1. Champeaux C, Wilson E, Brandner S, Shieff C, Thorne L. World Health Organization grade III meningiomas. A retrospective study for outcome and prognostic factors assessment. Br J Neurosurg. 2015; 29:693–698. PMID:
26098606.
2. Champeaux C, Dunn L. World Health Organization grade II meningioma: a 10-year retrospective study for recurrence and prognostic factor assessment. World Neurosurg. 2016; 89:180–186. PMID:
26850975.
3. Champeaux C, Houston D, Dunn L. Atypical meningioma. A study on recurrence and disease-specific survival. Neurochirurgie. 2017; 63:273–281. PMID:
28882609.
4. Gavrielov-Yusim N, Friger M. Use of administrative medical databases in population-based research. J Epidemiol Community Health. 2014; 68:283–287. PMID:
24248997.
5. Tuppin P, Rudant J, Constantinou P, et al. Value of a national administrative database to guide public decisions: from the système national d'information interrégimes de l'Assurance Maladie (SNIIRAM) to the système national des données de santé (SNDS) in France. Rev Epidemiol Sante Publique. 2017; 65 Suppl 4:S149–S167. PMID:
28756037.
6. Champeaux C, Weller J, Katsahian S. Epidemiology of meningiomas. A nationwide study of surgically treated tumours on French medico-administrative data. Cancer Epidemiol. 2019; 58:63–70. PMID:
30481723.
7. Champeaux-Depond C, Constantinou P, Weller J. Cause-specific survival after meningioma surgery: a nationwide population-based competing risk study. World Neurosurg. 2021; 146:e67–e75. PMID:
33096279.
8. Champeaux-Depond C, Weller J, Resche-Rigon M. Neurofibromatosis type 2: a nationwide population-based study focused on survival after meningioma surgery. Clin Neurol Neurosurg. 2020; 198:106236. PMID:
33002675.
9. Champeaux-Depond C, Weller J, Froelich S, Resche-Rigon M. A nationwide population-based study on overall survival after meningioma surgery. Cancer Epidemiol. 2020; 70:101875. PMID:
33360358.
10. Constantinou P, Tuppin P, Fagot-Campagna A, Gastaldi-Ménager C, Schellevis FG, Pelletier-Fleury N. Two morbidity indices developed in a nationwide population permitted performant outcome-specific severity adjustment. J Clin Epidemiol. 2018; 103:60–70. PMID:
30016643.
11. Lang TA, Altman DG. Basic statistical reporting for articles published in biomedical journals: the “Statistical Analyses and Methods in the Published Literature” or the SAMPL guidelines. Int J Nurs Stud. 2015; 52:5–9. PMID:
25441757.
12. Nicholls SG, Quach P, von Elm E, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement: methods for arriving at consensus and developing reporting guidelines. PLoS One. 2015; 10:e0125620. PMID:
25965407.
13. Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957; 20:22–39. PMID:
13406590.
14. Florijn MA, Sharfo AWM, Wiggenraad RGJ, et al. Lower doses to hippocampi and other brain structures for skull-base meningiomas with intensity modulated proton therapy compared to photon therapy. Radiother Oncol. 2020; 142:147–153. PMID:
31522879.
15. Kaur G, Sayegh ET, Larson A, et al. Adjuvant radiotherapy for atypical and malignant meningiomas: a systematic review. Neuro Oncol. 2014; 16:628–636. PMID:
24696499.
16. Champeaux C, Jecko V, Houston D, et al. Malignant meningioma: an international multicentre retrospective study. Neurosurgery. 2019; 85:E461–E469. PMID:
30566646.
17. Jenkinson MD, Javadpour M, Haylock BJ, et al. The ROAM/EORTC-1308 trial: radiation versus observation following surgical resection of atypical meningioma: study protocol for a randomised controlled trial. Trials. 2015; 16:519. PMID:
26576533.
18. Detti B, Scoccianti S, Di Cataldo V, et al. Atypical and malignant meningioma: outcome and prognostic factors in 68 irradiated patients. J Neurooncol. 2013; 115:421–427. PMID:
24045968.
19. Vernimmen FJ, Harris JK, Wilson JA, Melvill R, Smit BJ, Slabbert JP. Stereotactic proton beam therapy of skull base meningiomas. Int J Radiat Oncol Biol Phys. 2001; 49:99–105. PMID:
11163502.
20. Boskos C, Feuvret L, Noel G, et al. Combined proton and photon conformal radiotherapy for intracranial atypical and malignant meningioma. Int J Radiat Oncol Biol Phys. 2009; 75:399–406. PMID:
19203844.
21. Gennatas ED, Wu A, Braunstein SE, et al. Preoperative and postoperative prediction of long-term meningioma outcomes. PLoS One. 2018; 13:e0204161. PMID:
30235308.
22. van Alkemade H, de Leau M, Dieleman EM, et al. Impaired survival and long-term neurological problems in benign meningioma. Neuro Oncol. 2012; 14:658–666. PMID:
22406926.
23. Champeaux C, Houston D, Dunn L, Resche-Rigon M. Intracranial WHO grade I meningioma: a competing risk analysis of progression and disease-specific survival. Acta Neurochir (Wien). 2019; 161:2541–2549.
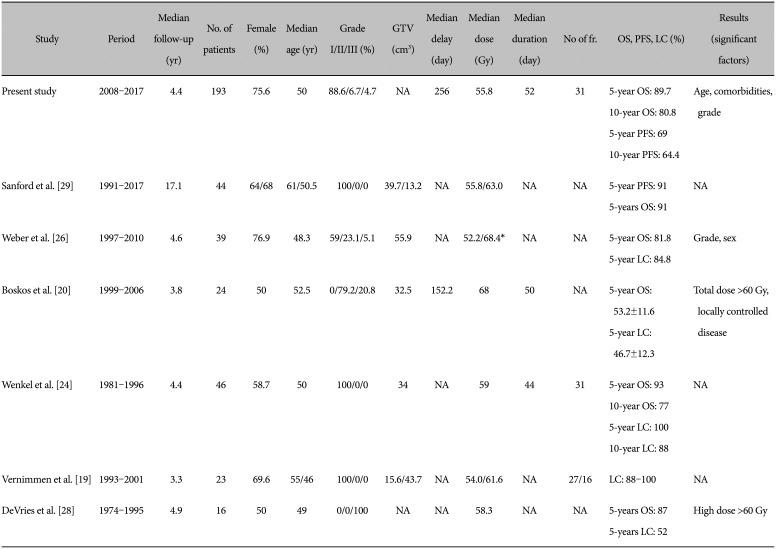
24. Wenkel E, Thornton AF, Finkelstein D, et al. Benign meningioma: partially resected, biopsied, and recurrent intracranial tumors treated with combined proton and photon radiotherapy. Int J Radiat Oncol Biol Phys. 2000; 48:1363–1370. PMID:
11121635.
25. Lesueur P, Calugaru V, Nauraye C, et al. Proton therapy for treatment of intracranial benign tumors in adults: a systematic review. Cancer Treat Rev. 2019; 72:56–64. PMID:
30530009.
26. Weber DC, Schneider R, Goitein G, et al. Spot scanning-based proton therapy for intracranial meningioma: long-term results from the Paul Scherrer Institute. Int J Radiat Oncol Biol Phys. 2012; 83:865–871. PMID:
22138457.
27. Hug EB, Devries A, Thornton AF, et al. Management of atypical and malignant meningiomas: role of high-dose, 3D-conformal radiation therapy. J Neurooncol. 2000; 48:151–160. PMID:
11083080.
28. DeVries A, Munzenrider JE, Hedley-Whyte T, Hug EB. The role of radiotherapy in the treatment of malignant meningiomas. Strahlenther Onkol. 1999; 175:62–67. PMID:
10065140.
29. Sanford NN, Yeap BY, Larvie M, et al. Prospective, randomized study of radiation dose escalation with combined proton-photon therapy for benign meningiomas. Int J Radiat Oncol Biol Phys. 2017; 99:787–796. PMID:
28865924.
30. El Shafie RA, Czech M, Kessel KA, et al. Evaluation of particle radiotherapy for the re-irradiation of recurrent intracranial meningioma. Radiat Oncol. 2018; 13:86. PMID:
29739417.
31. Woehrer A, Hackl M, Waldhör T, et al. Relative survival of patients with non-malignant central nervous system tumours: a descriptive study by the Austrian Brain Tumour Registry. Br J Cancer. 2014; 110:286–296. PMID:
24253501.
32. Burkhardt JK, Zinn PO, Graenicher M, et al. Predicting postoperative hydrocephalus in 227 patients with skull base meningioma. Neurosurg Focus. 2011; 30:E9.
33. Bir SC, Sapkota S, Maiti TK, Konar S, Bollam P, Nanda A. Evaluation of ventriculoperitoneal shunt-related complications in intracranial meningioma with hydrocephalus. J Neurol Surg B Skull Base. 2017; 78:30–36. PMID:
28180040.
34. Doyen J, Falk AT, Floquet V, Hérault J, Hannoun-Lévi JM. Proton beams in cancer treatments: clinical outcomes and dosimetric comparisons with photon therapy. Cancer Treat Rev. 2016; 43:104–112. PMID:
26827698.
35. Verma V, Mishra MV, Mehta MP. A systematic review of the cost and cost-effectiveness studies of proton radiotherapy. Cancer. 2016; 122:1483–1501. PMID:
26828647.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download