INTRODUCTION
Inflammatory bowel disease (IBD), which mainly comprises UC and CD, is characterized by chronic repetitive bowel inflammation that requires life-long treatment.
1 Although IBD prevails in Western countries, recent studies have shown that the incidence of the disease has significantly increased over the past several decades in Asia.
2
3 This change in Asia may be the result of Westernized diet, improved hygiene, increasing use of antibiotics, or changes in the gut microbiota.
4
IBD is a unique and disabling condition that often demands the care of gastroenterology specialists. Indeed, many studies on IBD in the literature have been conducted in tertiary referral centers (TRCs).
5 However, little is known about the clinical features and management of patients with IBD in primary or secondary care units. We surmise that there must be a difference in the characteristics and treatments between patients in secondary hospitals (SHs) and those in TRCs. It would be clinically relevant to understand if there are any disparities for better understanding of IBD patients as a whole and for setting up an appropriate management strategy for patients who were referred from primary or SHs. Therefore, we aimed to compare the demographic and clinical characteristics of IBD patients from a SH with those from TRCs. The steroid, immunomodulator and anti-tumor necrosis factor (anti-TNF) use pattern for patients with IBD was also compared between the 2 groups.
Go to :

METHODS
1. Subjects
The medical records of patients with CD and UC from an SH and 2 TRCs were reviewed retrospectively by 2 gastroenterology specialists (E.S.K. and K.O.K.). The SH had general physicians and surgeons while the 2 TRCs had specialized gastroenterology units including the department of gastroenterology and the department of surgery and only received referred patients from primary or SHs. Their diagnoses were made between January of 2011 and March of 2015. Patients older than 18 years and who were followed up with at least more than 6 months after diagnosis were included in the study. The disease diagnosis was based on a thorough clinical history taking, physical examination, laboratory investigations, endoscopic assessment, radiologic findings, and pathology assessment according to the Korean guidelines of IBD diagnosis.
6
7
The Institutional Review Boards from all of the hospitals approved this study (DSMC2015-06-003).
The informed consent from patients was waived because this was a retrospective study.
2. Variables
Variables included age at diagnosis, sex, initial symptoms and history of medications, such as steroid exposure, thiopurine, and anti-TNF. Initial CD symptoms included perianal symptoms, such as anal discharge or painful anal swelling, and luminal symptoms, such as abdominal pain, diarrhea, or body weight loss. The UC symptoms consisted of hematochezia, diarrhea, abdominal pain, or body weight loss. For CD, the locations were classified as ileal (L1), colonic (L2) or ileocolonic (L3), and the behaviors were categorized as inflammatory (B1), stricturing (B2) or penetrating (B3) in correspondence with the Montreal classification. Perianal disease, including perianal fistula or abscess, was also recorded. However, hemorrhoids and skin tag were not included in the definition of perianal disease. For UC, the extent of the disease was assessed as proctitis (E1), left sided (E2), or extensive (E3) according to the Montreal classification as well.
3. Statistical Analysis
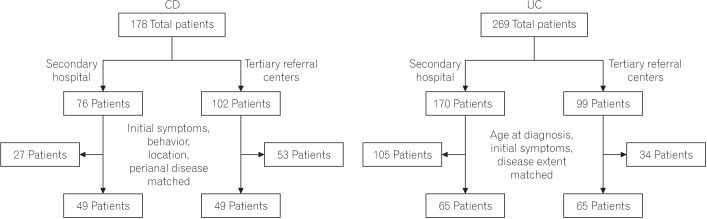
For categorical variables, Fisher exact or chi-square tests were used to assess the differences between the groups. For non-categorical variables, the Mann-Whitney U test was used and they were described as medians and ranges. The treatments patterns were analyzed after controlling for different baseline clinical characteristics, such as initial symptoms, disease behavior, CD location, extent of UC, and age at diagnosis using propensity score matching between the 2 groups. Propensity scores were estimated using a logistic regression analysis. A Kaplan-Meier analysis with the log-rank test was applied to describe cumulative use of thiopurine and anti-TNF between the groups. A two-tailed P-value <0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA).
Go to :

DISCUSSION
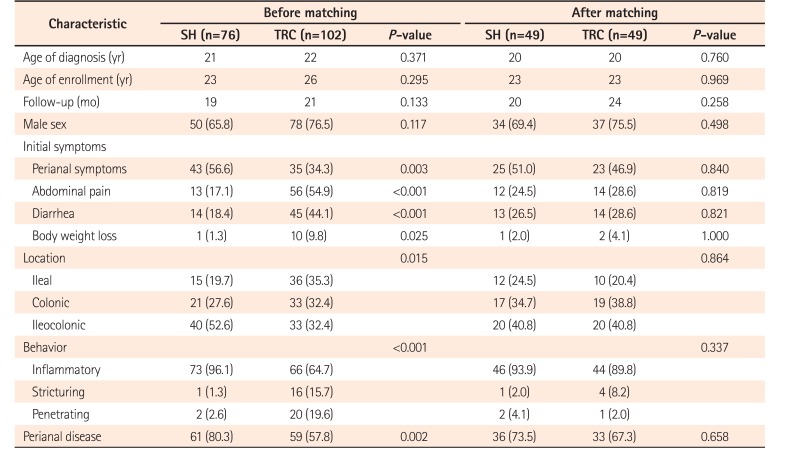
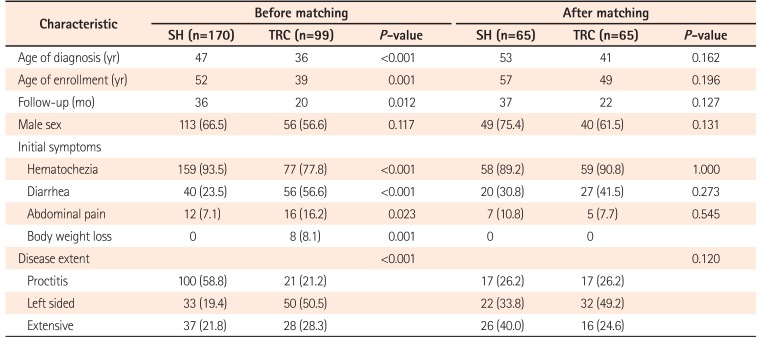
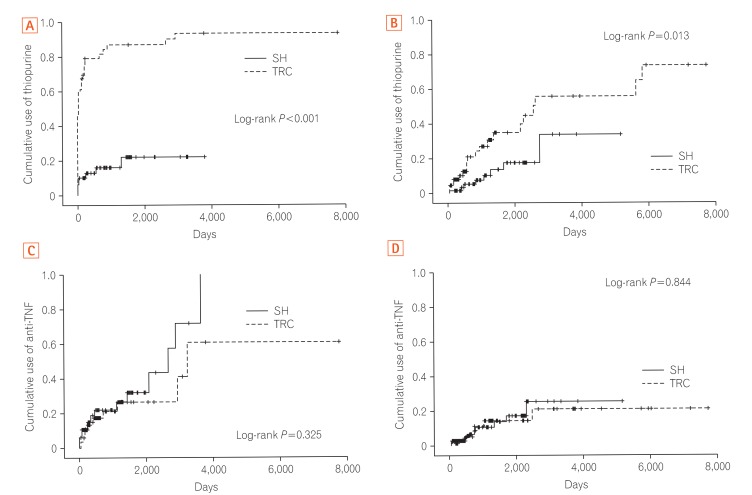
We found that there was a significant difference in the clinical characteristics of patients with IBD from a secondary care unit and from TRCs. The CD patients in the SH were more likely to have perianal disease-related problems whereas the CD patients in the TRCs had ileal location and complicating behaviors more frequently compared with the SH. Additionally, the UC patients in the SH were more likely to have a limited extent of the disease compared with those in the TRCs. Moreover, there was a substantial gap in the treatment behavior for patients with IBD between the SH and TRCs. After controlling for different characteristics using propensity score matching, the cumulative use of thiopurine for both CD and UC in the SH group was significantly lower than that in the TRC group.
To the best of our knowledge, this is the first study to compare the clinical features and management of patients with IBD between a secondary care unit and TRCs using a propensity score matching system. Although IBD is perceived as a condition that usually requires management by gastroenterology specialists in referral centers, the role of primary or secondary care units is recognized as essential in the long-term care of patients with IBD.
8 Further, issues in the communication between health care services for patients with IBD have been highlighted.
9 Therefore, it is imperative to understand the characteristics and management behaviors of patients with IBD before they get to referral centers.
Interestingly, this study showed that the SH group had more CD patients who had perianal fistulas than in the TRCs. Although the exact cause is unclear, accessibility to each health care service might contribute to this difference. For instance, patients who had anal discharge or painful anal swelling usually go to the Department of Surgery and, from the patients' perspective, secondary care hospitals are more accessible than TRCs. This finding is noteworthy because perianal disease is known as a peculiar feature of Korean CD patients as they more frequently have perianal disease than in Western countries.
10 In contrast, complicating behaviors, such as stricturing or penetrating, and ileal location were more frequently observed in the TRC group. This is not surprising, as referral centers address more serious patients who are referred from primary or SHs. Ileal location is a well-known indicator of poor clinical CD outcomes.
11 The result that the SH was more likely to have a limited extent of UC is also a reflection of this aspect, as proctitis is related to a mild UC disease course.
12 Likewise, the UC patients in the TRCs were younger at the time of diagnosis than those of the SH, indicating more adverse clinical outcomes in the TRC group, as younger diagnosis ages are known to be related with poor clinical outcomes for UC.
13
14
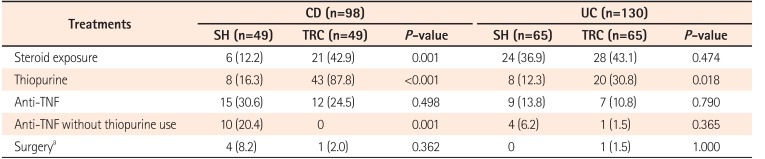
Regarding the UC patients, steroid exposure was not different between the SH and TRC groups after controlling for baseline characteristics with propensity score matching. However, cumulative thiopurine use for UC in the SH was significantly lower than in the TRCs (
Fig. 2B). This was also true for the management of CD. Cumulative thiopurine use for CD in the SH was much lower than the TRCs after matching between the groups (
Fig. 2A). In addition, the use of anti-TNF without thiopurine therapy was more common in the SH than in the TRCs (20.4% vs. 0% for CD; 6.2% vs. 1.5% for UC) (
Table 3). Although the exact reason of the underuse of thiopurine in the SH is unknown, it might be explained by the considerable adverse effects of thiopurine, including bone marrow suppression, hepatotoxicity, and increased risk of opportunistic infections and malignancies, which are difficult for physicians in SHs to handle.
8 In particular, leukopenia occurrences are the main obstacle to thiopurine use in clinical practice, as it requires tight laboratory white blood cell monitoring.
15 Indeed, the risk of thiopurine-induced leukopenia is much higher in Asians, including Koreans (~35.4%),
16
17 than in Western countries (~5%).
18
19 Therefore, Korean physicians might be more reluctant to use thiopurine for IBD management in their clinical practice. Another plausible explanation for inadequate use of thiopurine in the SH might be related with the Korean medical reimbursement system. According to the Korean National Health Insurance Service, thiopurine failure is required before anti-TNF therapy for luminal CD, indicating that thiopurine treatment is prerequisite for use of anti-TNF. However, thiopurine treatment is not necessarily mandatory before anti-TNF therapy for perianal CD or UC. Hence, the use of anti-TNF seems to be more liable without consideration of response to thiopurine in perianal CD or UC than luminal CD in Korea.
A robust effort is required to determine the exact hurdles for the underuse of thiopurine for IBD management by physicians in primary or secondary care units and to provide them with education for optimal thiopurine use. Recently, a consensus statement has been developed for guiding the appropriate use of thiopurine in IBD, which are more suitable for Korean patients.
20 Further, several genetic biomarkers for predicting thiopurine-induced leukopenia confirmed in Korean studies might be helpful to use thiopurine properly in the management of Korean patients with IBD.
16
21 These genetic biomarkers are particularly useful for physicians working at SH in the light of their concern of thiopurine-induced leukopenia.
This study had several limitations. First, there might be a selection bias inherent to the retrospective study design. Second, although we used a propensity score matching method to control for the disease phenotypes, it might not have fully regulated the differences in disease severity. However, a validated assessment of disease severity was not available in the retrospective setting. A successful control of disease severity between the groups in our study might be reflected by a similar anti-TNF use rate and surgery rate in both groups after propensity matching, which are one of indicators for disease severity.
22 Third, the SH in this study is specialized in coloproctology although it has many other departments as well. Therefore, it might be difficult to generalize data of the study. Further study with more data from primary or secondary care hospitals is needed.
In conclusion, the clinical characteristics and management of patients with IBD in the SH were different from the TRCs. The SH was more focused on the perianal disease for CD, whereas the TRCs had more complicating behaviors and ileal location. For UC, patients in the SH had a more limited extent compared with those in the TRCs. Overall, patients with IBD in the SH were less likely to receive treatment with thiopurine than those in the TRCs after controlling for different baseline characteristics using propensity score matching. Therefore, this study indicates that there is room for improvement in the proper use of thiopurine therapy in the SH.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download