Abstract
A 69-year-old male presented with a week of worsening headache, mild dizziness and left side weakness, and the radiological work-up of his brain displayed an enhancing mass on the right frontal lobe. The tumor was totally resected. The patient was initially diagnosed with glioblastoma multiforme. His neurologic symptoms recovered after surgery. He underwent adjuvant radiotherapy with concurrent temozolomide. Approximately 7 months after surgery, the patient complained of epigastric pains. Abdominal CT scan showed multiple hepatic metastasis and multiple lymphadenopathy. Chest CT and Torso positron emission tomography-CT scans for additional metastasis study revealed multiple metastatic lesions in the right lung, left pleura, liver, lymph nodes, bones, and muscles. Percutaneous liver biopsy was performed, and associated pathology was consistent with sarcomatous component. After liver biopsy, brain tumor pathology was reviewed, which revealed typical gliomatous and sarcomatous components. The patient was therefore diagnosed with metastatic gliosarcoma. The patient was in a septic condition with aggravated pleural effusion. The patient died 9 months after the diagnosis of primary gliosarcoma.
Gliosarcoma (GS) is a rare type of brain tumor, which comprises both gliomatous and sarcomatous components. The tumor is considered a rare variant of glioblastoma multiforme (GBM) and encompasses approximately 2% of all GBMs [1]. GSs are classified as World Health Organization (WHO) grade IV tumors according to the 2016 WHO classification scheme. Primary gliosarcomas (PGSs) may manifest as extracranial metastasis, although rarely [2]. Compared with GBM, GS has a great propensity of manifesting as extracranial metastasis. Here, we describe an uncommon case of PGS with extracranial metastasis that was initially regarded as GBM.
A 69-year-old male presented with headache which worsened gradually over a week, mild dizziness, and left side weakness. His physical examination results revealed mental alertness and a grade 4/5 left hemiparesis. CT of his brain displayed an enhancing 3.7 cm sized mass on the right frontal lobe (Fig. 1A). Additional radiological work-up, namely T1-weighted and T2-weighted MRI scans of the brain, revealed that the lesion was iso-intense and hyperintense to the brain parenchyma, respectively, with peripheral enhancement (Fig. 1B, C). Chest and abdomen CT scans as an initial metastatic work-up showed no evidence of metastatic lesions. The tumor was totally resected (Fig. 1D). The patient's initial histopathologic diagnosis was WHO grade IV, isocitrate dehydrogenase (IDH)-wild type (Fig. 2), and his neurologic symptoms recovered after surgery. He received adjuvant radiotherapy (60 Gy in 30 fractions) with concurrent temozolomide (75 mg/m2 for 42 days), followed by 2 cycles of adjuvant temozolomide (150 to 200 mg/m2 for 5 days during each 28-day cycle).
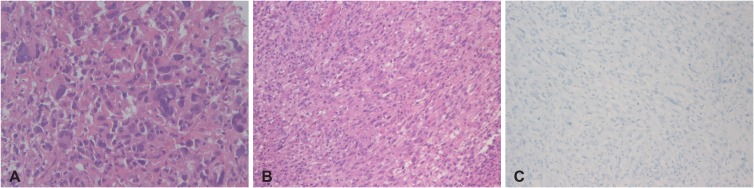
Approximately 7 months after surgery, the patient complained of epigastric pains. Abdomen CT scans showed multiple hepatic metastasis and multiple lymphadenopathy (Fig. 3A). Additional metastatic work-up including, chest CT and Torso positron emission tomography-CT scans displayed extensive metastatic lesions in the right lung, left pleura, liver, lymph nodes, bones and muscles (Fig. 3B, C). Percutaneous liver biopsy was performed (Fig. 4A). The pathology was consistent with sarcomatous component with immunopositivity for vimentin. After liver biopsy, pathology of the brain tumor was reviewed, and that tumor was found to not only contain a typical gliomatous component but also a sarcomatous component (Fig. 4B, C). The patient was diagnosed with systemic metastasis of GS. He was in a septic condition, with aggravated pleural effusion. The patient died 9 months after the diagnosis of PGS.
PGSs have various distinct features. They are located in the supratentorial space, with a predilection for the peripheral region of the temporal lobe. PGSs are more grossly distinct at surgery than GBMs, and they are often firm and well-circumscribed because of the presence of a sarcomatous component [3].
PGSs are often treated in the same manner as GBMs, because the former is a variant of the latter. Treatment modalities for GSs include tumor resection, adjuvant radiotherapy, and chemotherapy. PGSs have well-demarcated margins owdiing to the presence of a sarcomatous component, but it shows a weaker response to adjuvant treatment involving chemotherapy and radiotherapy during the postoperative period [4].
Although a rare occurrence, PGSs may show extracranial metastasis. The reported rate of extracranial metastasis for malignant gliomas is approximately 0.5% of cases [5]. There are several assumptions why extracranial metastasis of high grade glioma rarely occurs. The first assumption is the highly aggressive behavior of high grade gliomas. The mean survival time of high grade gliomas ranges from 6 to 14.8 months after diagnosis [6]. Since metastasis is rare, systemic staging imaging studies are not standard practice. Thus, extracranial metastasis may occur more frequently, but it is not diagnosed prior to fatal brain herniation.
Another explanation is the intrinsic biological obstacles that prevent tumor cells from infiltrating and surviving beyond the neural environment include the absence of a lymphatic system within the brain and spinal cord, and dense dura around intracranial veins [57].
Tumors metastasize by invading through connective tissue in other organs. There is rare collagen and fibronectin within central nervous system, the primary malignant brain tumors lack a component essential for extracranial metastasis. However, vascular endothelium derived fibronectin was more prominent in endothelial cells of high grade gliomas than low grade gliomas. For this reason, high grade gliomas have the ability to invade through connective tissue, basement membranes and blood vessels [789].
Compared to GBMs, PGSs have a great propensity for extracranial metastasis. The reported rate of extracranial metastasis for PGS is approximately 11% [10]. Smith et al. [11] reported a metastatic case series of 7 cases of GSs, and they observed that in 2 cases, the metastatic foci were composed only of a sarcomatous component. Other case reports showed similar finding of sarcomatous components alone in metastases [61213]. These observations indicate that the metastatic potential of GSs can be attributed to the sarcomatous component and reflects the great propensity of sarcomatous neoplasm to disseminate hematogenously. In our case, liver biopsy findings revealed the presence of a sarcomatous component alone, consistent with the other cases, wherein the metastatic foci had been composed solely of the sarcomatous component.
GSs that develop de novo are PGSs whereas those that are diagnosed subsequent to a diagnosis of GBMs are considered secondary GSs. Treatment for GBM, especially irradiation, may lead to sarcomatous metaplasia of glial cells. GBMs obtain the extracellular matrix proteins for vascular invasion and hematogenous dissemination to extracranial metastasis by sarcomatous metaplasia.
Although the extracranial metastatic mechanism currently remains unclear, iatrogenic spread consequent to surgery may be the main reason for extracranial metastasis [514]. The tumor cells can access the blood stream through defects in the meningeal and parenchymal blood vessels that are created. The patient described in this article also had a history of craniotomy.
The most common site of extracranial metastasis is intraspinal, followed by the vertebrae, lungs, liver, and lymph nodes. Moreover, metastasis has been reported in the spleen, scalp, skin, paranasal sinuses, eyes, parotid gland, small intestine, pancreas, kidneys, bone, pleura, and peritoneum [5].
The prognosis of GSs is similar to that of GBMs, with a mean survival time ranging from 6 to 14.8 months after diagnosis. A recent meta-analysis of outcomes of GBMs/GSs patients with extracranial metastasis revealed that the mean survival time was only 6.0±0.8 months after diagnosis [6].
PGSs may show extracranial metastasis, although rarely. Compared with GBM, GSs has a great propensity for extracranial metastasis. As a standard practice in the management of patients with GBMs, screening for extra-cranial metastasis may be warranted at the time of diagnosis and surveillance for all cases of GSs.
References
1. Ben Nsir A, Thai QA, Kassar AZ, Ben Said I, Jemel H. Primary cerebellar gliosarcoma with extracranial metastases: an orphan differential diagnosis. World Neurosurg. 2015; 84:2076.e13–2076.e17.
2. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016; 131:803–820. PMID: 27157931.
3. Han SJ, Yang I, Tihan T, Prados MD, Parsa AT. Primary gliosarcoma: key clinical and pathologic distinctions from glioblastoma with implications as a unique oncologic entity. J Neurooncol. 2010; 96:313–320. PMID: 19618114.
4. Tabibkhooei A, Fattahi A, Ebrahimnia F. Gliosarcoma with long progression free survival: a case report and literature review. Surg Neurol Int. 2018; 9:227. PMID: 30533274.
5. Sun Q, Xu R, Xu H, Wang G, Shen X, Jiang H. Extracranial metastases of high-grade glioma: the clinical characteristics and mechanism. World J Surg Oncol. 2017; 15:181. PMID: 28985756.
6. Weaver D, Vandenberg S, Park TS, Jane JA. Selective peripancreatic sarcoma metastases from primary gliosarcoma. case report. J Neurosurg. 1984; 61:599–601. PMID: 6747700.
7. Ray A, Manjila S, Hdeib AM, et al. Extracranial metastasis of gliobastoma: three illustrative cases and current review of the molecular pathology and management strategies. Mol Clin Oncol. 2015; 3:479–486. PMID: 26137254.
8. Mentrikoski M, Johnson MD, Korones DN, Scott GA. Glioblastoma multiforme in skin: a report of 2 cases and review of the literature. Am J Dermatopathol. 2008; 30:381–384. PMID: 18645311.
9. Lin ZX, Yang LJ, Huang Q, Fu J. Activated vascular endothelia regulate invasion of glioma cells through expression of fibronectin. Chin Med J (Engl). 2010; 123:1754–1761. PMID: 20819642.
10. Beaumont TL, Kupsky WJ, Barger GR, Sloan AE. Gliosarcoma with multiple extracranial metastases: case report and review of the literature. J Neurooncol. 2007; 83:39–46. PMID: 17171442.
11. Smith DR, Hardman JM, Earle KM. Contiguous glioblastoma multiforme and fibrosarcoma with extracranial metastasis. Cancer. 1969; 24:270–276. PMID: 4307749.
12. Gjerdrum LM, Bojsen-Møller M. 61 year old male with brain tumor and oral, lung, and palpebral masses. Brain Pathol. 1999; 9:421–422. PMID: 10219754.
13. Ojeda VJ, Sterrett GF. Cerebral gliosarcoma, pulmonary adenoid-cystic carcinoma, and pulmonary metastatic gliosarcoma: report of an untreated case. Pathology. 1984; 16:217–221. PMID: 6087260.
14. Wu W, Zhong D, Zhao Z, Wang W, Li J, Zhang W. Postoperative extracranial metastasis from glioblastoma: a case report and review of the literature. World J Surg Oncol. 2017; 15:231. PMID: 29284526.
Fig. 1
Pre- and postoperative brain imaging. A: Contrast-enhanced brain CT scan showing a rim-enhanced lesion (diameter, 3.7 cm). B: T2-weighted MRI scan showing a high-signal intensity edematous mass-like lesion. C: Gadolinium-enhanced T1-weighted MRI scan showing a well enhanced mass. D: The follow-up gadolinium-enhanced T1-weighted MRI scan taken after total tumor resection shows no evidence of enhanced lesion, which is considered as a remnant tumor.
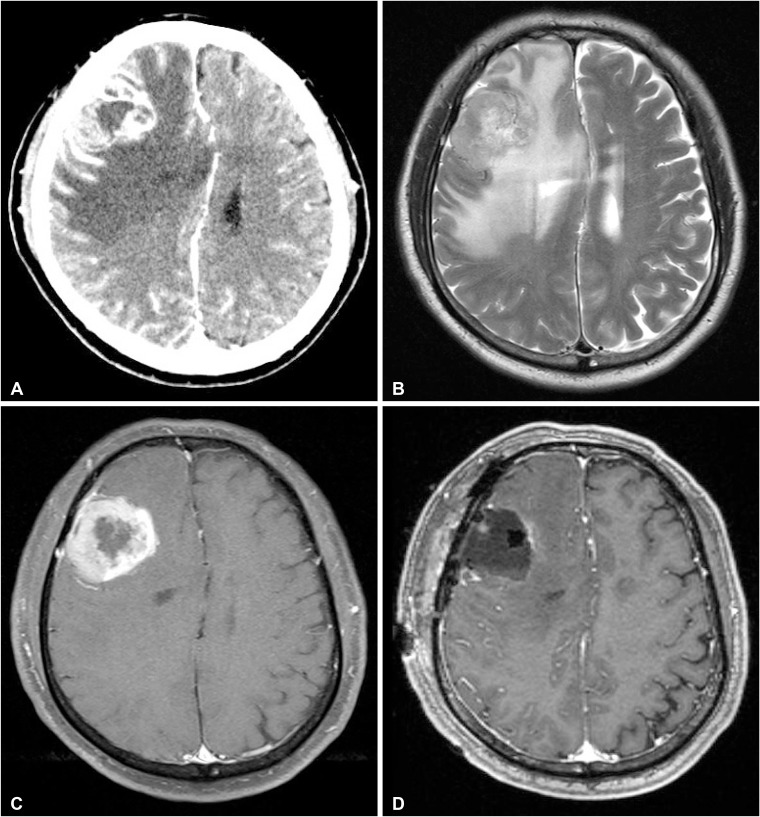
Fig. 2
Histopatological analysis of the brain tumor revealing high cellularity as well as cellular and nuclear anaplasia (hematoxylin and eosin stain, 100× magnification) (A). Image of glial fibrillary acidic protein staining showing the gliomatous component of the tumor (100× magnification) (B).
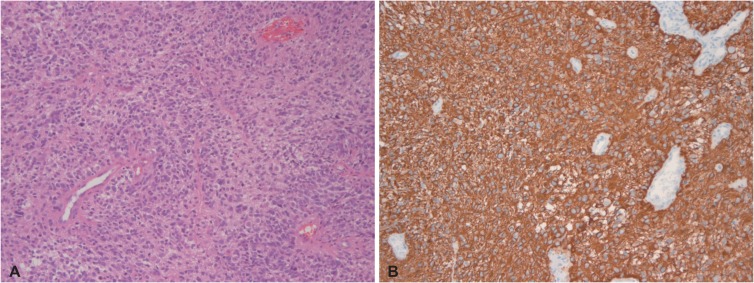
Fig. 3
Extracranial metastases of the gliosarcoma. A: Abdomen CT scan showing multiple hepatic metastasis and multiple lymphadenopathy. B: Chest CT scan showing pleural effusion of the right lung. C: Torso positron emission tomography-CT scan shows multiple metastatic lesions in the right lung, left pleura, liver, lymph nodes, bones, and muscles.

Fig. 4
Histopatological analysis of the liver revealing neoplastic cells with marked pleomorphic nucleus (H&E stain, 200× magnification) (A). Pathologic findings of the brain; sarcomatous component of spindle cells (H&E stain, 100× magnification) (B). Pathologic findings of brain; image of glial fibrillary acidic protein staining showing the non-gliomatous component of the tumor (100× magnification) (C). H&E, hematoxylin and eosin.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download