1. Warriner AH, Patkar NM, Curtis JR, Delzell E, Gary L, Kilgore M, et al. Which fractures are most attributable to osteoporosis? J Clin Epidemiol. 2011; 64(1):46–53. PMID:
21130353.

2. Jang HD, Kim EH, Lee JC, Choi SW, Kim K, Shin BJ. Current concepts in the management of osteoporotic vertebral fractures: a narrative review. Asian Spine J. 2020; 14(6):898–909. PMID:
33373513.

3. Umehara T, Inukai A, Kuwahara D, Kaneyashiki R, Kaneguchi A, Tsunematsu M, et al. Physical functions and comorbidity affecting collapse at 4 or more weeks after admission in patients with osteoporotic vertebral fractures: a prospective cohort study. Asian Spine J. 2022; 16(3):419–431. PMID:
33940771.

4. Cho ST, Kim SJ, Nam BJ, Kim KW, Lee GH, Kim JH. Absolute bed rest duration of 3 days for osteoporotic vertebral fractures: a retrospective study. Asian Spine J. 2022; 16(6):898–905. PMID:
35527538.

5. Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, et al. Fracture risk following an osteoporotic fracture. Osteoporos Int. 2004; 15(3):175–179. PMID:
14691617.

6. Kim TY, Jang S, Park CM, Lee A, Lee YK, Kim HY, et al. Trends of incidence, mortality, and future projection of spinal fractures in Korea using nationwide claims data. J Korean Med Sci. 2016; 31(5):801–805. PMID:
27134505.

7. Abrahamsen B, Brask-Lindemann D, Rubin KH, Schwarz P. A review of lifestyle, smoking and other modifiable risk factors for osteoporotic fractures. Bonekey Rep. 2014; 3:574. PMID:
25228987.

8. Lee CY, Back GY, Lee SH. Relationship between type 2 diabetes mellitus and lumbar bone mineral density in postmenopausal women. Asian Spine J. 2021; 15(6):721–727. PMID:
34551503.

9. Lee J, Chang G, Kang H, Ham DW, Lee JS, Jung HS, et al. Impact of bone mineral density on the incidence of age-related vertebral fragility fracture. J Korean Med Sci. 2020; 35(17):e116. PMID:
32356418.

10. Kanis JA, Oden A, Johansson H, Borgström F, Ström O, McCloskey E. FRAX and its applications to clinical practice. Bone. 2009; 44(5):734–743. PMID:
19195497.

11. World Health Organization. WHO Scientific Group on the Assessment of Osteoporosis at Primary Health Care Level. Summary Meeting Report. Geneva, Switzerland: World Health Organization;2004. p. 5–7.
12. Armstrong ME, Spencer EA, Cairns BJ, Banks E, Pirie K, Green J, et al. Body mass index and physical activity in relation to the incidence of hip fracture in postmenopausal women. J Bone Miner Res. 2011; 26(6):1330–1338. PMID:
21611971.

13. Tanaka S, Kuroda T, Saito M, Shiraki M. Overweight/obesity and underweight are both risk factors for osteoporotic fractures at different sites in Japanese postmenopausal women. Osteoporos Int. 2013; 24(1):69–76. PMID:
23229467.

14. Beck TJ, Petit MA, Wu G, LeBoff MS, Cauley JA, Chen Z. Does obesity really make the femur stronger? BMD, geometry, and fracture incidence in the women’s health initiative-observational study. J Bone Miner Res. 2009; 24(8):1369–1379. PMID:
19292617.

15. Cho MJ, Moon SH, Lee JH, Lee JH. Association between osteoporotic vertebral compression fractures and age, bone mineral density, and European quality of life-5 dimensions in korean postmenopausal women: a nationwide cross-sectional observational study. Clin Orthop Surg. 2021; 13(2):207–215. PMID:
34094011.

16. Han S, Park J, Nah S, Jang HD, Han K, Hong JY. Severity of underweight and risk of fracture: a Korean nationwide population-based cohort study. Sci Rep. 2022; 12(1):10153. PMID:
35710927.

17. Han S, Park J, Jang HD, Nah S, Boo J, Han K, et al. Incidence of hip fracture in underweight individuals: a nationwide population-based cohort study in Korea. J Cachex Sarcopenia Muscle;2022.
18. Han S, Park J, Jang HD, Han K, Lee C, Kim W, et al. Changes in underweight status and risk of hip fracture: a Korean nationwide population-based cohort study. J Clin Med. 2022; 11(7):11.

19. Choi EK. Cardiovascular research using the Korean national health information database. Korean Circ J. 2020; 50(9):754–772. PMID:
32725984.

20. World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Geneva, Switzerland: World Health Organization;2000.
21. World Health Organization. Food and Nutrition Surveillance Systems: A Manual for Policy-Makers and Programme Managers. Geneva, Switzerland: World Health Organization;2014.
22. Ahn SH, Park SM, Park SY, Yoo JI, Jung HS, Nho JH, et al. Osteoporosis and osteoporotic fracture fact sheet in Korea. J Bone Metab. 2020; 27(4):281–290. PMID:
33317231.

23. Park SM, Ahn SH, Kim HY, Jang S, Ha YC, Lee YK, et al. Incidence and mortality of subsequent vertebral fractures: analysis of claims data of the Korea National Health Insurance Service from 2007 to 2016. Spine J. 2020; 20(2):225–233. PMID:
31589928.

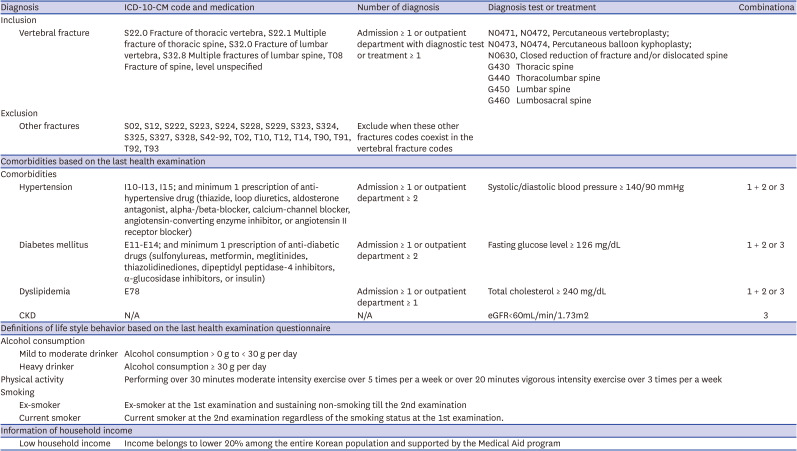
24. Yu MH, Hong N, Lee S, Kim HY, Park HS, Park SM, et al. Operational definition identifying osteoporotic vertebral fractures in the claims database. J Korean Med Sci. 2022; 37(32):e249. PMID:
35971763.

25. Kwon H, Yun JM, Park JH, Cho BL, Han K, Joh HK, et al. Incidence of cardiovascular disease and mortality in underweight individuals. J Cachexia Sarcopenia Muscle. 2021; 12(2):331–338. PMID:
33619889.

26. De Laet C, Kanis JA, Odén A, Johanson H, Johnell O, Delmas P, et al. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005; 16(11):1330–1338. PMID:
15928804.

27. Nevitt MC, Cummings SR, Stone KL, Palermo L, Black DM, Bauer DC, et al. Risk factors for a first-incident radiographic vertebral fracture in women > or = 65 years of age: the study of osteoporotic fractures. J Bone Miner Res. 2005; 20(1):131–140. PMID:
15619679.

28. Xue S, Kemal O, Lu M, Lix LM, Leslie WD, Yang S. Age at attainment of peak bone mineral density and its associated factors: The National Health and Nutrition Examination Survey 2005-2014. Bone. 2020; 131:115163. PMID:
31760214.

29. Coin A, Perissinotto E, Enzi G, Zamboni M, Inelmen EM, Frigo AC, et al. Predictors of low bone mineral density in the elderly: the role of dietary intake, nutritional status and sarcopenia. Eur J Clin Nutr. 2008; 62(6):802–809. PMID:
17637603.

30. Coin A, Sergi G, Benincà P, Lupoli L, Cinti G, Ferrara L, et al. Bone mineral density and body composition in underweight and normal elderly subjects. Osteoporos Int. 2000; 11(12):1043–1050. PMID:
11256896.

31. Sieber CC. Malnutrition and sarcopenia. Aging Clin Exp Res. 2019; 31(6):793–798. PMID:
31148100.

32. Landi F, Liperoti R, Russo A, Giovannini S, Tosato M, Capoluongo E, et al. Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr. 2012; 31(5):652–658. PMID:
22414775.

33. Tokeshi S, Eguchi Y, Suzuki M, Yamanaka H, Tamai H, Orita S, et al. Relationship between skeletal muscle mass, bone mineral density, and trabecular bone score in osteoporotic vertebral compression fractures. Asian Spine J. 2021; 15(3):365–372. PMID:
32872758.

34. Kanis JA, Johansson H, Harvey NC, Gudnason V, Sigurdsson G, Siggeirsdottir K, et al. The effect on subsequent fracture risk of age, sex, and prior fracture site by recency of prior fracture. Osteoporos Int. 2021; 32(8):1547–1555. PMID:
33537845.

35. Park C, Jang S, Jang S, Ha YC, Lee YK, Yoon HK, et al. Identification and validation of osteoporotic hip fracture using the National Health Insurance Database. J Korean Hip Soc. 2010; 22(4):305–311.

36. Lee YK, Park C, Won S, Park JW, Koo KH, Ha YC, Jung HS. Validation of an operational definition to identify distal radius fractures in a National Health Insurance Database. J Hand Surg Am. 2021; 46(11):1026.e1–e7.
37. Curtis JR, Mudano AS, Solomon DH, Xi J, Melton ME, Saag KG. Identification and validation of vertebral compression fractures using administrative claims data. Med Care. 2009; 47(1):69–72. PMID:
19106733.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download