1. Ostrom QT, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2014-2018. Neuro Oncol. 2021; 23(12 Suppl 2):iii1–iii105. PMID:
34608945.

2. Ohgaki H, Dessen P, Jourde B, Horstmann S, Nishikawa T, Di Patre PL, et al. Genetic pathways to glioblastoma: a population-based study. Cancer Res. 2004; 64:6892–6899. PMID:
15466178.
3. Ladomersky E, Zhai L, Lauing KL, Bell A, Xu J, Kocherginsky M, et al. Advanced age increases immunosuppression in the brain and decreases immunotherapeutic efficacy in subjects with glioblastoma. Clin Cancer Res. 2020; 26:5232–5245. PMID:
32546647.

4. Wee CW, Kim E, Kim N, Kim IA, Kim TM, Kim YJ, et al. Novel recursive partitioning analysis classification for newly diagnosed glioblastoma: a multi-institutional study highlighting the MGMT promoter methylation and IDH1 gene mutation status. Radiother Oncol. 2017; 123:106–111. PMID:
28302331.

5. Wen PY, Weller M, Lee EQ, Alexander BM, Barnholtz-Sloan JS, Barthel FP, et al. Glioblastoma in adults: a Society for Neuro-Oncology (SNO) and European Society of Neuro-Oncology (EANO) consensus review on current management and future directions. Neuro Oncol. 2020; 22:1073–1113. PMID:
32328653.

6. Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005; 352:987–996. PMID:
15758009.

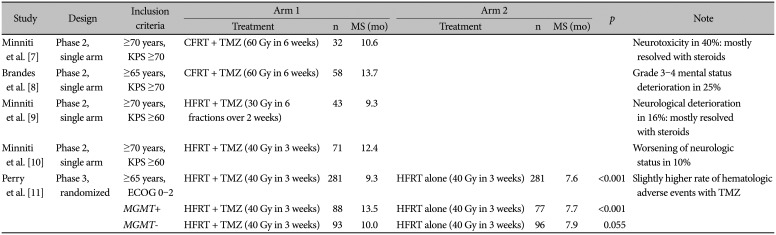
7. Minniti G, De Sanctis V, Muni R, Filippone F, Bozzao A, Valeriani M, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma in elderly patients. J Neurooncol. 2008; 88:97–103. PMID:
18250965.

8. Brandes AA, Franceschi E, Tosoni A, Benevento F, Scopece L, Mazzocchi V, et al. Temozolomide concomitant and adjuvant to radiotherapy in elderly patients with glioblastoma: correlation with MGMT promoter methylation status. Cancer. 2009; 115:3512–3518. PMID:
19514084.

9. Minniti G, De Sanctis V, Muni R, Rasio D, Lanzetta G, Bozzao A, et al. Hypofractionated radiotherapy followed by adjuvant chemotherapy with temozolomide in elderly patients with glioblastoma. J Neurooncol. 2009; 91:95–100. PMID:
18758912.

10. Minniti G, Lanzetta G, Scaringi C, Caporello P, Salvati M, Arcella A, et al. Phase II study of short-course radiotherapy plus concomitant and adjuvant temozolomide in elderly patients with glioblastoma. Int J Radiat Oncol Biol Phys. 2012; 83:93–99. PMID:
22079725.
11. Perry JR, Laperriere N, O’Callaghan CJ, Brandes AA, Menten J, Phillips C, et al. Short-course radiation plus temozolomide in elderly patients with glioblastoma. N Engl J Med. 2017; 376:1027–1037. PMID:
28296618.
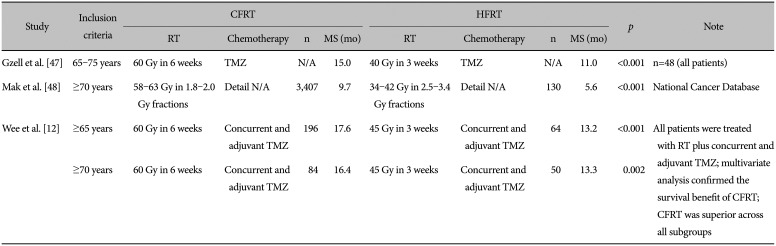
12. Wee CW, Kim IH, Park CK, Kim N, Suh CO, Chang JH, et al. Chemoradiation in elderly patients with glioblastoma from the multi-institutional GBM-molRPA cohort: is short-course radiotherapy enough or is it a matter of selection? J Neurooncol. 2020; 148:57–65. PMID:
32361863.
13. Cloney M, D’Amico R, Lebovic J, Nazarian M, Zacharia BE, Sisti MB, et al. Frailty in geriatric glioblastoma patients: a predictor of operative morbidity and outcome. World Neurosurg. 2016; 89:362–367. PMID:
26775233.
14. Gavrilovic IT, Hormigo A, Yahalom J, DeAngelis LM, Abrey LE. Long-term follow-up of high-dose methotrexate-based therapy with and without whole brain irradiation for newly diagnosed primary CNS lymphoma. J Clin Oncol. 2006; 24:4570–4574. PMID:
17008697.
15. Nunna RS, Khalid SI, Patel S, Sethi A, Behbahani M, Mehta AI, et al. Outcomes and patterns of care in elderly patients with glioblastoma multiforme. World Neurosurg. 2021; 149:e1026–e1037. PMID:
33482415.
16. Koh HK, Kim H, Hong S. Patterns of care after surgery for elderly patients with malignant brain tumors: data from the National Health Insurance Service in South Korea. Anticancer Res. 2019; 39:5733–5739. PMID:
31570475.
18. Lopez-Rivera V, Dono A, Lewis CT, Chandra A, Abdelkhaleq R, Sheth SA, et al. Extent of resection and survival outcomes of geriatric patients with glioblastoma: is there benefit from aggressive surgery? Clin Neurol Neurosurg. 2021; 202:106474. PMID:
33454497.
19. Han Q, Liang H, Cheng P, Yang H, Zhao P. Gross total vs. subtotal resection on survival outcomes in elderly patients with high-grade glioma: a systematic review and meta-analysis. Front Oncol. 2020; 10:151. PMID:
32257941.
20. Straube C, Kessel KA, Antoni S, Gempt J, Meyer B, Schlegel J, et al. A balanced score to predict survival of elderly patients newly diagnosed with glioblastoma. Radiat Oncol. 2020; 15:97. PMID:
32375830.
21. Song AJ, Ding K, Alnahhas I, Laperriere NJ, Perry J, Mason WP, et al. Impact of lymphopenia on survival for elderly patients with glioblastoma: a secondary analysis of the CCTG CE.6 (EORTC 26062-22061, TROG03.01) randomized clinical trial. Neurooncol Adv. 2021; 3:vdab153. PMID:
34765975.
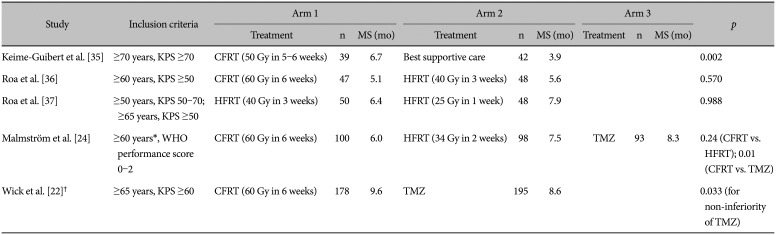
22. Wick W, Platten M, Meisner C, Felsberg J, Tabatabai G, Simon M, et al. Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the NOA-08 randomised, phase 3 trial. Lancet Oncol. 2012; 13:707–715. PMID:
22578793.
23. Wick A, Kessler T, Platten M, Meisner C, Bamberg M, Herrlinger U, et al. Superiority of temozolomide over radiotherapy for elderly patients with RTK II methylation class, MGMT promoter methylated malignant astrocytoma. Neuro Oncol. 2020; 22:1162–1172. PMID:
32064499.
24. Malmström A, Grønberg BH, Marosi C, Stupp R, Frappaz D, Schultz H, et al. Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic randomised, phase 3 trial. Lancet Oncol. 2012; 13:916–926. PMID:
22877848.
25. Reifenberger G, Hentschel B, Felsberg J, Schackert G, Simon M, Schnell O, et al. Predictive impact of MGMT promoter methylation in glioblastoma of the elderly. Int J Cancer. 2012; 131:1342–1350. PMID:
22139906.
26. Kleinberg L, Sloan L, Grossman S, Lim M. Radiotherapy, lymphopenia, and host immune capacity in glioblastoma: a potentially actionable toxicity associated with reduced efficacy of radiotherapy. Neurosurgery. 2019; 85:441–453. PMID:
31232425.
27. McMahon SJ. The linear quadratic model: usage, interpretation and challenges. Phys Med Biol. 2018; 64:01TR01.
28. Pedicini P, Fiorentino A, Simeon V, Tini P, Chiumento C, Pirtoli L, et al. Clinical radiobiology of glioblastoma multiforme: estimation of tumor control probability from various radiotherapy fractionation schemes. Strahlenther Onkol. 2014; 190:925–932. PMID:
24699988.
29. Walker MD, Strike TA, Sheline GE. An analysis of dose-effect relationship in the radiotherapy of malignant gliomas. Int J Radiat Oncol Biol Phys. 1979; 5:1725–1731. PMID:
231022.

30. Bleehen NM, Stenning SP. A Medical Research Council trial of two radiotherapy doses in the treatment of grades 3 and 4 astrocytoma. Br J Cancer. 1991; 64:769–774. PMID:
1654987.
31. Weller M, van den Bent M, Preusser M, Le Rhun E, Tonn JC, Minniti G, et al. EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat Rev Clin Oncol. 2021; 18:170–186. PMID:
33293629.
32. Kim YZ, Kim CY, Lim J, Sung KS, Lee J, Oh HJ, et al. The Korean Society for Neuro-Oncology (KSNO) guideline for glioblastomas: version 2018.01. Brain Tumor Res Treat. 2019; 7:1–9. PMID:
31062525.

34. Cabrera AR, Kirkpatrick JP, Fiveash JB, Shih HA, Koay EJ, Lutz S, et al. Radiation therapy for glioblastoma: executive summary of an American Society for radiation oncology evidence-based clinical practice guideline. Pract Radiat Oncol. 2016; 6:217–225. PMID:
27211230.
35. Keime-Guibert F, Chinot O, Taillandier L, Cartalat-Carel S, Frenay M, Kantor G, et al. Radiotherapy for glioblastoma in the elderly. N Engl J Med. 2007; 356:1527–1535. PMID:
17429084.

36. Roa W, Brasher PM, Bauman G, Anthes M, Bruera E, Chan A, et al. Abbreviated course of radiation therapy in older patients with glioblastoma multiforme: a prospective randomized clinical trial. J Clin Oncol. 2004; 22:1583–1588. PMID:
15051755.
37. Roa W, Kepka L, Kumar N, Sinaika V, Matiello J, Lomidze D, et al. International Atomic Energy Agency randomized phase III study of radiation therapy in elderly and/or frail patients with newly diagnosed glioblastoma multiforme. J Clin Oncol. 2015; 33:4145–4150. PMID:
26392096.

38. Bernhardt D, Wick W, Weiss SE, Sahgal A, Lo SS, Suh JH, et al. Neurooncology management during the COVID-19 pandemic with a focus on WHO grades III and IV gliomas. Neuro Oncol. 2020; 22:928–935.

39. Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005; 352:997–1003. PMID:
15758010.
40. Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009; 10:459–466. PMID:
19269895.

41. Kil WJ, Cerna D, Burgan WE, Beam K, Carter D, Steeg PS, et al. In vitro and in vivo radiosensitization induced by the DNA methylating agent temozolomide. Clin Cancer Res. 2008; 14:931–938. PMID:
18245557.

42. Herrlinger U, Tzaridis T, Mack F, Steinbach JP, Schlegel U, Sabel M, et al. Lomustine-temozolomide combination therapy versus standard temozolomide therapy in patients with newly diagnosed glioblastoma with methylated MGMT promoter (CeTeG/NOA-09): a randomised, open-label, phase 3 trial. Lancet. 2019; 393:678–688. PMID:
30782343.

43. Franceschi E, Depenni R, Paccapelo A, Ermani M, Faedi M, Sturiale C, et al. Which elderly newly diagnosed glioblastoma patients can benefit from radiotherapy and temozolomide? A PERNO prospective study. J Neurooncol. 2016; 128:157–162. PMID:
26943851.
44. Arakawa Y, Sasaki K, Mineharu Y, Uto M, Mizowaki T, Mizusawa J, et al. A randomized phase III study of short-course radiotherapy combined with Temozolomide in elderly patients with newly diagnosed glioblastoma; Japan clinical oncology group study JCOG1910 (AgedGlio-PIII). BMC Cancer. 2021; 21:1105. PMID:
34654402.

45. Arvold ND, Tanguturi SK, Aizer AA, Wen PY, Reardon DA, Lee EQ, et al. Hypofractionated versus standard radiation therapy with or without temozolomide for older glioblastoma patients. Int J Radiat Oncol Biol Phys. 2015; 92:384–389. PMID:
25841623.

46. Navarria P, Pessina F, Franzese C, Loi M, Bellu L, Clerici E, et al. The 70-year-old newly diagnosed glioblastoma patients are older than the 65-year-old? Outcome evaluation of the two categories in a matched case control study with propensity score balancing. Radiother Oncol. 2021; 156:49–55. PMID:
33245946.

47. Gzell C, Wheeler H, Guo L, Kastelan M, Back M. Elderly patients aged 65-75 years with glioblastoma multiforme may benefit from long course radiation therapy with temozolomide. J Neurooncol. 2014; 119:187–196. PMID:
24830984.

48. Mak KS, Agarwal A, Qureshi MM, Truong MT. Hypofractionated short-course radiotherapy in elderly patients with glioblastoma multiforme: an analysis of the National Cancer Database. Cancer Med. 2017; 6:1192–1200. PMID:
28440040.

49. Mohile SG, Dale W, Somerfield MR, Schonberg MA, Boyd CM, Burhenn PS, et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology. J Clin Oncol. 2018; 36:2326–2347. PMID:
29782209.

50. Flannery MA, Culakova E, Canin BE, Peppone L, Ramsdale E, Mohile SG. Understanding treatment tolerability in older adults with cancer. J Clin Oncol. 2021; 39:2150–2163. PMID:
34043433.

51. Mohile SG, Mohamed MR, Xu H, Culakova E, Loh KP, Magnuson A, et al. Evaluation of geriatric assessment and management on the toxic effects of cancer treatment (GAP70+): a cluster-randomised study. Lancet. 2021; 398:1894–1904. PMID:
34741815.

52. Spina M, Balzarotti M, Uziel L, Ferreri AJ, Fratino L, Magagnoli M, et al. Modulated chemotherapy according to modified comprehensive geriatric assessment in 100 consecutive elderly patients with diffuse large B-cell lymphoma. Oncologist. 2012; 17:838–846. PMID:
22610154.

53. Corre R, Greillier L, Le Caër H, Audigier-Valette C, Baize N, Bérard H, et al. Use of a comprehensive geriatric assessment for the management of elderly patients with advanced non–small-cell lung cancer: the phase III randomized ESOGIA-GFPC-GECP 08-02 study. J Clin Oncol. 2016; 34:1476–1483. PMID:
26884557.

54. Deluche E, Leobon S, Lamarche F, Tubiana-Mathieu N. First validation of the G-8 geriatric screening tool in older patients with glioblastoma. J Geriatr Oncol. 2019; 10:159–163. PMID:
30037767.

55. Mathen P, Rowe L, Mackey M, Smart D, Tofilon P, Camphausen K. Radiosensitizers in the temozolomide era for newly diagnosed glioblastoma. Neurooncol Pract. 2020; 7:268–276. PMID:
32537176.

56. Majd NK, Yap TA, Koul D, Balasubramaniyan V, Li X, Khan S, et al. The promise of DNA damage response inhibitors for the treatment of glioblastoma. Neurooncol Adv. 2021; 3:vdab015. PMID:
33738447.

57. Singh R, Lehrer EJ, Wang M, Perlow HK, Zaorsky NG, Trifiletti DM, et al. Dose escalated radiation therapy for glioblastoma multiforme: an international systematic review and meta-analysis of 22 prospective trials. Int J Radiat Oncol Biol Phys. 2021; 111:371–384. PMID:
33991621.

58. Laprie A, Ken S, Filleron T, Lubrano V, Vieillevigne L, Tensaouti F, et al. Dose-painting multicenter phase III trial in newly diagnosed glioblastoma: the SPECTRO-GLIO trial comparing arm A standard radiochemotherapy to arm B radiochemotherapy with simultaneous integrated boost guided by MR spectroscopic imaging. BMC Cancer. 2019; 19:167. PMID:
30791889.

59. Laprie A, Noel G, Chaltiel L, Truc G, Sunyach MP, Charissoux M, et al. Dose-painting multicenter phase III trial in newly diagnosed glioblastoma: the SPECTRO-GLIO trial. Radiother Oncol. 2021; 161(Suppl 1):S246–S247.
60. Perlow HK, Yang M, Klamer B, Raval R, Blakaj DM, Arnett ALH, et al. Hypofractionated dose-escalation for elderly patients with a newly diagnosed glioblastoma improves survival. Int J Radiat Oncol Biol Phys. 2021; 111(3 Suppl):e597–e598.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download