Abstract
Notes
Ethics Statement: The Institutional Review Board of National Health Insurance Service Ilsan Hospital exempted the requirement for written informed consent in this case of verbal allowance to publish the retrospective case report with a minimal risk for the patient (NHIMC 2022-01-023).
Author Contributions:
Conceptualization: Kookhee Yang.
Data curation: Boeun Lee.
Formal analysis: Boeun Lee.
Funding acquisition: Kookhee Yang.
Investigation: Dong Jun Jeong.
Methodology: Boeun Lee.
Project administration: Boeun Lee.
Resources: Kookhee Yang.
Software: Boeun Lee.
Supervision: Kookhee Yang.
Validation: Boeun Lee.
Visualization: Dong Jun Jeong.
Writing—original draft: Dong Jun Jeong.
Writing—review & editing: Kookhee Yang.
Availability of Data and Material
References
Fig. 1
Initial MR image. A: T2-weighted axial MR image showing a parietal osteolytic lesion, confirming the presence of a herniated brain cortex within the diploe. B: Magnified the white square of T2-weighted axial image. C: T2-weighted coronal MR image. D: Magnified the white square of T2-weighted coronal image. E: Gadolinium (Gd)-enhanced T1-weighted axial MR image. F: Magnified the white square of Gd-enhanced T1-weighted axial image reveal no enhancement of lesion.

Fig. 2
Skull X-ray and CT findings. A: Initial skull X-ray showing an osteolytic lesion (white arrow heads) in the right parietal bone. B: Initial CT scan showing intradiploic herniation of brain parenchyma. C: Initial CT scan (bone window) reveal skull osteolytic lesion confined to inner table. D: Two-year follow up CT scan shows no change of the lesion.

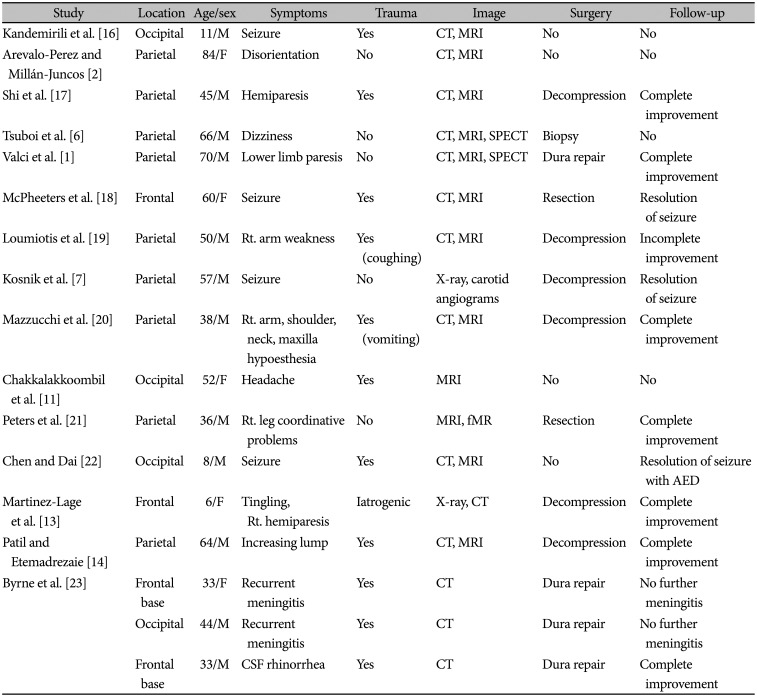
Table 1
Review of intradiploic encephalocele cases
| Study | Location | Age/sex | Symptoms | Trauma | Image | Surgery | Follow-up |
|---|---|---|---|---|---|---|---|
| Kandemirili et al. [16] | Occipital | 11/M | Seizure | Yes | CT, MRI | No | No |
| Arevalo-Perez and Millán-Juncos [2] | Parietal | 84/F | Disorientation | No | CT, MRI | No | No |
| Shi et al. [17] | Parietal | 45/M | Hemiparesis | Yes | CT, MRI | Decompression | Complete improvement |
| Tsuboi et al. [6] | Parietal | 66/M | Dizziness | No | CT, MRI, SPECT | Biopsy | No |
| Valci et al. [1] | Parietal | 70/M | Lower limb paresis | No | CT, MRI, SPECT | Dura repair | Complete improvement |
| McPheeters et al. [18] | Frontal | 60/F | Seizure | Yes | CT, MRI | Resection | Resolution of seizure |
| Loumiotis et al. [19] | Parietal | 50/M | Rt. arm weakness | Yes (coughing) | CT, MRI | Decompression | Incomplete improvement |
| Kosnik et al. [7] | Parietal | 57/M | Seizure | No | X-ray, carotid angiograms | Decompression | Resolution of seizure |
| Mazzucchi et al. [20] | Parietal | 38/M | Rt. arm, shoulder, neck, maxilla hypoesthesia | Yes (vomiting) | CT, MRI | Decompression | Complete improvement |
| Chakkalakkoombil et al. [11] | Occipital | 52/F | Headache | Yes | MRI | No | No |
| Peters et al. [21] | Parietal | 36/M | Rt. leg coordinative problems | No | MRI, fMR | Resection | Complete improvement |
| Chen and Dai [22] | Occipital | 8/M | Seizure | Yes | CT, MRI | No | Resolution of seizure with AED |
| Martinez-Lage et al. [13] | Frontal | 6/F | Tingling, Rt. Hemiparesis | Iatrogenic | X-ray, CT | Decompression | Complete improvement |
| Patil and Etemadrezaie [14] | Parietal | 64/M | Increasing lump | Yes | CT, MRI | Decompression | Complete improvement |
| Byrne et al. [23] | Frontal base | 33/F | Recurrent meningitis | Yes | CT | Dura repair | No further meningitis |
| Occipital | 44/M | Recurrent meningitis | Yes | CT | Dura repair | No further meningitis | |
| Frontal base | 33/M | CSF rhinorrhea | Yes | CT | Dura repair | Complete improvement |




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download