1. Bleeker FE, Molenaar RJ, Leenstra S. Recent advances in the molecular understanding of glioblastoma. J Neurooncol. 2012; 108:11–27. PMID:
22270850.

2. Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009; 10:459–466. PMID:
19269895.

3. Krex D, Klink B, Hartmann C, von Deimling A, Pietsch T, Simon M, et al. Long-term survival with glioblastoma multiforme. Brain. 2007; 130(Pt 10):2596–2606. PMID:
17785346.

4. Burzynski S, Burzynski G. Long-term progression-free survival of recurrent glioblastoma multiforme treated with a combination of targeted agents: a case report. Neuro Oncol. 2014; 16(Suppl 5):v11.
5. Yong RL, Lonser RR. Surgery for glioblastoma multiforme: striking a balance. World Neurosurg. 2011; 76:528–530. PMID:
22251498.

6. Bergmann N, Delbridge C, Gempt J, Feuchtinger A, Walch A, Schirmer L, et al. The intratumoral heterogeneity reflects the intertumoral subtypes of glioblastoma multiforme: a regional immunohistochemistry analysis. Front Oncol. 2020; 10:494. PMID:
32391260.

7. Denicolaï E, Tabouret E, Colin C, Metellus P, Nanni I, Boucard C, et al. Molecular heterogeneity of glioblastomas: does location matter? Oncotarget. 2016; 7:902–913. PMID:
26637806.

8. Becker AP, Sells BE, Haque SJ, Chakravarti A. Tumor heterogeneity in glioblastomas: from light microscopy to molecular pathology. Cancers (Basel). 2021; 13:761. PMID:
33673104.

9. Bastiancich C, Da Silva A, Estève MA. Photothermal therapy for the treatment of glioblastoma: potential and preclinical challenges. Front Oncol. 2021; 10:610356. PMID:
33520720.

10. Doughty ACV, Hoover AR, Layton E, Murray CK, Howard EW, Chen WR. Nanomaterial applications in photothermal therapy for cancer. Materials (Basel). 2019; 12:779.

11. Liu Y, Bhattarai P, Dai Z, Chen X. Photothermal therapy and photoacoustic imaging via nanotheranostics in fighting cancer. Chem Soc Rev. 2019; 48:2053–2108. PMID:
30259015.

12. Chu KF, Dupuy DE. Thermal ablation of tumours: biological mechanisms and advances in therapy. Nat Rev Cancer. 2014; 14:199–208. PMID:
24561446.

13. Hirschberg H, Berg K, Peng Q. Photodynamic therapy mediated immune therapy of brain tumors. Neuroimmunol Neuroinflamm. 2018; 5:27. PMID:
30221185.

14. Kaneko S, Fujimoto S, Yamaguchi H, Yamauchi T, Yoshimoto T, Tokuda K. Photodynamic therapy of malignant gliomas. Prog Neurol Surg. 2018; 32:1–13. PMID:
29990969.

15. Akimoto J, Haraoka J, Aizawa K. Preliminary clinical report on safety and efficacy of photodynamic therapy using talaporfin sodium for malignant gliomas. Photodiagnosis Photodyn Ther. 2012; 9:91–99. PMID:
22594978.

16. Hussein EA, Zagho MM, Nasrallah GK, Elzatahry AA. Recent advances in functional nanostructures as cancer photothermal therapy. Int J Nanomedicine. 2018; 13:2897–2906. PMID:
29844672.

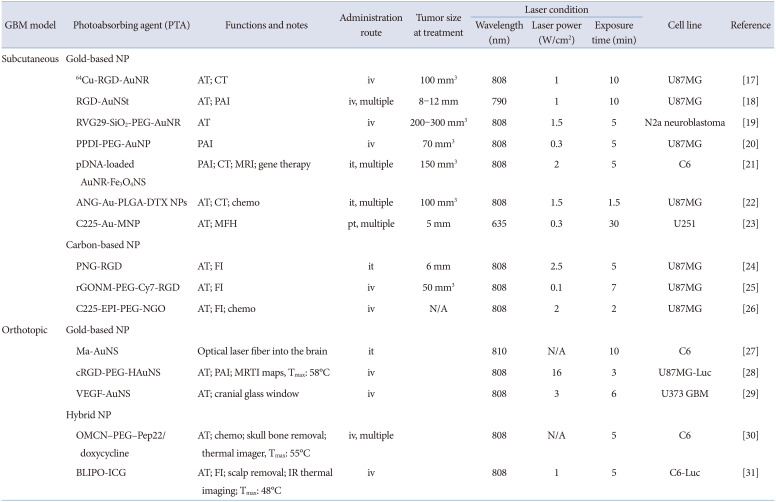
17. Sun X, Huang X, Yan X, Wang Y, Guo J, Jacobson O, et al. Chelator-free (64)Cu-integrated gold nanomaterials for positron emission tomography imaging guided photothermal cancer therapy. ACS Nano. 2014; 8:8438–8446. PMID:
25019252.

18. Nie L, Wang S, Wang X, Rong P, Ma Y, Liu G, et al. In vivo volumetric photoacoustic molecular angiography and therapeutic monitoring with targeted plasmonic nanostars. Small. 2014; 10:1585–1593. PMID:
24150920.

19. Lee C, Hwang HS, Lee S, Kim B, Kim JO, Oh KT, et al. Rabies virus-inspired silica-coated gold nanorods as a photothermal therapeutic platform for treating brain tumors. Adv Mater. 2017; 29:1605563.

20. Yang Z, Song J, Dai Y, Chen J, Wang F, Lin L, et al. Self-assembly of semiconducting-plasmonic gold nanoparticles with enhanced optical property for photoacoustic imaging and photothermal therapy. Theranostics. 2017; 7:2177–2185. PMID:
28740543.

21. Hu Y, Zhou Y, Zhao N, Liu F, Xu FJ. Multifunctional pDNA-conjugated polycationic Au nanorod-coated Fe3O4 hierarchical nanocomposites for trimodal imaging and combined photothermal/gene therapy. Small. 2016; 12:2459–2468. PMID:
26996155.

22. Wang L, Hu Y, Hao Y, Li L, Zheng C, Zhao H, et al. Tumor-targeting core-shell structured nanoparticles for drug procedural controlled release and cancer sonodynamic combined therapy. J Control Release. 2018; 286:74–84. PMID:
30026078.

23. Lu Q, Dai X, Zhang P, Tan X, Zhong Y, Yao C, et al. Fe3O4@Au composite magnetic nanoparticles modified with cetuximab for targeted magneto-photothermal therapy of glioma cells. Int J Nanomedicine. 2018; 13:2491–2505. PMID:
29719396.
24. Su S, Wang J, Vargas E, Wei J, Martínez-Zaguilán R, Sennoune SR, et al. Porphyrin immobilized nanographene oxide for enhanced and targeted photothermal therapy of brain cancer. ACS Biomater Sci Eng. 2016; 2:1357–1366. PMID:
33434989.

25. Akhavan O, Ghaderi E. Graphene nanomesh promises extremely efficient in vivo photothermal therapy. Small. 2013; 9:3593–3601. PMID:
23625739.

26. Yang HW, Lu YJ, Lin KJ, Hsu SC, Huang CY, She SH, et al. EGRF conjugated PEGylated nanographene oxide for targeted chemotherapy and photothermal therapy. Biomaterials. 2013; 34:7204–7214. PMID:
23800742.

27. Madsen SJ, Christie C, Hong SJ, Trinidad A, Peng Q, Uzal FA, et al. Nanoparticle-loaded macrophage-mediated photothermal therapy: potential for glioma treatment. Lasers Med Sci. 2015; 30:1357–1365. PMID:
25794592.

28. Lu W, Melancon MP, Xiong C, Huang Q, Elliott A, Song S, et al. Effects of photoacoustic imaging and photothermal ablation therapy mediated by targeted hollow gold nanospheres in an orthotopic mouse xenograft model of glioma. Cancer Res. 2011; 71:6116–6121. PMID:
21856744.

29. Day ES, Zhang L, Thompson PA, Zawaski JA, Kaffes CC, Gaber MW, et al. Vascular-targeted photothermal therapy of an orthotopic murine glioma model. Nanomedicine (Lond). 2012; 7:1133–1148. PMID:
22583571.

30. Qian W, Qian M, Wang Y, Huang J, Chen J, Ni L, et al. Combination glioma therapy mediated by a dual-targeted delivery system constructed using OMCN-PEG-Pep22/DOX. Small. 2018; 14:e1801905. PMID:
30346089.
31. Jia Y, Wang X, Hu D, Wang P, Liu Q, Zhang X, et al. Correction to phototheranostics: active targeting of orthotopic glioma using biomimetic proteolipid nanoparticles. ACS Nano. 2021; 15:10733. PMID:
34106690.

32. Riley RS, Day ES. Gold nanoparticle-mediated photothermal therapy: applications and opportunities for multimodal cancer treatment. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2017; 9:e1449.

33. Kennedy LC, Bickford LR, Lewinski NA, Coughlin AJ, Hu Y, Day ES, et al. A new era for cancer treatment: gold-nanoparticle-mediated thermal therapies. Small. 2011; 7:169–183. PMID:
21213377.

34. Kim HS, Seo M, Park TE, Lee DY. A novel therapeutic strategy of multimodal nanoconjugates for state-of-the-art brain tumor phototherapy. J Nanobiotechnology. 2022; 20:14. PMID:
34983539.

35. Lin J, Wang S, Huang P, Wang Z, Chen S, Niu G, et al. Photosensitizer-loaded gold vesicles with strong plasmonic coupling effect for imaging-guided photothermal/photodynamic therapy. ACS Nano. 2013; 7:5320–5329. PMID:
23721576.

36. Jang B, Park JY, Tung CH, Kim IH, Choi Y. Gold nanorod-photosensitizer complex for near-infrared fluorescence imaging and photodynamic/photothermal therapy in vivo. ACS Nano. 2011; 5:1086–1094. PMID:
21244012.

37. Vankayala R, Lin CC, Kalluru P, Chiang CS, Hwang KC. Gold nanoshells-mediated bimodal photodynamic and photothermal cancer treatment using ultra-low doses of near infra-red light. Biomaterials. 2014; 35:5527–5538. PMID:
24731706.

38. Sun J, Guo Y, Xing R, Jiao T, Zou Q, Yan X. Synergistic in vivo photodynamic and photothermal antitumor therapy based on collagen-gold hybrid hydrogels with inclusion of photosensitive drugs. Colloids Surf A Physicochem Eng Asp. 2017; 514:155–160.

39. Ensign LM, Cone R, Hanes J. Oral drug delivery with polymeric nanoparticles: the gastrointestinal mucus barriers. Adv Drug Deliv Rev. 2012; 64:557–570. PMID:
22212900.

40. Pawar VK, Meher JG, Singh Y, Chaurasia M, Surendar Reddy B, Chourasia MK. Targeting of gastrointestinal tract for amended delivery of protein/peptide therapeutics: strategies and industrial perspectives. J Control Release. 2014; 196:168–183. PMID:
25305562.

41. Pridgen EM, Alexis F, Farokhzad OC. Polymeric nanoparticle technologies for oral drug delivery. Clin Gastroenterol Hepatol. 2014; 12:1605–1610. PMID:
24981782.

42. Tang WL, Tang WH, Chen WC, Diako C, Ross CF, Li SD. Development of a rapidly dissolvable oral pediatric formulation for mefloquine using liposomes. Mol Pharm. 2017; 14:1969–1979. PMID:
28460165.

43. Song Z, Lin Y, Zhang X, Feng C, Lu Y, Gao Y, et al. Cyclic RGD peptide-modified liposomal drug delivery system for targeted oral apatinib administration: enhanced cellular uptake and improved therapeutic effects. Int J Nanomedicine. 2017; 12:1941–1958. PMID:
28331317.

44. Liu Y, Luo X, Xu X, Gao N, Liu X. Preparation, characterization and in vivo pharmacokinetic study of PVP-modified oleanolic acid liposomes. Int J Pharm. 2017; 517:1–7. PMID:
27899320.

45. Sze LP, Li HY, Lai KLA, Chow SF, Li Q, KennethTo KW, et al. Oral delivery of paclitaxel by polymeric micelles: a comparison of different block length on uptake, permeability and oral bioavailability. Colloids Surf B Biointerfaces. 2019; 184:110554. PMID:
31627103.

46. Jeong Y, Lee D, Choe K, Ahn H, Kim P, Park JH, et al. Polypeptide-based polyelectrolyte complexes overcoming the biological barriers of oral insulin delivery. J Ind Eng Chem. 2017; 48:79–87.

47. Lee E, Lee J, Lee IH, Yu M, Kim H, Chae SY, et al. Conjugated chitosan as a novel platform for oral delivery of paclitaxel. J Med Chem. 2008; 51:6442–6449. PMID:
18826299.

48. Kebede A, Singh AK, Rai PK, Giri NK, Rai AK, Watal G, et al. Controlled synthesis, characterization, and application of iron oxide nanoparticles for oral delivery of insulin. Lasers Med Sci. 2013; 28:579–587. PMID:
22581389.

49. Kong FY, Zhang JW, Li RF, Wang ZX, Wang WJ, Wang W. Unique roles of gold nanoparticles in drug delivery, targeting and imaging applications. Molecules. 2017; 22:1445.

50. Sung HW, Sonaje K, Liao ZX, Hsu LW, Chuang EY. pH-responsive nanoparticles shelled with chitosan for oral delivery of insulin: from mechanism to therapeutic applications. Acc Chem Res. 2012; 45:619–629. PMID:
22236133.

51. des Rieux A, Fievez V, Garinot M, Schneider YJ, Préat V. Nanoparticles as potential oral delivery systems of proteins and vaccines: a mechanistic approach. J Control Release. 2006; 116:1–27. PMID:
17050027.

52. Yun Y, Cho YW, Park K. Nanoparticles for oral delivery: targeted nanoparticles with peptidic ligands for oral protein delivery. Adv Drug Deliv Rev. 2013; 65:822–832. PMID:
23123292.

53. Banerjee A, Qi J, Gogoi R, Wong J, Mitragotri S. Role of nanoparticle size, shape and surface chemistry in oral drug delivery. J Control Release. 2016; 238:176–185. PMID:
27480450.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download