Abstract
Background
Modified orbitozygomatic craniotomy is characterized by simplicity and wide exposure. The purpose of the present study was to describe a modified orbitozygomatic approach without resecting the zygomatic arch for large parasellar tumor surgeries.
Methods
Between April 2016 and December 2019, seven patients with parasellar tumor underwent surgiest with a modified orbitozygomatic approach. Surgical procedures, clinical outcomes, and complications were analyzed.
Results
This study included 3 meningiomas, 2 pituitary adenomas, 1 chondrosarcoma, and 1 schwannoma. Modified orbitozygomatic craniotomy provides a wider surgical freedom in the opticocarotid and prechiasmatic cistern than frontotemporal craniotomy without orbitotomy, Total, subtotal, and partial resections were achieved for 3, 2, and 2 patients, respectively. Reasons for partial resections were tight adhesion to the carotid artery and encasing of the carotid artery. Permanent morbidities developed in one patient with 3rd nerve palsy and one patient with hemiparesis.
Conclusion
Modified orbitozygomatic approach can provide the shortest access to the interpeduncular cistern with a minimum brain retraction. Surgeons who experience surgical challenge during the conventional approach for parasellar tumor resection are recommended to learn the modified orbitozygomatic approach.
Skull base approach includes resection of the frontotemporal craniotomy, the roof, and the lateral wall of the orbit, the zygoma lateral surface, and the zygomatic process of the temporal bone. The use of the supraorbital craniotomy approach was introduced in 1982 [1]. Since then, a variety of similar modified approaches with orbital rim removal have been reported [234]. Orbitozygomatic approaches include those osteotomies performed as one-piece or two-piece [56]. The modified orbitozygomatic craniotomy is one variant used to treat vascular and tumorous lesions of parasellar regions [78].
Here, we report surgical experiences of a modified orbitozygomatic approach without resecting the zygomatic arch in 7 patients with skull base tumors.
Seven consecutive patients with various brain tumors underwent an operation via a modified orbitozygomatic approach from April 2016 to December 2019 by an experienced surgeon (SHY) at a single institution. Patients were placed supine with the bed head raised by 15° to facilitate venous drainage. The patient’s head was rotated 30° contralaterally and padding was placed beneath the ipsilateral shoulder. The head was fixed in a Mayfield headholder. A curvilinear scalp incision was made less than 1 cm anterior to the tragus along the hairline, which was terminated around the midline. Subfascial dissection of the temporalis muscle was performed to protect the temporal branch of the facial nerve. Burr holes were placed at the anatomical keyhole, directly behind the zygomatic process of the frontal bone, the temporal bone, and along the superior temporal line. The first cut carried on from the medial sphenoid wing and extended to the lateral orbital wall including the portion of zygoma root. The surgeon hold the reciprocating saw in a position parallel to the floor with protection along the frontal bone and periorbital. A tiny chisel under a microscope was helpful for safe cutting. A high-speed sidecut drill bit was used to cut the thick orbital rim (Fig. 1). The craniotomy including orbital osteotomy was removed in one piece (video clip at https://youtu.be/WrBrxq9EzNY). Anterior clinoidectomy and unroofing of the optic canal were performed when necessary. Intradural procedures was tailored based on tumor characteristics. The Institutional Review Board (IRB) of St. Vincent’s Hospital approved this study (VC21RISI0082) and this report was conducted according to the guidelines of the Declaration of Helsinki for biomedical research. The requirement of informed consent was waived due to its retrospective nature.
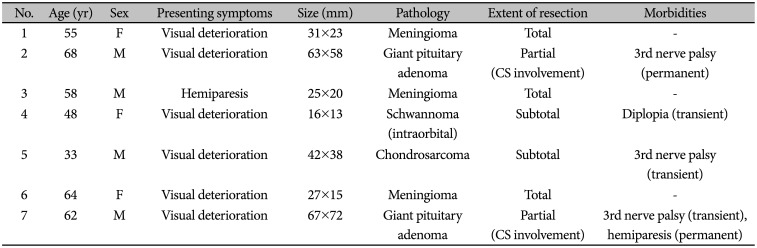
Characteristics of patients are summarized in Table 1. Seven patients (3 meningiomas, 2 pituitary adenomas, 1 schwannoma, and 1 chondrosarcoma) with an average age of 55.4 years (range, 33–68 years) were treated with a modified orbitozygomatic approach. The presenting symptoms were visual deterioration in 6 patients and motor weakness in 1. Total, subtotal, and partial resections were achieved in 3, 2, and 2 patients, respectively. Postoperatively, 3rd nerve palsy developed in 3 patients. One of them had permanent 3rd nerve palsy due to direct injury during removal of tumor involving the cavernous sinus. One patient developed hemiparesis caused by cerebral infarction of lenticulostriate arteries.
A 62-year-old male patient presented with visual deterioration. He developed gait disturbance and cognitive dysfunction recently. The visual acuity was 0.6 in the right eye and 0.2 in the left eye. On visual field examination, temporal side and defect total depression were noted in the right eye and the left eye, respectively. Preoperative MR images showed a large pituitary adenoma in sellar, suprasellar, and the third ventricle with encasement of the left internal carotid artery and hydrocephalus (Fig. 2). The patient underwent the modified orbitozygomatic approach. After sylvian dissection, compromised optic nerve was noted. The tumor was located beneath several perforators. The tumor located in the third ventricle was resected through a lamina terminalis approach. Basilar artery was noted without brain retraction following removal of the main lesion (Fig. 3). Postoperative MR images showed the removal of pituitary adenoma in sellar, suprasellar, and the third ventricle (Fig. 4). Postoperatively, she developed 3rd nerve palsy permanently. The injury of the oculomotor nerve was not detected intraoperatively. Hydrocephalus was improved immediately after the surgery.
Minimally invasive approach is now used in all major fields of surgery. Skull base approach is not an exception [910]. A modified orbitozygomatic approach provides simple working space without resecting the zygomatic arch. We performed orbitotomy in one piece combined with frontotemporal craniotomy. This is different from the conventional orbitozygomatic approach. It has been reported that an additional orbital rim resection can increase surgical exposure by 26% to 39% compared to the frontotemporal craniotomy alone [1112]. Removal of >3 cm of the zygomatic arch does not provide advantage in terms of exposure. However, it does increase the risk of atrophy of muscles that contribute to chewing. It also increases the risk of cosmetic defects. With radical drilling of the greater wing of the sphenoid bone, medial regions of the petrous temporal bone can be reached [12]. Anterior extradural clinoidectomy constitutes an expansion of the approach that enhances surgical access to the skull base and contributes to safe exposure of critical neurovascular elements such as the carotid artery and the optic nerve [13].
It has been noted that the surgical technique proposed cannot completely replace the conventional orbitozygomatic craniotomy. We suggest that a modified orbitozygomatic approach provide a short access to the interpeduncular cistern with a minimum brain retraction. We noticed that the angle to lesions of our approach was 1 cm to 3 cm lower than that with either a pterional or a subtemporal approach (Fig. 5). We prefer the one-piece orbitozygomatic craniotomy without reconstructing the resected roof of the orbit. Preservation of the periorbital tissue is mandatory. Neoplastic lesions arising in the anterior, middle cranial fossa, and petrous apex can be indicated for this approach. However, lesions involving infratemporal regions and middle to posterior fossa require the additional osteotomy. The two-piece orbitozygomatic craniotomy reported by Zabramski et al. [14] is an ideal procedure that can expose the skull base region widely without requiring an additional orbital resection. However, some surgeons, especially inexperienced ones, hesitate to use a two-piece orbitozygomatic craniotomy because of complicated surgical anatomy and technical difficulty [15]. Most difficulties were encountered during cuts around the superior orbital fissure and the inferior orbital fissure. We recommend final cuts to be made using both a high-speed drill and a tiny chisel under a microscope. A comparative study is necessary to analyze the surgical field amplitude, working angles, brain retraction degree, surgical time, and quality of life of patients.
The reason of partial resection was the presence of a mass in the cavernous sinus. Our patients with debilitating symptoms such as visual deterioration were offered an operation with the goal to decrease the mass effect. Invasive and adherent tumors present surgical challenges. Attempt at dissection or debulking of tumor from cranial nerves often result in damage to cranial nerves. In case 2 with postoperatively permanent 3rd nerve palsy, we noticed a discontinuation of the oculomotor nerve after debulking. It was very hard to see the nerve pathway because of displacement and spreading of the nerve compressed by the tumor [1617].
The rate of postoperative complications including temporary palsy was 62.5%. Permanent 3rd nerve palsy and hemiparesis developed in 1 patient each. However, none of these complications developed by our patients was affected by the technique of drilling or specifically by the surgical approach. Periorbital swelling occurred in the majority of patients. This was resolved with a few days after the procedure with rest and icing. There were no additional serious complications such as enophthalmos, pulsatile exophthalmos, or cosmetic defects.
Radical removal of parasellar tumor involves difficult surgical procedures. We recognized that the usefulness of a modified orbitozygomatic approach with a one-piece craniotomy was based on our experience in a small series. Further studies with a number of patients and surgeries performed by several surgeons are needed to validate and compare surgical advantages and disadvantages of the modified approach considering other variants of the orbitozygomatic approach.
Notes
Author Contributions:
Conceptualization: Seung Ho Yang.
Data curation: Young Il Kim.
Formal analysis: Il Sup Kim.
Funding acquisition: Seung Ho Yang.
Investigation: Jin Gu Kim.
Methodology: Young Il Kim.
Project administration: Dong Hoon Lee.
Resources: Jae Hoon Sung.
Software: Dong Hoon Lee.
Supervision: Jae Hoon Sung.
Validation: Seung Ho Yang.
Visualization: Jin Gu Kim.
Writing—original draft: Jin Gu Kim.
Writing—review & editing: Seung Ho Yang.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
References
1. Jane JA, Park TS, Pobereskin LH, Winn HR, Butler AB. The supraorbital approach: technical note. Neurosurgery. 1982; 11:537–542. PMID: 7145070.
2. Andaluz N, Van Loveren HR, Keller JT, Zuccarello M. Anatomic and clinical study of the orbitopterional approach to anterior communicating artery aneurysms. Neurosurgery. 2003; 52:1140–1148. discussion 1148-9. PMID: 12699559.
3. Fujitsu K, Kuwabara T. Orbitocraniobasal approach for anterior communicating artery aneurysms. Neurosurgery. 1986; 18:367–369. PMID: 3517674.
4. Smith RR, Al-Mefty O, Middleton TH. An orbitocranial approach to complex aneurysms of the anterior circulation. Neurosurgery. 1989; 24:385–391. PMID: 2927612.
5. Balasingam V, Noguchi A, McMenomey SO, Delashaw JB Jr. Modified osteoplastic orbitozygomatic craniotomy. Technical note. J Neurosurg. 2005; 102:940–944. PMID: 15926727.
6. Tanriover N, Ulm AJ, Rhoton AL Jr, Kawashima M, Yoshioka N, Lewis SB. One-piece versus two-piece orbitozygomatic craniotomy: quantitative and qualitative considerations. Neurosurgery. 2006; 58:ONS-229–ONS-237. discussion ONS-237.
7. Cheng CM, Chang CF, Ma HI, Chiang YH, McMenomey SO, Delashaw JB Jr. Modified orbitozygomatic craniotomy for large medial sphenoid wing meningiomas. J Clin Neurosci. 2009; 16:1157–1160. PMID: 19560361.
8. López-Elizalde R, Robledo-Moreno E, O Shea-Cuevas G, Matute-Villaseñor E, Campero Á, Godínez-Rubí M. Modified orbitozygomatic approach without orbital roof removal for middle fossa lesions. J Korean Neurosurg Soc. 2018; 61:407–414. PMID: 29631381.
9. Cherekaev VA, Gol'bin DA, Belov AI, Radchenkov NS, Lasunin NV, Vinokurov AG. Orbitozygomatic approaches to the skull base. Zh Vopr Neirokhir Im N N Burdenko. 2015; 79:95–101. PMID: 26529627.
10. Kim IS, Rha HK, Lee KJ, et al. Surgical approaches to the middle cranial base tumors. J Korean Neurosurg Soc. 2001; 30:1079–1085.
11. Schwartz MS, Anderson GJ, Horgan MA, Kellogg JX, McMenomey SO, Delashaw JB Jr. Quantification of increased exposure resulting from orbital rim and orbitozygomatic osteotomy via the frontotemporal transsylvian approach. J Neurosurg. 1999; 91:1020–1026. PMID: 10584849.
12. Taguchi Y, Tanaka K, Matsuzawa M, Sekino H. A surgical technique to avoid postoperative enophthalmos in the cranioorbital approach. Technical note. J Neurosurg. 1996; 85:514–517. PMID: 8751643.
13. Ota N, Tanikawa R, Miyazaki T, et al. Surgical microanatomy of the anterior clinoid process for paraclinoid aneurysm surgery and efficient modification of extradural anterior clinoidectomy. World Neurosurg. 2015; 83:635–643. PMID: 25527880.
14. Zabramski JM, Kiriş T, Sankhla SK, Cabiol J, Spetzler RF. Orbitozygomatic craniotomy. Technical note. J Neurosurg. 1998; 89:336–341. PMID: 9688133.
15. Kodera T, Arishima H, Yamada S, et al. Orbitozygomatic craniotomy with modified Zabramski's technique: a technical note and anatomic and clinical findings. World Neurosurg. 2017; 97:49–57. PMID: 27693820.
16. Mercier P, Brassier G, Fournier HD, Delion M, Papon X, Lasjaunias P. Morphological anatomy of the cranial nerves in their cisternal segment (III-XII). Neurochirurgie. 2009; 55:78–86. PMID: 19328500.
17. Son BC, Lee SW, Kim S, Hong JT, Sung JH, Yang SH. Transzygomatic approach with intraoperative neuromonitoring for resection of middle cranial fossa tumors. J Neurol Surg B Skull Base. 2012; 73:28–35. PMID: 23372992.
Fig. 1
One-piece frontotemporal craniotomy accompanied by orbitotomy following reflection of the temporalis muscle. A: Orbit is exposed after a modified orbitozygomatic craniotomy. B: Parasellar regions are approached by anterior clinoidectomy.
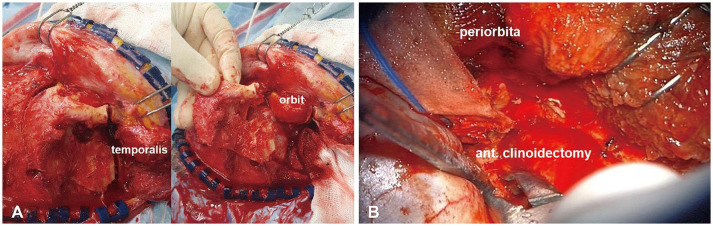
Fig. 2
Preoperative sagittal (A) and coronal (B) T1-enhanced images. Large pituitary adenoma (3.5×5.8×6.3 cm) noted in sellar, suprasellar, the third ventricle, and the left cavernous sinus with an upward displacement of the optic chiasm and an encasement of the left internal carotid artery.
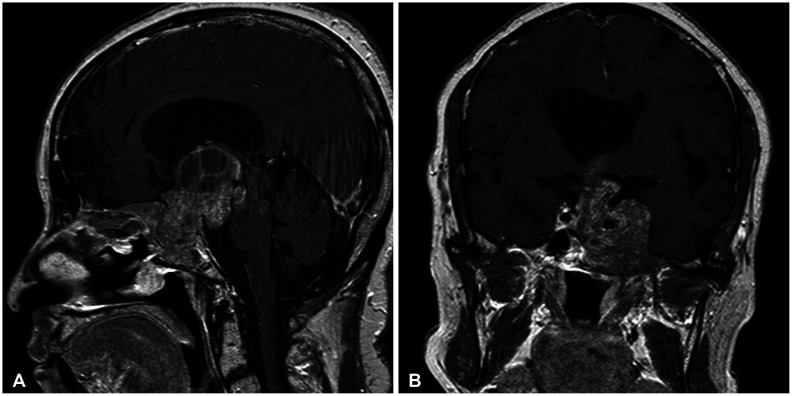
Fig. 3
Intraoperative findings. A: Left optic nerve (arrowhead) compressed by a tumor (asterisk). B: After the tumor’s removal, basilar artery is noted. ACA, anterior cerebral artery; MCA, middle cerebral artery.
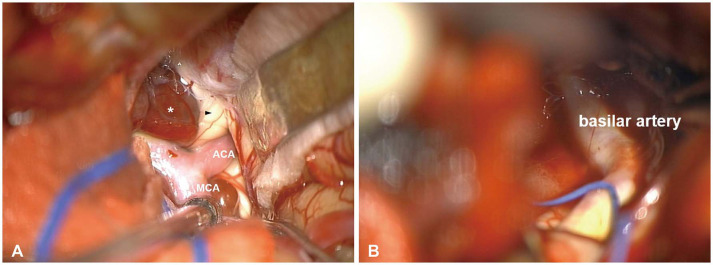
Fig. 4
Postoperative MR images. A: Axial T1-enhanced image showing removal of the lesion located in sellar, suprasellar, and the third ventricle. B: Coronal T1-enhanced image shows that hydrocephalus is resolved but remnant tumor is noted in the left cavernous sinus.

Fig. 5
Illustrated comparison of pterional approach (red) and modified orbitozygomatic approach (blue).
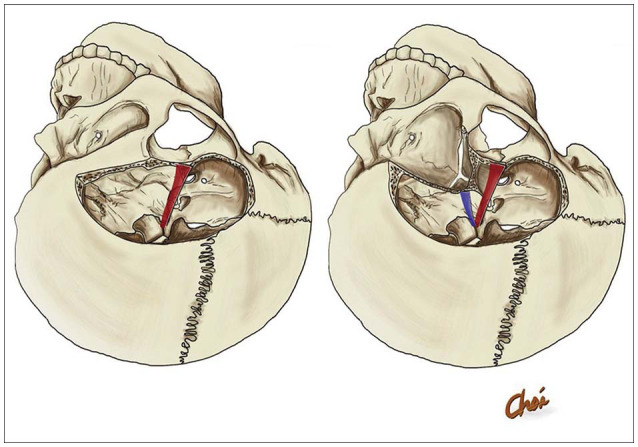
Table 1
Characteristics of patients underwent a modified orbitozygomatic approach




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download