Abstract
Intracranial plasmacytoma is a rare neoplasm and a subtype of malignant plasma cell tumor. Most patients with plasma cell tumors are diagnosed with multiple myeloma, but 5%–10% of patients are not. This report includes descriptions of radiologic and clinical findings in a patient with intracranial plasmacytoma. Intracranial extra-axial plasmacytomas can be easily misdiagnosed as meningioma in radiologic and clinical findings. A 69-year-old woman presented with exophthalmos and diplopia, and MRI indicated meningioma. Thus, she underwent gross total resection, and her pathologic diagnosis was plasmacytoma. Exophthalmos and diplopia were fully recovered. She was finally diagnosed with multiple myeloma based on systemic evaluation and treated with targeted chemotherapy. MRI conducted at 3 months after surgery showed no local recurrence or remnant tumor. Although intracranial plasmacytomas are difficult to distinguish from meningiomas in preoperative evaluation, gross total resection is recommended for the same purposes as meningiomas. If the pathologic diagnosis is a plasmacytoma, it is essential to have a systemic evaluation for multiple myeloma.
Intracranial plasmacytoma is a rare neoplasm. It refers to the presence of a solitary plasmacytoma in skull, meninges or brain. Solitary plasmacytoma is a subtype of malignant plasma cell tumor [123]. Most patients with plasma cell tumors are diagnosed with multiple myeloma. However, in a few patients with plasma cell tumor, a single bone lesion (solitary bone plasmacytoma, SBP) or a soft tissue lesion (solitary extramedullary plasmacytoma, SEP) could be developed. Intracranial plasmacytoma is a disease that can belong to either SBP or SEP [145]. We report a case of an intracranial plasmacytoma in a 64-year-old woman, who was finally diagnosed with multiple myeloma.
A 69-year-old woman presented with exophthalmos of right eye with reduced visual acuity and diplopia for three months. There were no systemic symptoms. Laboratory findings were normal. Brain CT revealed a 5.1×4.4×4.7-cm hyperdens lobulated mass with lysis of the lateral wall of the right orbit, zygomatic process of right frontal bone, squamous part of the right temporal bone and the presence of an extracranial component (Fig. 1). Orbit MRI revealed a 5.1×4.4×4.7-cm contrast-enhancing and diffusion restricted, lobulated mass infiltrating the zygomatic process of the right frontal bone and extending up to right intraconal space, intracranial space, and right infratemporal fossa (Fig. 2). External carotid angiography with embolization showed the presence of a tumor-like vascular brush at the right periorbital area supplied by branches from the middle meningeal, internal maxillary, and superficial temporal arteries (Fig. 3A and B). Embolization was performed after selective catheter insertion into the right external carotid branches (Fig. 3C and D). A preoperative diagnosis was periorbital meningioma or skull-base malignancy.
She underwent surgery via a right frontotemporal craniotomy. Intraoperatively, soft and highly vascular mass was detected. It was glued to the bones, muscles and dura mater. Gross total resection of tumor was performed, including the infiltrating dura mater. Dural defect was repaired with pericranium. The result of intraoperative frozen biopsy was mesenchymal tumor. There were no postoperative complications. Exophthalmos and diplopia were recovered.
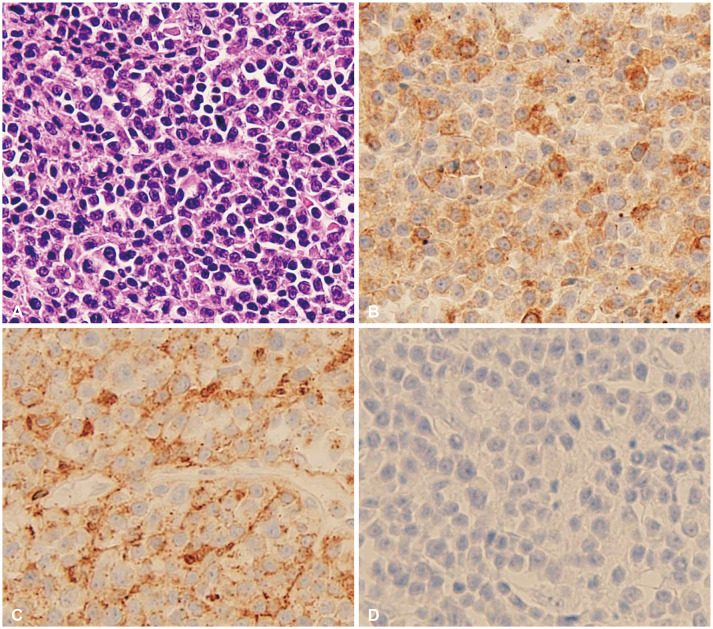
Microscopic examination showed high cellularity of well-differentiated plasma cells. Rare immature plasmacytic cells were founded without necrotic areas (Fig. 4A). Immunohistochemistry revealed that tumor cells were CD138 and CD79a-positive plasmacytoma (Fig. 4B and C). She was then referred to the department of oncology for diagnosis of multiple myeloma and treatment.
There were no osteolytic lesions in plane X-ray scans. Whole body MRI revealed a macro-nodular type multiple myeloma with multiple macro-nodular lesions at sternum, ribs, both femoral shafts, pelvic bones, proximal humerus, and vertebrae. Serum electrophoresis showed a monoclonal peak of IgA-kappa. Bone marrow biopsy confirmed that the number of plasma cells increased (21.3%). Immunohistochemistry of bone marrow biopsy showed a CD138-positive result. She was finally diagnosed with IgA-kappa multiple myeloma. Targeted chemotherapy with Velcade + Revlimid + dexamethasone (VRd) regimen was started. There was no local recurrence or remnant tumor as a result of follow-up MRI at 3 months after surgery. Pachymeningeal enhancement considered as a postoperative change was found (Fig. 5).
Multiple myeloma is a cancer of plasma cells. It is characterized by proliferation and improper function of plasma cells with the production of immunoglobulin. A solitary plasmacytoma is characterized by localized proliferation of plasma cells without proof of systemic plasma cell proliferation. A solitary plasmacytomas are uncommon, accounting for 5%–10% of all plasma cell tumors [123]. Therefore, if a solitary plasmacytoma is diagnosed in any part of the body, it is essential to have a systemic evaluation for multiple myeloma [156789]. Moreover, patients diagnosed with a solitary plasmacytoma are required to have follow-up management because it may progress to multiple myeloma [910]. Factors that influence the risk and frequency of progression to multiple myeloma are controversial [11].
MRI of this patient revealed a single lobulated mass infiltrating the sphenoid bone and frontotemporal bone, which was enhanced homogenously. It had well defined border with characteristics of an extra-axial tumor. Plasmacytomas can be easily misdiagnosed as a meningioma in radiological and clinical findings [4]. It has similar radiologic features to meningiomas, such as extra-axial mass with attachment to the dura and high density on CT with homogenous enhancing lesion and vascular marking on MRI. Therefore, radiological findings of an intracranial plasmacytoma are not specific [34]. In imaging studies, plasmacytomas are not exactly differentiated from meningioma, lymphoma, metastasis, sarcoma, or infectious meningitis. It may be presented on angiography that a number of pathological vessels and a tumor brush. However, angiography is not a reliable diagnostic method for differential diagnosis, as 50%–70% of meningiomas may present angiographic features similar to the above [1234].
During operation, the mass was found to be in epidural and intradural space with infiltration to dura mater. It was not accurately identified whether it was an SEP or an SBP, but considering the wide bony erosion without sclerotic changes, it was suspected that an SBP had infiltrated the dura mater. The mechanism of plasmacytomas spreading to the dura mater is still unknown. A hypothesis of dural invasion of plasmacytomas is that bone lesions spread contiguously through the veins of the arachnoid [1112]. This case could support this hypothesis by findings of extensive bone erosion without sclerotic changes.
The first treatment of an intracranial plasmacytoma is gross total resection or subtotal resection exact diagnosis with pathology, reduction of mass effects and tumor induced edema, and cytoreduction of tumor as a malignant brain tumor. If the patient diagnosed with a solitary plasmacytoma, not a multiple myeloma, some authors recommend postoperative radiation therapy. Local control rates exceed 80% with radiation alone and doses over 40 Gy can provide an initial response rate of over 90% [12369]. If the patient diagnosed with multiple myeloma, systemic chemotherapy is recommended [24611]. Since this patient was diagnosed with IgA-kappa multiple myeloma, treated with targeted chemotherapy. Although the gold standard treatment of an intracranial plasmacytoma is unknown, we suggest the gross total resection of tumor, and systemic evaluation to diagnose multiple myeloma. Despite some authors reported recurrence after complete resection, a patient can expect long-term control of diseases with gross total resection of tumor.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
References
1. Soutar R, Lucraft H, Jackson G, Reece A, Bird J, Low E, et al. Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Clin Oncol (R Coll Radiol). 2004; 16:405–413. PMID: 15487132.

2. Dimopoulos MA, Moulopoulos A, Delasalle K, Alexanian R. Solitary plasmacytoma of bone and asymptomatic multiple myeloma. Hematol Oncol Clin North Am. 1992; 6:359–369. PMID: 1582978.

3. Kilciksiz S, Karakoyun-Celik O, Agaoglu FY, Haydaroglu A. A review for solitary plasmacytoma of bone and extramedullary plasmacytoma. ScientificWorldJournal. 2012; 2012:895765. PMID: 22654647.

4. Rahmah N, Brotoarianto H, Andor E, Kusnarto G, Muttaqin Z, Hongo K. Dural plasmacytoma mimicking meningioma in a young patient with multiple myeloma. Biomed Imaging Interv J. 2009; 5:e5. PMID: 21611030.

5. Seetahal-Maraj P, Knight P, Ramnarine N. Proptosis secondary to a solitary plasmacytoma of the sphenoid bone: a case report on a rare skull base tumour. Egypt J Neurosurg. 2022; 37:4.

6. Sahin F, Saydam G, Ertan Y, Calli C, Dönmez A, Tombuloglu M. Dural plasmacytoma mimicking meningioma in a patient with multiple myeloma. J Clin Neurosci. 2006; 13:259–261. PMID: 16459088.

7. Hasturk AE, Basmaci M, Erten F, Cesur N, Yilmaz ER, Kertmen H. Solitary dural plasmacytoma mimicking meningioma and invading calvarium. J Craniofac Surg. 2013; 24:e175–e177. PMID: 23524828.

8. Singh AD, Chacko AG, Chacko G, Rajshekhar V. Plasma cell tumors of the skull. Surg Neurol. 2005; 64:434–438. discussion 438-9. PMID: 16253694.

9. Bindal AK, Bindal RK, van Loveren H, Sawaya R. Management of intracranial plasmacytoma. J Neurosurg. 1995; 83:218–221. PMID: 7616264.

10. Dimopoulos MA, Kiamouris C, Moulopoulos LA. Solitary plasmacytoma of bone and extramedullary plasmacytoma. Hematol Oncol Clin North Am. 1999; 13:1249–1257. PMID: 10626148.

11. Haegelen C, Riffaud L, Bernard M, Carsin-Nicol B, Morandi X. Dural plasmacytoma revealing multiple myeloma. Case report. J Neurosurg. 2006; 104:608–610. PMID: 16619666.
12. Azarpira N, Noshadi P, Pakbaz S, Torabineghad S, Rakei M, Safai A. Dural plasmacytoma mimicking meningioma. Turk Neurosurg. 2014; 24:403–405. PMID: 24848182.

Fig. 1
Preoperative CT scanning. Axial (A) and coronal (B) views of brain CT revealed a mass lesion which has destroyed the lateral wall of the right orbit, zygomatic process of right frontal bone, and squamous part of the right temporal bone and extend to temporal muscle.
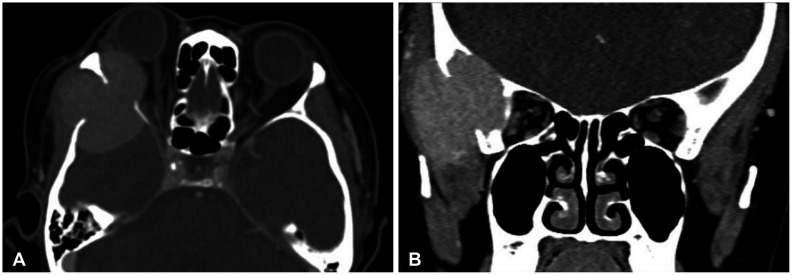
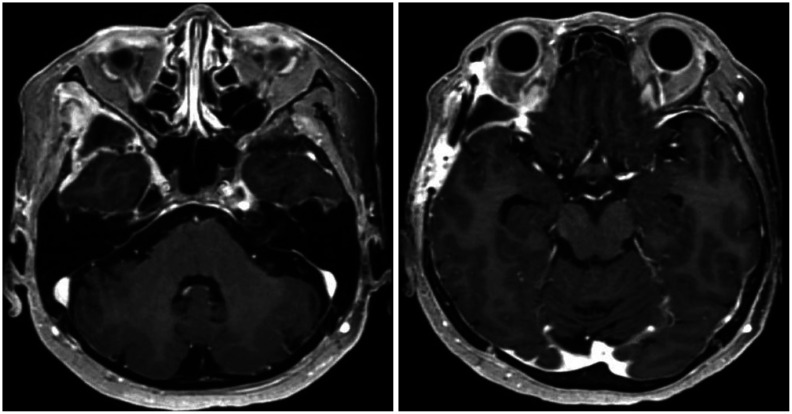
Fig. 2
Preoperative MRI. A: T2-weighted MR coronal image shows a lobulated extra-axial mass extend to exocranial space. B: Apparent diffusion coefficient map MR axial image shows low signal intensity, which indicate more aggressive tumor behavior. C and D: T1-weighted enhanced MR axial image demonstrates a homogenous hyperintense mass and thickened dura mate, which meningioma-like radiological appearance.
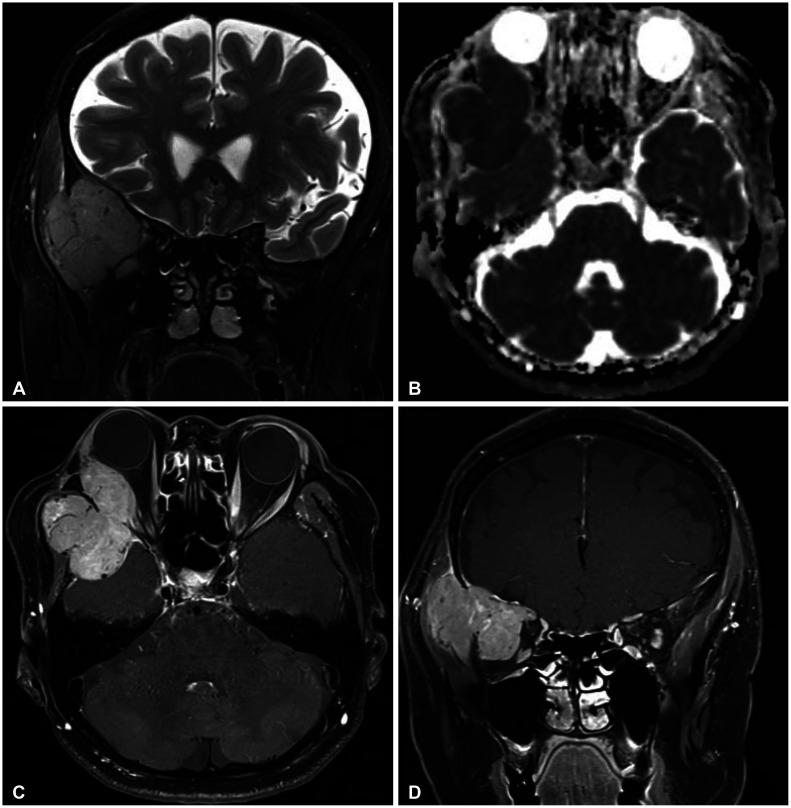
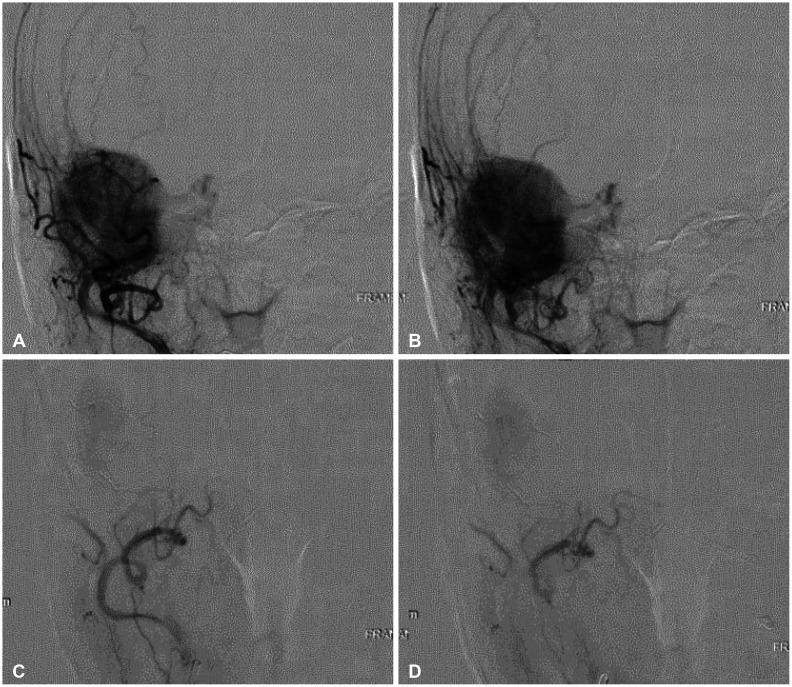
Fig. 3
Digital subtraction angiography. A and B: Pre-embolization angiography shows tumor-like vascular brush. C and D: Post-embolization angiography shows decreased blood flow.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download