma (e.g., albumin, clotting factors, fibrinogen, and immunoglobulins) from allogeneic blood and acute normovolemic hemodilution, dialysis, cardiopulmonary bypass, and blood salvage using autologous blood are potentially acceptable [3]. Jehovah's Witnesses have a worldwide network of more than 1,700 Hospital Liaison Committees. This network provides information on clinical strategies to avoid blood transfusion and facilitates access to health care for patients who are Jehovah's Witnesses. They may also help to minimize ethical conflicts related to medical care among patients who are Jehovah's Witnesses or their clinicians [3].
Suess et al. [2] examined whether the refusal of blood transfusion affected the surgical indications for neurosurgery and whether morbidity and mortality rates were higher after neurosurgical interventions in 103 Jehovah's Witness patients. In surgery for spinal disorders, the blood loss in Jehovah's Witnesses was a mean of 34.5% less than that in the control group. The changes in hemoglobin and hematocrit during spinal surgery were also significantly smaller in Jehovah's Witness patients. The mean intraoperative blood loss in intracranial surgery was significantly lower by 39.5% in Jehovah's Witnesses compared to the control group. The changes in hemoglobin and hematocrit during intracranial surgery were also significantly smaller in Jehovah's Witness patients. Surgical times were 17.5 minutes longer in spinal interventions and 36.7 minutes longer in intracranial interventions than those in the control groups. These results showed that neurosurgeons paid more attention to hemostasis and made efforts to minimize bleeding when operating on Jehovah's Witness patients. In other words, these results suggest that the decreased intraoperative blood loss by 34.5% in spinal surgery and 39.5% in intracranial surgery were reduced only by the efforts of intraoperative physicians to achieve hemostasis. Similarly, in the present case, since the author paid great attention to hemostasis while trying to minimize tissue damage during surgery, there was no significant decrease in the hemoglobin value after surgery, although surgery time took a little longer. Suess et al. [2] also reported no statistically significant increase in morbidity or mortality for Jehovah's Witnesses and, therefore, concluded that the risk was not higher when Jehovah's Witnesses underwent microsurgical techniques and received extensive anesthetic monitoring during neurosurgery.
In the operation of Jehovah's Witnesses who refuse to receive allogenic transfusions, it is necessary to determine if there are conditions for bloodless surgery, and various alternatives to allogeneic transfusions should be considered. The generally accepted alternatives to allogenic transfusion are surgical aids to minimize bleeding (clipping, electrocautery, laser, embolization, and tissue adhesives), anesthesia aids to minimize bleeding during surgery (hypotension, hypothermia, normovolemic hemodilution, and intraoperative monitoring techniques), proper use of hemostatic agents, bloodless volume expansion (clloids and crystalloids), and preoperative treatment of anemia (recombinant human erythropoietin, folic acid, and vitamin B12) [2]. Normovolemic hemodilution is known to be useful in surgery for Jehovah's Witness, where moderate to severe bleeding is expected [89]. Normovolemic hemodilution can be applied when the hematocrit level is higher than 34% and the expected intraoperative bleeding is more than 1000 mL. It is contraindicated in severe anemia with a hematocrit level of less than 30% [9]. However, the importance of open and continuous communication between physicians and patients is very important because the final decision depends on the patient's personal judgment. In this case, the patient wanted not to perform normovolemic hemodilution if possible. Therefore, the author did not perform normovolemic hemodilution considering the patient's good general condition. The author focused on surgical and anesthesiological aids to minimize intraoperative bleeding. The surgeon minimized the intraoperative bleeding through careful manipulation. However, preoperative embolization was not performed because it was judged not to be of great help because the tumor was not stained strongly in preoperative angiograms. In this case, induced hypotensive anesthesia was also used as one of the anesthesiological aids to minimize intraoperative bleeding. Several studies have reported that induced hypotension reduces the surgical bleeding and reduces need for blood transfusion [10]. Blood-free volume expansion was used through thorough intraoperative monitoring. Because hypothermia can increase bleeding by inhibiting the function of blood coagulation factors and platelets, we tried to maintain normal body temperature in this case [11].
In conclusion, the present case experienced no major problems other than the fear of unexpected massive bleeding. Although bloodless surgery cannot completely replace blood transfusion itself, there seems to be no definite contraindication for Jehovah's Witnesses requiring neurosurgical treatment. The surgeon's attention and efforts to minimize bleeding during surgery seem to be the most important factors related to success.
References
1. Goodnough LT, Brecher ME. Autologous blood transfusion. Intern Med. 1998; 37:238–245. PMID: 9617857.
2. Suess S, Suess O, Brock M. Neurosurgical procedures in Jehovah's Witnesses: an increased risk? Neurosurgery. 2001; 49:266–272. discussion 272-3. PMID: 11504102.
3. Watch Tower Bible and Tract Society of Pennsylvania. Hospital Liaison Committees for Jehovah's Witnesses. New York, NY: Watch Tower Bible and Tract Society of Pennsylvania;2012. Accessed October 21, 2020. at https://www.jw.org/en/medical-library/strategies-downloads/hospital-liaison-committees-jehovahs-witnesses/.
4. American Society of Anesthesiologists Task Force on Perioperative Blood Management. Practice guidelines for perioperative blood management: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Management. Anesthesiology. 2015; 122:241–275. PMID: 25545654.
5. Spence RK. Surgical red blood cell transfusion practice policies. Am J Surg. 1995; 170(6 Suppl 1):S3–S15.
6. Carson JL. Morbidity risk assessment in the surgically anemic patient. Am J Surg. 1995; 170(6 Suppl 1):S32–S36.
7. Supreme Court of Korea. Jehovah's Witnesses Death During Bloodless Surgery. Seoul: Supreme Court of Korea;2014. Accessed September 9, 2020. at https://www.scourt.go.kr/portal/news/NewsViewAction.work?seqnum=4557&gubun=4&searchOption=&searchWord=.
8. Lindstrom E, Johnstone R. Acute normovolemic hemodilution in a Jehovah's Witness patient: a case report. AANA J. 2010; 78:326–330. PMID: 20879634.
9. Yang SA, Park SW, Kim KS. Acute normovolemic hemodilution in Jehovah's Witness. J Kyung Hee Univ Med Cent. 2015; 30:74–77.
10. Lin S, McKenna SJ, Yao CF, Chen YR, Chen C. Effects of hypotensive anesthesia on reducing intraoperative blood loss, duration of operation, and quality of surgical field during orthognathic surgery: a systematic review and meta-analysis of randomized controlled trials. J Oral Maxillofac Surg. 2017; 75:73–86. PMID: 27542543.
11. Michelson AD, MacGregor H, Barnard MR, Kestin AS, Rohrer MJ, Valeri CR. Reversible inhibition of human platelet activation by hypothermia in vivo and in vitro. Thromb Haemost. 1994; 71:633–640. PMID: 7522354.
Fig. 1
(A) Gadolinium-enhanced axial and (B) sagittal MRI showing strong a homogeneous contrast-enhancing mass with a broad base in the tentorium of the left posterior fossa. C: The tumor shows increased relative cerebral blood volume on perfusion MRI.
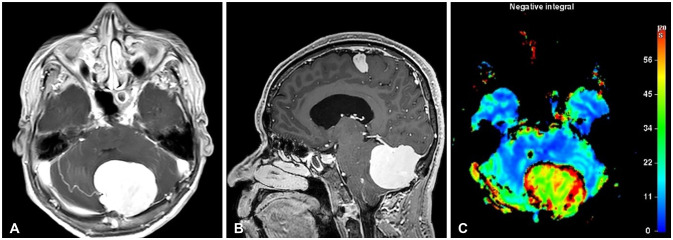
Fig. 2
A: Left external carotid artery angiogram showing diffuse tumor straining and supply by the posterior branch of the middle meningeal and posterior auricular arteries. B: The venous phase of the left internal carotid artery shows left transverse and straight sinus occlusion due to the large tumor and normal venous drainage through the dominant right transverse sinus.
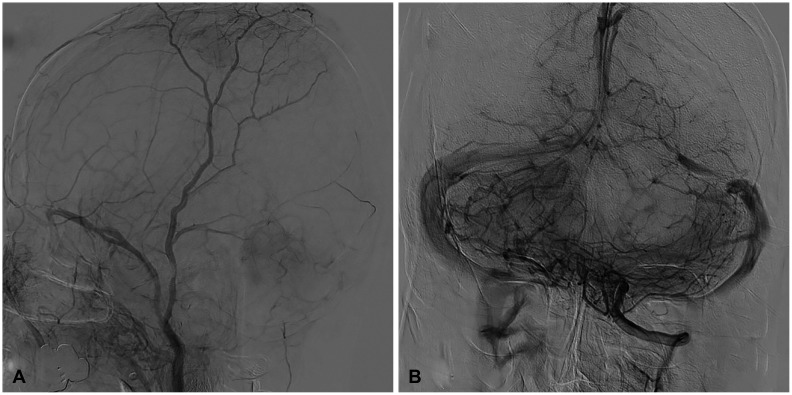
Fig. 3
(A) Gadolinium-enhanced sagittal and (B) coronal MRI obtained 6 months after operation showing that the meningioma had been completely removed and without recurrence.
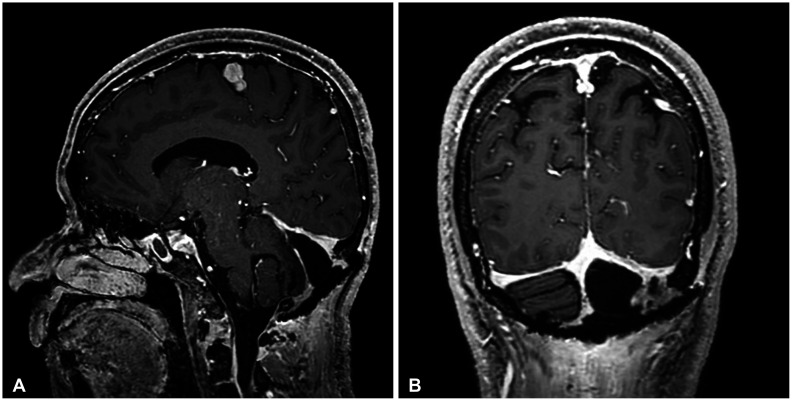
Table 1
On June 26, 2014, the Korean Supreme Court decided whether the right to self-determination of patients who refused blood transfusion would be evaluated as having the same value as life, considering the following five criteria




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download