Abstract
Notes
Ethics Statement: The Institional Review Board (IRB) exempted informed consent due to only descriptive nature of case report and no risk for harm to the patients, and this report was conucted according to the guidelines of the Declaration of Helsinki for biomedical research.
Author Contributions:
Conceptualization: Yong-Jun Lee, Shin Jung.
Data curation: Yong-Jun Lee, Shin Jung, Yeong Jin Kim.
Formal analysis: Yong-Jun Lee, Shin Jung.
Investigation: Yong-Jun Lee, Shin Jung, Bo-Seob Kim.
Methodology: Yong-Jun Lee, Shin Jung, Yeong Jin Kim.
Supervision: Shin Jung, Kyung-Hwa Lee.
Writing—original draft: Yong-Jun Lee.
Writing—review & editing: Shin Jung, Yeong Jin Kim, Kyung-Hwa Lee.
Availability of Data and Material
References
Fig. 1
Preoperative brain imaging. A: Initial brain CT revealing a hyperdense mass in the right posterior cranial fossa (right cerebellopontine angle and cerebellomedullary cistern). B and C: Iso-/hypointense signal mass in T1-weighted and iso-/hyperintense signal mass in T2-weighted images. D-F: Brain MRI with gadolinium enhancement revealing a homogeneously enhancing mass and mass effect on the 4th ventricle without definitive hydrocephalus.
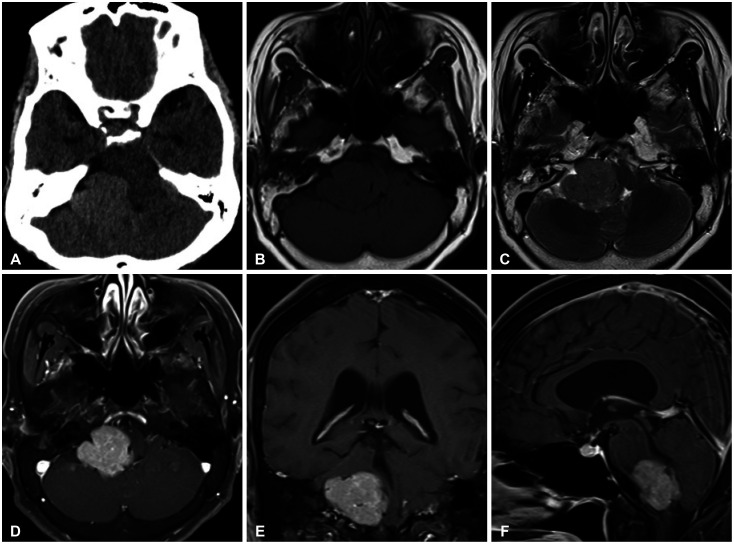
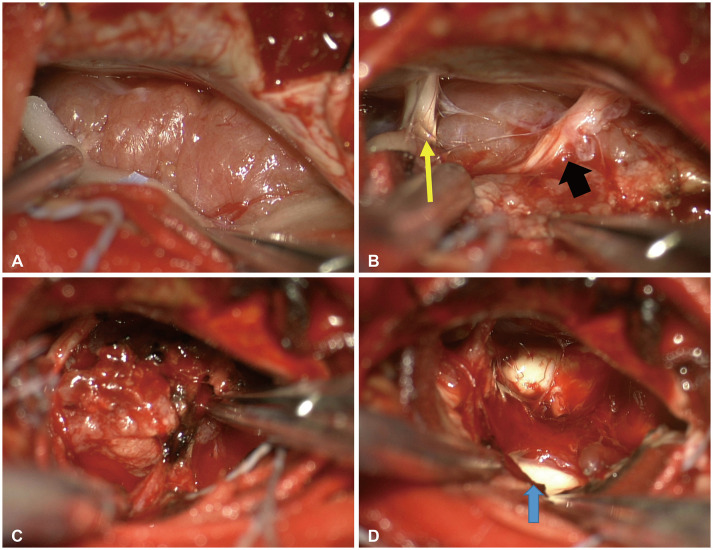
Fig. 2
Intraoperative findings. A: Mass of a large lower cerebellopontine angle region without dural attachment. B: 7th & 8th cranial nerves (yellow arrow) located in the cranial part and lower cranial nerves (9th & 10th) identified above the mass (black arrow). C: Mass originating from the choroid plexus of the foramen of Luschka. D: 4th ventricle lateral part (blue arrow) after mass removal and coagulation of the origin site.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download