Abstract
A 42-year-old man presented with a headache and right hemiparesis and was found to have a cystic mass with a calcified mural nodule in the left thalamus. Because the thalamus is surrounded by vital neurovascular structures, the surgical approach to thalamic lesions can be challenging. We decided to remove the mass for decompression and pathological diagnosis. The mass was removed through a contralateral interhemispheric transcallosal transchoroidal approach with less retraction and parenchymal injury than other approaches to avoid brain retraction and cortical injury. The pathological diagnosis was cavernous malformation. Temporary worsening of the preoperative hemiparesis was recovered over two months following surgery. Tolerable thalamic pain syndrome remained. Here, we report a rare case of thalamic cavernous malformation with a favorable outcome through a contralateral surgical approach.
The thalamus is an eloquent structure located in the center of the lateral ventricles rostral to the brainstem. Because it is surrounded by vital neurovascular structures, the surgical approach to the thalamus can be challenging. In the past, the outcome of surgical treatment for a thalamic tumor was poor and these lesions were often considered inoperable. However, contemporary microsurgical techniques together with improvements in neuroimaging that enable accurate presurgical planning, allow for the performance of safer resections. Gliomas and cavernous malformation are considered to be surgically accessible lesions of thalamic masses. The decision on whether to operate on any individual lesion depends upon the specific location of the lesion within the thalamus, the nature of the patient's symptoms, and the patient's history. The basic principle in selecting the surgical approach is to provide a trajectory that does not violate any eloquent structures such as the corticospinal tract or the thalamus [1]. Here, we report and review a case of thalamic cavernous malformation with a favorable outcome through the contralateral interhemispheric transcallosal approach.
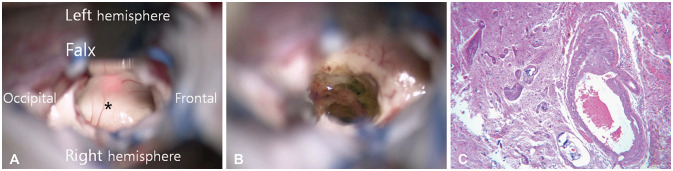
A 42-year-old man presented to our department with the sudden onset of headache under progressive right hemiparesis and hemihypesthesia. Neurological evaluation revealed decreased grasping power of the right hand and paresthesia of the right arm. The laboratory findings were normal. CT showed a cystic mass with fluid-fluid level and a calcified nodule at the left thalamus and obstructive hydrocephalus with signs of increased intracranial pressure (Fig. 1A). Brain MRI showed about a 50×30×30-mm-sized lobulated cyst with a fluid-fluid level, a focal peripheral calcified nodule, and subtle enhancement in the left thalamus (Fig. 1B–D). The cystic mass compressed the third ventricle and left basal ganglia. The differential diagnoses of the radiological findings were cavernous malformation, neurocysticercosis, and low-grade glioma. Based on the clinical and radiological features, we decided to remove the mass through a contralateral interhemispheric transcallosal transchoroidal approach that had more advantages than other proven approaches to thalamic lesions (Fig. 2A and B). The patient was placed in the supine oblique position with head elevation. After head fixation, the sagittal plane was aligned parallel to the floor with the superior placement of the left hemisphere to reduce brain retraction of the right hemisphere by gravity. After making a curvilinear scalp incision along the coronal suture, craniotomy crossing the midline sagittal sinus was performed two-thirds in front and one-third behind the coronal suture, as in the usual anterior interhemispheric approach. Opening of the interhemispheric fissure to reveal the corpus callosum was performed with less retraction of the ipsilateral hemisphere with the assistance of gravity. With the use of neuronavigation, the ideal trajectory was identified to expose the contralateral ventricle with the lesion. We discerned the orientation of the thalamostriate and septal veins to confirm entry into the left lateral ventricle with the thalamic lesion. We found and dissected the discolored swollen ependymal surface just lateral to the choroid plexus on the floor of the left lateral ventricle. As much of the cyst with xanthochromic fluid and the calcified mass was removed as possible (Fig. 3A and B). Inferomedial cystic wall was retained to prevent injury to the eloquent structures. The temporary aggravation of preoperative hemiparesis and hemiparesthesia was noted after surgery and recovered over two months following surgery. A postoperative CT showed the total removal of the calcified nodule and a decreased extent of hydrocephalus. A follow-up MRI showed a small cyst with a hemosiderin rim opening into the ipsilateral lateral ventricle (Fig. 2C and D). Pathology revealed cavernous malformation (Fig. 3C).
The thalamus is in a critical location near the internal capsule, basal ganglia, midbrain, and several important neurovascular structures. The anatomical location makes surgery on thalamic lesions more difficult compared to other intracranial locations. Accordingly, there remains much debate over the optimal treatment of thalamic lesions, which ranges from conservative management to open surgery. The decision on whether to operate on any thalamic lesion depends upon the specific location of the lesion within the thalamus, the nature of the thalamic lesion, and the patient's clinical manifestations [1]. Thalamic lesions have corresponding surgical approaches to each specific location within the thalamus. Different surgical approaches for each part of the thalamus include the orbitozygomatic approach to the anteroinferior thalamus, the anterior interhemispheric transcallosal approach to the medial thalamus, the anterior contralateral interhemispheric transcallosal approach to the lateral thalamus, the posterior interhemispheric transcallosal approach to the posterosuperior thalamus, and the parieto-occipital transventricular approach to the lateral posteroinferior thalamus [1]. The most important consideration in the choice of the surgical approach is the relationship of the tumor to eloquent structures such as the internal capsule and corticospinal tract [2]. The basic principle guiding the selection of one of these approaches is to provide a trajectory that does not violate any eloquent structures [3]. The surgical approach should be tailored to the individual according to the location of the lesion, the patient's symptoms, and the existence of hydrocephalus. Ventricular size is an important parameter that must be considered in choosing a surgical approach. The location of the lesion in relation to the ependymal or pial surface should also be considered when deciding upon a surgical approach.
The transcortical transventricular approach is popular for the resection of periventricular lesions. However, the transcortical transventricular approach destroys normal brain tissue to increase the risk of postoperative deficits from lesions located adjacent to critical anatomical structures such as the basal ganglia or internal capsule. Several reports indicated a higher incidence of seizures in patients who underwent the transcortical approach. In contrast, the interhemispheric transcallosal approach takes advantage of the interhemispheric fissure, allowing deep access and requiring only a small amount of normal tissue resection. The interhemispheric transcallosal approach to thalamic lesions has both ipsilateral and contralateral interhemispheric approaches according to the interhemispheric direction.
The ipsilateral interhemispheric approach is for lesions closer to the midline because less retraction is needed to remove the lateral mass. Conversely, eccentric lesions are best approached through the contralateral interhemispheric approach because it provides a trajectory that avoids injury to eloquent structures by greater retraction and a lower chance of remnants [4]. In a series by Rangel-Castilla and Spetzler [5], the thalamus was divided into six regions, each with its corresponding preferred surgical approach. Of these, the anterior contralateral interhemispheric transcallosal approach was the most commonly used approach [1].
Preoperative imaging in our case demonstrated that the cystic wall appeared to have reached the pial surface superior to the floor of the ipsilateral lateral ventricle and medial to the third ventricle. Hydrocephalus in our case made the surgical trajectory easier by the displacement of eloquent structures. The calcified solid component of the thalamic cavernous malformation was at the lateral part of the thalamus. It was difficult to see and remove the calcified mass without excessive retraction in the ipsilateral interhemispheric approach. To avoid excessive retraction in the ipsilateral hemisphere, we selected the contralateral trajectory instead of the ipsilateral trajectory. Head positioning could also affect exposure due to gravity-assisted brain shift. The sagittal plane of the head was parallel to the floor with the superior placement of the lesion. During the interhemispheric dissection, the gap between the right hemisphere and the falx could be opened with minimal hemispheric retraction and the assistance of gravity. The fixed retractor was placed against the falx to secure further exposure of the contralateral corpus callosum and lateral ventricle with the thalamic lesion. This approach allowed us to use the direct visualization of reliable anatomic landmarks to verify the accuracy of the image guidance. A contralateral interhemispheric craniotomy is a useful approach for many different surgical pathologies, including tumors, cysts, and arteriovenous malformations [6]. In low-grade gliomas, radical resection in a single or staged procedure can be curative without complementary treatment. Recurrence or residual regrowth can be safely managed surgically. However, in high-grade tumors, the role of radical or partial resection remains a matter of debate [2].
Cavernous malformations commonly arise in the cerebral subcortex or the cerebral white matter but are rarely found in the thalamus [7]. Thalamic cavernous malformations are relatively rare deep-seated lesions that can cause significant neurologic morbidity and mortality. The presentation of thalamic lesions includes headache, motor deficits, sensory deficits, hemorrhage, hydrocephalus, and seizures [4]. Both lesion enlargement and extralesional bleeding can cause neurological deficits even from minor morphological changes. In the largest series of thalamic cavernous malformations reported to date, 59% of the patients presented with hemorrhage, and 11% presented with hydrocephalus [8]. Dorsal or medial thalamic cavernous malformations have a higher chance of causing obstructive hydrocephalus after enlargement or bleeding [9]. The patient in our case visited the emergency department with the sudden onset of headache and gait disturbance during progressive motor and sensory deficits of the contralateral extremities. We suggested that obstructive hydrocephalus had developed by compression of the third ventricle from enlargement of the thalamic mass. Fortunately, hydrocephalus gave us a surgical trajectory to escape the injury of neighboring neurovascular structures. The benefits of operating on cavernous malformations such as the elimination of re-hemorrhage risk must be weighed against the risk of worsening neurological deficits by surgery [10]. Initially, conservative management was suggested for patients who had incidental lesions, especially asymptomatic lesions. The yearly rebleeding incidence of cavernous malformations without surgical intervention was 2% for incidental lesions and 7% for symptomatic lesions. Therefore, the outcomes after conservative treatment were worse than after microsurgery [9]. Poor outcomes were reported for radiosurgery for thalamic cavernous malformation, with a yearly rebleeding incidence of 8% and a 22.2% morbidity [9]. A reduced hemorrhage rate was reported for some patients after radiosurgery, but many studies did not support it as an effective therapy.
Therefore, cavernous malformations with progressive enlargement that results in a progressive neurological decline might require more aggressive treatment. Surgical resection remains an option for thalamic cavernous malformations. The neurosurgeon must consider a wide variety of factors in deciding whether surgery is the best option, in particular, the number of times the lesion has bled and the time of surgery [11]. Clinical presentation, location within the thalamus, natural history, and surgical morbidity must be taken into account when deciding on a management strategy [1]. Of these, the anterior contralateral interhemispheric transcallosal approach was the most commonly used approach. Because our case had a major calcified component of the mass in the lateral thalamus, we selected the contralateral trajectory over the ipsilateral trajectory to avoid excessive retraction in the ipsilateral hemisphere. Our surgical experience with thalamic cavernous malformations demonstrated that favorable results can be achieved with adequate exposure and safe microsurgical resection by contralateral approach.
Notes
AUTHOR CONTRIBUTIONS:
Conceptualization: Seung Heon Cha.
Data curation: Seung Heon Cha, Tak Gun Jang.
Formal analysis: Seung Heon Cha, Tak Gun Jang.
Funding acquisition: Seung Heon Cha.
Investigation: Tak Gun Jang, Won Ho Cho.
Methodology: Tak Gun Jang, Won Ho Cho.
Supervision: Seung Heon Cha, Won Ho Cho.
Writing–original draft: Seung Heon Cha, Tak Gun Jang.
Writing–review & editing: Tak Gun Jang, Won Ho Cho.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
References
1. Sarris CE, Atwal GS, Nakaji P. Thalamic cavernous malformations. Handb Clin Neurol. 2017; 143:297–302. PMID: 28552153.
2. Cinalli G, Aguirre DT, Mirone G, et al. Surgical treatment of thalamic tumors in children. J Neurosurg Pediatr. 2018; 03. 21:247–257. PMID: 29271729.
3. Kumar A, Sharma R, Garg A, Sharma BS. Contralateral anterior interhemispheric transparaterminal gyrus approach for thalamopeduncular pilocytic astrocytoma in an adult: technical report. World Neurosurg. 2016; 87:21–25. PMID: 26409092.
4. Zaidi HA, Chowdhry SA, Nakaji P, Abla AA, Spetzler RF. Contralateral interhemispheric approach to deep-seated cavernous malformations: surgical considerations and clinical outcomes in 31 consecutive cases. Neurosurgery. 2014; 75:80–86. PMID: 24618803.
5. Rangel-Castilla L, Spetzler RF. The 6 thalamic regions: surgical approaches to thalamic cavernous malformations, operative results, and clinical outcomes. J Neurosurg. 2015; 123:676–685. PMID: 26024002.
6. Schwartz C, Grillhösl A, Schichor C, et al. Symptomatic cavernous malformations of the brainstem: functional outcome after microsurgical resection. J Neurol. 2013; 260:2815–2822. PMID: 23974645.
7. Otani N, Fujioka M, Oracioglu B, et al. Thalamic cavernous angioma: paraculminar supracerebellar infratentorial transtentorial approach for the safe and complete surgical removal. Acta Neurochir Suppl. 2008; 103:29–36. PMID: 18496942.
8. Lanzino G, Wanebo JE, Spetzler RF. Contralateral interhemispheric resection of thalamic cavernous malformations with frameless stereotaxy. Operat Tech Neurosurg. 2002; 5:191–197.
9. Mathiesen T, Edner G, Kihlström L. Deep and brainstem cavernomas: a consecutive 8-year series. J Neurosurg. 2003; 99:31–37. PMID: 12854740.
10. Li D, Zhang J, Hao S, et al. Surgical treatment and long-term outcomes of thalamic cavernous malformations. World Neurosurg. 2013; 79:704–713. PMID: 22381871.
11. Pandey P, Westbroek EM, Gooderham PA, Steinberg GK. Cavernous malformation of brainstem, thalamus, and basal ganglia: a series of 176 patients. Neurosurgery. 2013; 72:573–589. discussion 588–9. PMID: 23262564.
Fig. 1
Preoperative radiologic findings. A: CT scanning shows a cystic mass with peripheral calcified nodule at left thalamus and hydrocephalus. B: T2-weighted MR axial image shows a lobulated cyst with fluid-fluid level and obstructive hydrocephalus. C: T1-weighted MR axial image shows a lobulated cyst with peripheral high signal mass. D: T1-weighted enhanced MR axial image shows subtle enhanced cystic mass at left thalamus.

Fig. 2
Postoperative radiologic findings. A: Surgical trajectory of contralateral interhemispheric transcallosal approach (red arrows) on T2-weighted MR coronal image. B: Postoperative CT coronal image shows contralateral callosotomy and ventricular catheter through the surgical route. C and D: Postoperative follow-up MRI shows removal of solid component and disappearance of mass effect without any neurovascular injury.

Fig. 3
Operative and pathologic findings. A: The floor of left lateral ventricle (asterisk) was upward displaced by thalamic mass. B: Gliosis and hemosiderin deposits are seen along the margin of cavernous malformation. C: Microscopic finding shows some abnormal shaped vessels that are consistent with cavernous malformation (hematoxylin & eosin, ×100).




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download