Abstract
Intracranial neurenteric cyst at the anterior craniocervical junction is very rare, and its treatment and prognosis have not been established. We report a case of neurenteric cyst at the anterior craniocervical junction and review the relevant literature. A 16-year-old girl presented with a 2-month history of slowly progressive headache. MRI revealed a well-defined intradural extramedullary cyst in the anterior medulla and brain stem with C1 cord compression. We performed gross total resection of the cyst using a far-lateral transcondylar approach. Surgical resection is the treatment of choice for neurenteric cysts at anterior craniocervical junction, the far-lateral transcondylar approach might be the optimal surgical approach.
Neurenteric cyst of the central nervous system is a congenital lesion characterized by misplaced endodermal epithelial cells. It is a rare benign lesion of the central neural axis that primarily occurs in the lower cervical or upper thoracic spine and accounts for 1.3% of all spinal cord tumors [12]. To date, only 80 cases of intracranial neurenteric cysts have been reported in the literature, and these cysts were located at the midline of the posterior fossa, cerebellopontine angle, fourth ventricle and brain stem [3]. Since only a few cases of neurenteric cyst at the anterior craniocervical junction have been reported, its treatment and prognosis remain unclear [45]. We present a case of neurenteric cyst at the anterior craniocervical junction that was surgically treated using the far-lateral transcondylar approach.
A 16-year-old girl presented with slowly progressive headache. MRI showed a well-defined, 14×16×20 mm, intradural extramedullary cystic lesion in the premedullary cistern (Fig. 1). The lesion was homogeneously hyperintense on T1- and T2-weighted images. There was no restriction on diffusion-weighted imaging. Slightly elevated cerebral blood flow and cerebral blood volume were noted in the anterior part of the cystic mass on perfusion-weighted imaging. There was no gadolinium contrast enhancement on MRI.
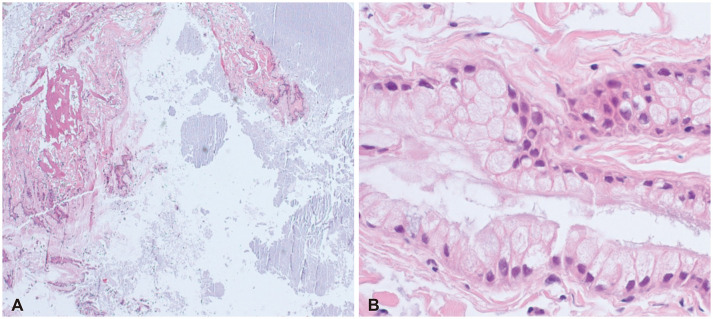
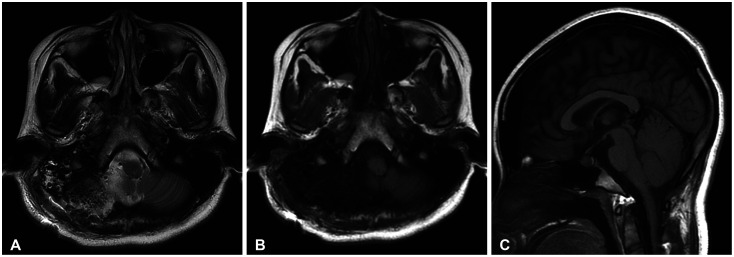
We decided to perform surgery to prevent symptom progression and avoid neurologic deficit. A far-lateral transcondylar approach was chosen to secure the surgical field and prevent cranial nerve injury (Fig. 2). We performed lateral suboccipital craniotomy with minimal condylectomy and secured the surgical field, which included the anterior aspect of the medulla and the premedullary cistern. The cyst was located following arachnoidal dissection of the cranial nerves and vertebral artery. The cyst was covered by a light gray capsule, which was loosely connected to the brain parenchyma. The cystic wall was punctured, and an amorphous gray-yellowish fluid was drained. The residual cyst capsule was completely detached from the adjacent neurovascular structures. Histopathological examination revealed non-ciliated, mucin-producing columnar and cuboid epithelial cells with isolated goblet cells, which are characteristic features of neurenteric cyst (Fig. 3). Complete surgical resection of the cyst was performed without any complications. MRI conducted postoperatively confirmed that the mass had been completely resected (Fig. 4). No adverse events occurred during 6-month follow-up period.
Neurenteric cyst is a rare congenital anomaly that usually associated with vertebral anomalies [6]. Embryologically, it is a central nervous system lesion of endodermal origin, and it has been known as enterogenous cyst, teratoid cyst, enteric cyst, respiratory cyst, endodermal cyst, gastrocytoma, intestinoma, and archenteric cyst [7]. Most intracranial neurenteric cysts are located at the craniocervical junction, fourth ventricle, or basal cistern, that is, anterior to the brain stem. Acute neurologic deficit is rare, and most symptoms are due to the mass effect of the slowly growing cysts [8].
The treatment of choice in symptomatic patients is complete surgical resection. Because of the risk of recurrence or malignant change due to incomplete resection, the goal of surgery is to resect both the cyst wall and its contents, completely [9]. The major determinant for complete neurenteric cyst resection is whether the arachnoid plane between the tumor and the surrounding tissue is preserved. Subtotal cyst resection is an alternative technique used in patients with severe adhesion to prevent damage to adjacent neurovascular structures [10]. However, revision surgery may be required if neurenteric cyst recurrence occurs from the remnant of cyst wall [1112]. The rate of recurrence following incomplete cyst resection varies, with overall recurrence rates is between 11.6% and 37% reported in different studies [1314]. To resect neurenteric cyst located in ventral craniocervical junction completely, many different surgical approaches have been discussed in literature. In many cases, the cyst was resected through suboccipital craniotomy, with or without cervical laminectomy, using a conventional posterior approach [1516]. Since the neurenteric cysts are located anterior to the medulla and cervical cord, a secure surgical field is necessary for the resection of the cyst using decompression through cyst aspiration. However, when the cyst wall is adhered to the anterior structure, it is difficult to view the cyst from its posterior side, there is a high risk of damage to the medulla and cervical cord due to intraoperative manipulation and retraction.
In some cases, an anterior approach such as a transoral approach is used for complete neurenteric cyst resection [1718]. Although the transoral approach provides a wide intraoperative view and access to the anterior craniocervical lesion, it is technically difficult and is often associated with fatal postoperative complications such as infection [18].
The far-lateral transcondylar approach is considered the most effective technique for managing anterior craniocervical lesions [19]. Satisfactory surgical outcomes and prognoses have been reported for cyst resection using the far-lateral transcondylar approach [2021]. This approach provides a direct intraoperative view of the lower clivus, anterior craniocervical junction, and neurenteric cysts at the anterior brain stem and cervical cord without retraction of the medulla and cervical cord. In the case series on the surgical resection of neurenteric cysts at the anterior craniocervical junction using a far-lateral transcondylar approach, Menezes et al. [22] reported that in all 5 patients, who had extramedullary neurenteric cysts located anterior to the foramen magnum, the lesion was completely resected using far-latral transcondylar approach. After complete resection, all symptoms and signs were improved, and there was no recurrence for 1 to 28 years. Adequate working space can be secured through condylar resection and vertebral artery exposure. Depending on the extent of occipital condylar resection, there may be increased instability, necessitating occipitocervical fusion. In general, it is known that removal of one-third of the occipital condyle does not cause instability [23].
Clinical and radiological follow-up is needed for at least 5 to 10 years after surgery [24]. Because of the risk of recurrence, patients with a residual mass or residual cyst wall may require longer follow-up.
Neurenteric cyst is a rare, benign central nervous system lesion. Although it usually occurs in the cervical or thoracic spine, intracranial neurenteric cysts should be considered during the differential diagnosis of intracranial cystic lesions. When symptoms developed and surgical resection is to be performed, based on our experience, the far-lateral transcondylar approach is the optimal technique for improving the prognosis through complete cyst resection as it provides a good intraoperative view of the cyst and adjacent neurovascular structures while minimizing brain retraction.
Ethics Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Board of CHA Bundang Medical Center (approval no. 2020-04-055). The study demonstrated minimal risk for included patients and received a waiver of informed consent from the Institutional Review Board.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
References
1. Sundaram C, Paul TR, Raju BV, et al. Cysts of the central nervous system: a clinicopathologic study of 145 cases. Neurol India. 2001; 49:237–242. PMID: 11593239.
2. Guilburd JN, Arieh YB, Peyser E. Spinal intradural enterogenous cyst: report of a case. Surg Neurol. 1980; 14:359–362. PMID: 7444743.
3. Al Qadhi S, Laiq S, Salhotra N, et al. Neurenteric cyst at craniovertebral junction: an uncommon presentation. Am J Med Case Rep. 2021; 9:407–410.
4. Prasad GL, Sharma BS, Mahapatra AK. Ventral foramen magnum neurenteric cysts: a case series and review of literature. Neurosurg Rev. 2016; 39:535–544. PMID: 26662045.
5. Haque M, Rahman A, Ahmed N, Alam S. Huge ventral cervicomedullary neurenteric cyst: a rare entity with good surgical outcome and appraisal. Asian J Neurosurg. 2020; 15:1016–1019. PMID: 33708680.
6. Wang L, Zhang J, Wu Z, et al. Diagnosis and management of adult intracranial neurenteric cysts. Neurosurgery. 2011; 68:44–52. PMID: 21150754.
7. Preece MT, Osborn AG, Chin SS, Smirniotopoulos JG. Intracranial neurenteric cysts: imaging and pathology spectrum. AJNR Am J Neuroradiol. 2006; 27:1211–1216. PMID: 16775266.
8. Anderson T, Kaufman T, Murtagh R. Intracranial neurenteric cyst: a case report and differential diagnosis of intracranial cystic lesions. Radiol Case Rep. 2020; 15:2649–2654. PMID: 33093931.
9. Perry A, Scheithauer BW, Zaias BW, Minassian HV. Aggressive enterogenous cyst with extensive craniospinal spread: case report. Neurosurgery. 1999; 44:401–404. PMID: 9932896.
10. Gavrjushin AV, Chelushkin DM. Intra-axial neurenteric cyst of medulla: case report and literature review. Cureus. 2021; 13:e15361. PMID: 34239793.
11. Nelson SM, Mathis DA, Hobbs JK, Timpone VM. Intracranial neurenteric cyst mimicking an ependymoma: imaging features, pathologic correlation and review of literature. Clin Imaging. 2017; 44:117–120. PMID: 28505503.
12. Chen CT, Lai HY, Jung SM, Lee CY, Wu CT, Lee ST. Neurenteric cyst or neuroendodermal cyst? Immunohistochemical study and pathogenesis. World Neurosurg. 2016; 96:85–90. PMID: 27586176.
13. Warf BC. Comparison of endoscopic third ventriculostomy alone and combined with choroid plexus cauterization in infants younger than 1 year of age: a prospective study in 550 African children. J Neurosurg. 2005; 103:475–481. PMID: 16383244.
14. Savage JJ, Casey JN, McNeill IT, Sherman JH. Neurenteric cysts of the spine. J Craniovertebr Junction Spine. 2010; 1:58–63. PMID: 20890417.
15. Breeze RE, Nichols P, Segal H, Apuzzo ML. Intradural epithelial cyst at the craniovertebral junction. Case report. J Neurosurg. 1990; 73:788–791. PMID: 2213172.
16. Ergun R, Akdemir G, Gezici AR, Kara C, Ergungor F. Craniocervical neurenteric cyst without associated abnormalities. Pediatr Neurosurg. 2000; 32:95–99. PMID: 10838509.
17. Koksel T, Revesz T, Crockard HA. Craniospinal neurenteric cyst. Br J Neurosurg. 1990; 4:425–428. PMID: 2261106.
18. Menezes AH, Ryken TC. Craniocervical intradural neurenteric cysts. Pediatr Neurosurg. 1995; 22:88–95. PMID: 7710978.
19. Mehdi W, Niaz A, Irfan M, Tasdique S, Majeed S. Far lateral transcondylar approach for anterior foramen magnum lesions. Pak J Neurol Surg. 2020; 24:149–155.
20. Liu JK, Couldwell WT. Far-lateral transcondylar approach: surgical technique and its application in neurenteric cysts of the cervicomedullary junction: report of two cases. Neurosurg Focus. 2005; 19:1–7.
21. Menezes AH, Traynelis VC. Spinal neurenteric cysts in the magnetic resonance imaging era. Neurosurgery. 2006; 58:97–105. PMID: 16385333.
22. Menezes AH, Dlouhy BJ. Neurenteric cysts at foramen magnum in children: presentation, imaging characteristics, and surgical management—case series and literature review. Childs Nerv Syst. 2020; 36:1379–1384. PMID: 32322975.
23. Mazur MD, Couldwell WT, Cutler A, et al. Occipitocervical instability after far-lateral transcondylar surgery: a biomechanical analysis. Neurosurgery. 2017; 80:140–145. PMID: 28362894.
24. Gauden AJ, Khurana VG, Tsui AE, Kaye AH. Intracranial neuroenteric cysts: a concise review including an illustrative patient. J Clin Neurosci. 2012; 19:352–359. PMID: 22260959.
Fig. 1
Preoperative MR images of the craniocervical junction. A: The T2-weighted axial image shows a homogeneously hyperintense cyst (arrowhead) anterior to the medulla. B and C: Pre-gadolinium T1-weighted axial and sagittal images show a homogeneously hyperintense cyst that compresses the brain stem at the anterior craniocervical junction. D: The post-gadolinium T1-weighted axial image shows no enhancement of the cystic lesion. E: Diffusion MR image shows a homogeneously hyperintense cyst without diffusion restriction. F: Perfusion MR images reveal partial uptake of the contrast medium in the anterior part of the cystic lesion.
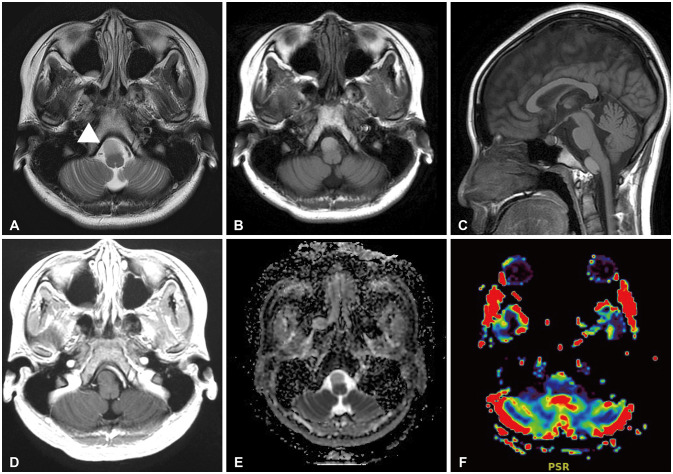
Fig. 2
Intraoperative photographs of neurenteric cyst resection using the far-lateral transcondylar approach. A: The right semispinalis captitis muscle was seen, and the dissection of the superior and inferior oblique muscles was performed. B: To secure the vertebral artery, the groove of the vertebral artery was located and lateral partial suboccipital craniotomy was performed. Condylectomy was performed to optimize the view of the anterior brain stem. C: A well-defined capsulated cyst that adheres to the lower cranial nerve and vertebral artery was seen. Posterior bulging of the medulla and cervical cord were seen. D: The lesion was punctured and filled with yellowish viscous fluid. E: The decompressed and lax cyst was completely resected after dissection of the adhesion, which was approximately 10 mm long. F: The premedullary cistern was subsequently secured. The medulla, cervical cord, low cranial nerve, C1 nerve root, and vertebral artery were intact.
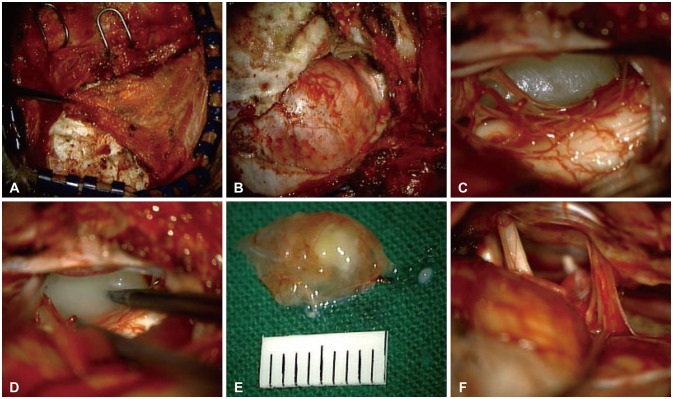
Fig. 3
Histopathologic findings. A: The low-magnification image shows mucin (hematoxylin and eosin stain, original magnification ×40). B: The high-magnification image shows non-ciliated, mucin-producing columnar epithelium lining the cyst wall and basal nuclei (hematoxylin and eosin stain, original magnification ×200).




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download