1. Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014; 64:9–29. PMID:
24399786.

2. Katsidzira L, Gangaidzo I, Thomson S, Rusakaniko S, Matenga J, Ramesar R. The shifting epidemiology of colorectal cancer in sub-Saharan Africa. Lancet Gastroenterol Hepatol. 2017; 2:377–383. PMID:
28397702.

3. Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015; 136:E359–E386. PMID:
25220842.

4. Irabor DO. Colorectal carcinoma in West Africans: some considerations on its relatively lower incidence compared to caucasians. Pak J Med Sci. 2008; 24:331–335.
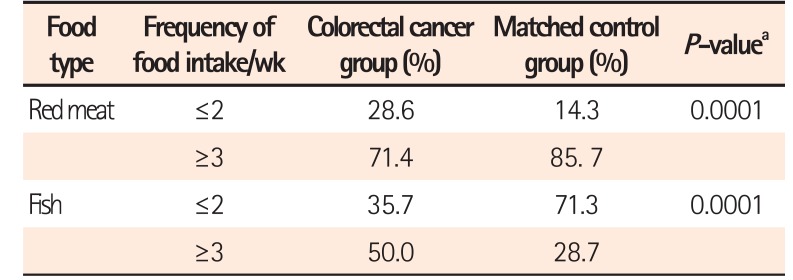
5. O'Keefe SJ, Li JV, Lahti L, et al. Fat, fibre and cancer risk in African Americans and rural Africans. Nat Commun. 2015; 6:6342. DOI:
10.1038/ncomms7342. PMID:
25919227.
6. Tuan J, Chen YX. Dietary and lifestyle factors associated with colorectal cancer risk and interactions with microbiota: fiber, red or processed meat and alcoholic drinks. Gastrointest Tumors. 2016; 3:17–24. PMID:
27722153.

7. Louis P, Hold GL, Flint HJ. The gut microbiota, bacterial metabolites and colorectal cancer. Nat Rev Microbiol. 2014; 12:661–672. PMID:
25198138.

8. Dziedzic K, Szwengiel A, Górecka D, et al. Effect of wheat dietary fiber particle size during digestion in vitro on bile acid, faecal bacteria and short-chain fatty acid content. Plant Foods Hum Nutr. 2016; 71:151–157. PMID:
26924312.

9. Drasar BS, Jenkins DJ. Bacteria, diet, and large bowel cancer. Am J Clin Nutr. 1976; 29:1410–1416. PMID:
998551.

10. Sugawara M, Suzuki K, Endo K, Kumemura M, Takeuchi M, Mitsuoka T. Effect of the dietary supplementation of corn hemicellulose on fecal flora and bacterial enzyme activities in human adults. Agric Biol Chem. 1990; 54:1683–1688.

11. Nagao-Kitamoto H, Kitamoto S, Kuffa P, Kamada N. Pathogenic role of the gut microbiota in gastrointestinal diseases. Intest Res. 2016; 14:127–138. PMID:
27175113.

12. Goering HK, Van Soest PJ. Forage fiber analyses: apparatus, reagents, procedures, and some applications. Washington DC: U.S. Agricultural Research Service;1970.
13. Van Soest PJ, Robertson JB, Lewis BA. Methods for dietary fiber, neutral detergent fiber, and nonstarch polysaccharides in relation to animal nutrition. J Dairy Sci. 1991; 74:3583–3597. PMID:
1660498.

14. Iliyasu Y, Ladipo JK, Akang EE, Adebamowo CA, Ajao OG, Aghadiuno PU. A twenty-year review of malignant colorectal neoplasms at University College Hospital, Ibadan, Nigeria. Dis Colon Rectum. 1996; 39:536–540. PMID:
8620804.

15. Leufkens AM, Van Duijnhoven FJ, Boshuizen HC, et al. Educational level and risk of colorectal cancer in EPIC with specific reference to tumor location. Int J Cancer. 2012; 130:622–630. PMID:
21412763.

16. Uchida K, Kono S, Yin G, et al. Dietary fiber, source foods and colorectal cancer risk: the Fukuoka Colorectal Cancer Study. Scand J Gastroenterol. 2010; 45:1223–1231. PMID:
20500015.

17. Cheah PY, Bernstein H. Colon cancer and dietary fiber: cellulose inhibits the DNA-damaging ability of bile acids. Nutr Cancer. 1990; 13:51–57. PMID:
2153952.

18. Abe SK, Inoue M, Sawada N, et al. Rice, bread, noodle and cereal intake and colorectal cancer in Japanese men and women: the Japan Public Health Center-based prospective Study (JPHC Study). Br J Cancer. 2014; 110:1316–1321. PMID:
24384682.

19. Pérez-Jiménez J, Díaz-Rubio ME, Mesías M, Morales FJ, Saura-Calixto F. Evidence for the formation of maillardized insoluble dietary fiber in bread: a specific kind of dietary fiber in thermally processed food. Food Res Int. 2014; 55:391–396.

20. Skeie G, Braaten T, Olsen A, et al. Whole grain intake and survival among Scandinavian colorectal cancer patients. Nutr Cancer. 2014; 66:6–13. PMID:
24274588.

21. O'Callaghan NJ, Toden S, Bird AR, Topping DL, Fenech M, Conlon MA. Colonocyte telomere shortening is greater with dietary red meat than white meat and is attenuated by resistant starch. Clin Nutr. 2012; 31:60–64. PMID:
21963168.
22. Hall MN, Chavarro JE, Lee IM, Willett WC, Ma J. A 22-year prospective study of fish, n-3 fatty acid intake, and colorectal cancer risk in men. Cancer Epidemiol Biomarkers Prev. 2008; 17:1136–1143. PMID:
18483335.

23. Eltweri AM, Thomas AL, Metcalfe M, Calder PC, Dennison AR, Bowrey DJ. Potential applications of fish oils rich in omega-3 polyunsaturated fatty acids in the management of gastrointestinal cancer. Clin Nutr. 2017; 36:65–78. PMID:
26833289.

24. Rodríguez-Romero N, Abecia L, Fondevila M, et al. Effects of levels of insoluble and soluble fibre in diets for growing rabbits on faecal digestibility, nitrogen recycling and in vitro fermentation. World Rabbit Sci. 2011; 19:85–94.

25. Singh A, Singh SN. Dietary fiber content of Indian diets. Asian J Pharm Clin Res. 2015; 8:58–61.
26. Zhang YJ, Li S, Gan RY, Zhou T, Xu DP, Li HB. Impacts of gut bacteria on human health and diseases. Int J Mol Sci. 2015; 16:7493–7519. PMID:
25849657.

27. Biddle A, Stewart L, Blanchard J, Leschine S. Untangling the genetic basis of fibrolytic specialization by Lachnospiraceae and Ruminococcaceae in diverse gut communities. Diversity. 2013; 5:627–640.

29. Salyers AA, Balascio RJ, Palmer JK. Breakdown of xylan by enzymes from human colonic bacteria. J Food Biochem. 1982; 6:39–55.

30. Sloan DA, Fleiszer DM, Richards GK, Murray D, Brown RA. The effect of the fiber components cellulose and lignin on experimental colon neoplasia. J Surg Oncol. 1993; 52:77–82. PMID:
8385723.

31. Degirolamo C, Modica S, Palasciano G, Moschetta A. Bile acids and colon cancer: solving the puzzle with nuclear receptors. Trends Mol Med. 2011; 17:564–572. PMID:
21724466.

32. Ajouz H, Mukherji D, Shamseddine A. Secondary bile acids: an underrecognized cause of colon cancer. World J Surg Oncol. 2014; 12:164. PMID:
24884764.
33. Lee S, Monnappa AK, Mitchell RJ. Biological activities of lignin hydrolysate-related compounds. BMB Rep. 2012; 45:265–274. PMID:
22617449.
34. Ferguson LR, Harris PJ. Studies on the role of specific dietary fibres in protection against colorectal cancer. Mutat Res. 1996; 350:173–184. PMID:
8657179.
35. Hester CM, Jala VR, Langille MG, Umar S, Greiner KA, Haribabu B. Fecal microbes, short chain fatty acids, and colorectal cancer across racial/ethnic groups. World J Gastroenterol. 2015; 21:2759–2769. PMID:
25759547.
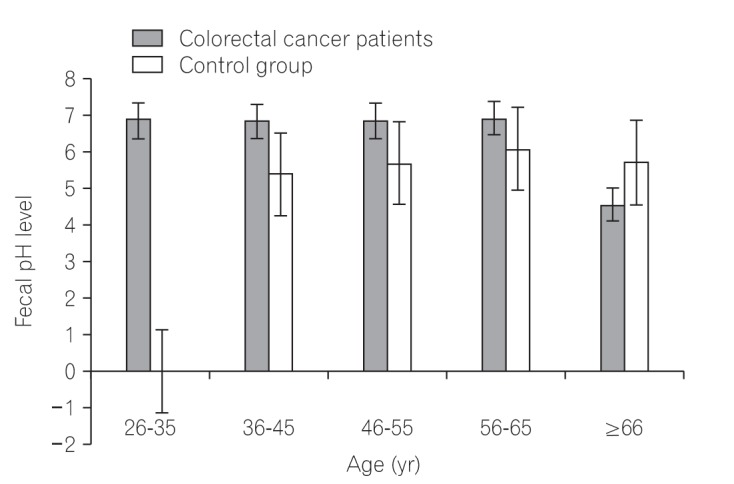
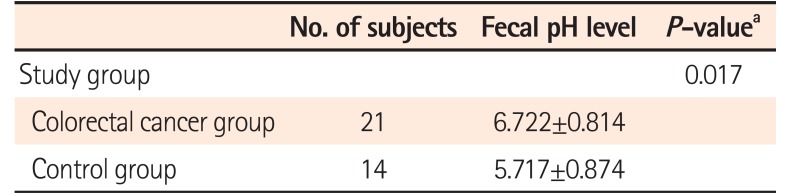
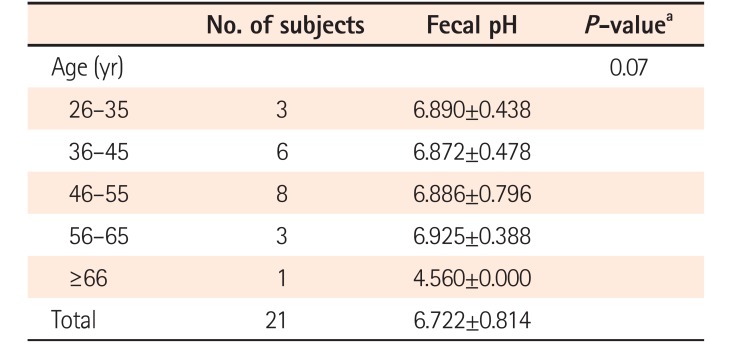
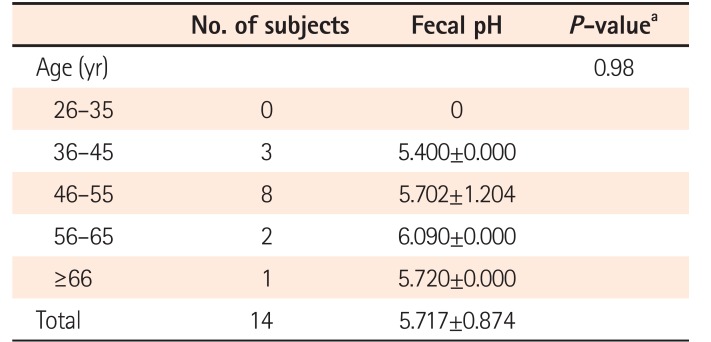
36. Ohigashi S, Sudo K, Kobayashi D, et al. Changes of the intestinal microbiota, short chain fatty acids, and fecal pH in patients with colorectal cancer. Dig Dis Sci. 2013; 58:1717–1726. PMID:
23306850.
37. Donohoe DR, Holley D, Collins LB, et al. A gnotobiotic mouse model demonstrates that dietary fiber protects against colorectal tumorigenesis in a microbiota- and butyrate-dependent manner. Cancer Discov. 2014; 4:1387–1397. PMID:
25266735.

38. Bordonaro M, Lazarova DL, Sartorelli AC. Butyrate and Wnt signaling: a possible solution to the puzzle of dietary fiber and colon cancer risk? Cell Cycle. 2008; 7:1178–1183. PMID:
18418037.

39. Bultman SJ. Molecular pathways: gene-environment interactions regulating dietary fiber induction of proliferation and apoptosis via butyrate for cancer prevention. Clin Cancer Res. 2014; 20:799–803. PMID:
24270685.

40. de Kok TM, van Faassen A, Glinghammar B, et al. Bile acid concentrations, cytotoxicity, and pH of fecal water from patients with colorectal adenomas. Dig Dis Sci. 1999; 44:2218–2225. PMID:
10573365.
41. Walker AR, Walker BF, Walker AJ. Faecal pH, dietary fibre intake, and proneness to colon cancer in four South African populations. Br J Cancer. 1986; 53:489–495. PMID:
3011051.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download