INTRODUCTION
The future hope of the society is children, and the health of children is very important in maintaining the society. Infancy and childhood show the rapid growth and development over a lifetime, and the hearing during this period is very important for the language and the cognitive function development.
12 The interest in infants and children’s health has led to the establishment of a periodic infant and toddler health management system in developed countries. Japan has been conducting infant health checkups since 1969 limited to low-income families, and since 1973 it has been implemented for all infants and toddlers. The checkup period in Japan is 3–4 months, 6–7 months, 18 months, and 3 years old; especially the 18 months and the 3 years examinations are mandatory by the Maternal and Child Health Act.
3 Infant and child checkups in Germany are conducted nine times in preschool period and until a child’s 14th year.
4 The United States Government’s Infant and Toddler Screening is an early and periodic screening, diagnostic and treatment program through the Medicaid for low-income children, and the subjects are children and adolescents from 1 month, 2 months, 4 months, 6 months, 8 months, 12 months, 18 months, and 2 years to 20 years old.
5
Korea has the lowest total fertility rate as 0.92 in 2019 among Organization for Economic Cooperation and Development (OECD) countries due to an aging population and the decrease in the fertile female population, and as a result, the population of infants and toddlers continues to decrease.
6 With an aging Korean society and low birth rate, the Korean government realized the importance of providing an environment which guarantees the healthy birth and the well-being of the infants and children of the nation. Therefore, the Ministry of Health and Welfare and the Korea Centers for Disease Control and Prevention (KCDC) introduced the National Health Screening Program for Infants and Children (NHSPIC) since 2007.
7 This is a children population surveillance program which contains physical examinations and measurements, the screening for visual acuity, and questionnaires regarding anticipatory guidance, developmental issues, and hearing for infants and children in the following age groups: 4 months, 9 months, 18 months, 3 years, 4 years, 5 years, and 6 years old.
The universal hearing screening program for newborns (newborn hearing screening; NHS) was also implemented in October 2018 with the National Health Insurance Service (NHIS) coverage in South Korea. Prior to 2018, the government recognized the significance of NHS and had initiated a nationwide NHS program since 2007, but the programs were primarily for newborns of low-income families. Accordingly, there was no official statistics to identify how many newborns had performed NHS tests in the country before the NHIS coverage, because most caregivers paid the screening tests at their own expenses and test results were shared only between the parents and hospitals. However, as NHSPIC were conducted since 2007 and there are questionnaires asking NHS test results, we could analyze the results of NHS in these periods.
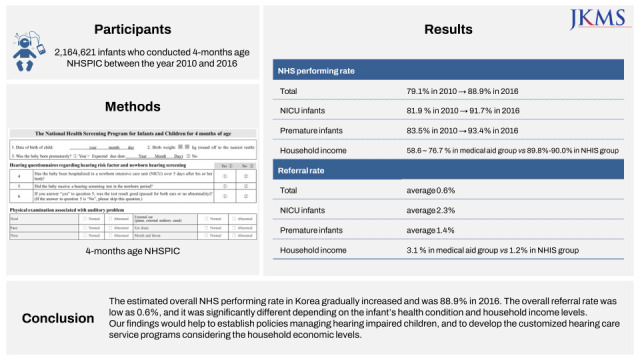
8 Herein, we investigated the results of the hearing questionnaires, physical examination, and the NHS status of infants who participated in the 4-months NHSPIC for 7 years (from 2010 to 2016) in Korea.
METHODS
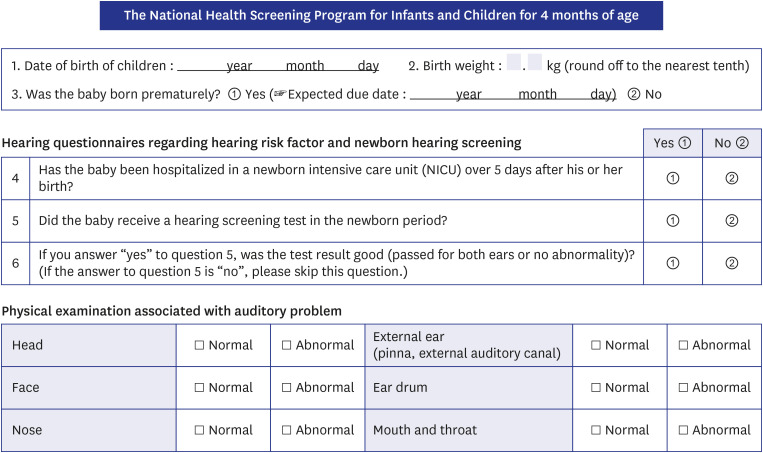
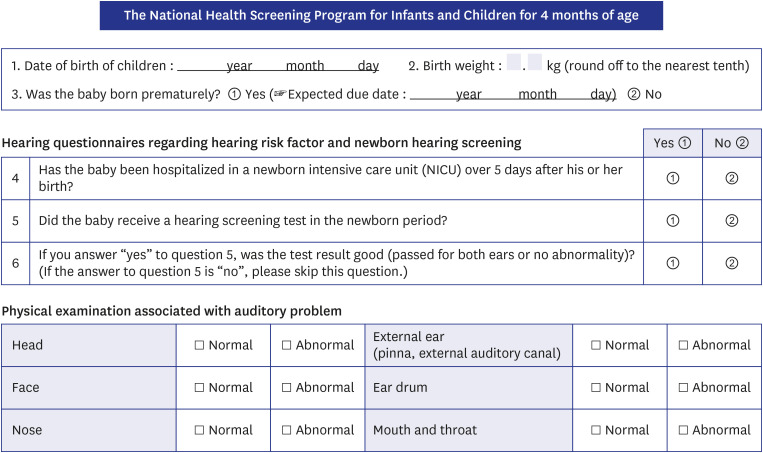
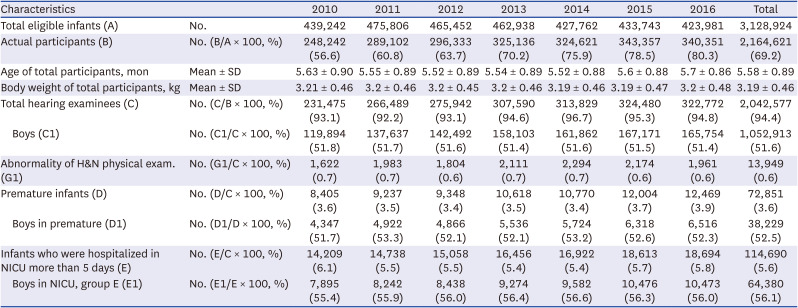
The study used nationwide population data of total 2,164,621 infants who underwent the 4-months NHSPIC from January 2010 to December 2016 using the NHIS information database. The 4-months NHSPIC contains history taking, physical examination and measurement, questionnaires of the anticipatory guidance, developmental issues, visual and hearing states. We collected the results of the date of birth, birth weight, the expected due date for checking premature state, physical examination of head and neck (head, face, nose, external ear, ear drum, and oral cavity) and three hearing questionnaires which inquired whether infant had been hospitalized in the neonatal intensive care unit (NICU) more than 5 days, had performed NHS test and how the result of NHS was (
Fig. 1). The household income classification of this study was based on health insurance premiums: beneficiaries of the Medical Aid program were the lowest grade, and the national health insurance beneficiaries were divided into quintiles (the first quintile means the bottom 20%, and the fifth quintile means the top 20%).
Fig. 1
The National Health Screening Program for Infants and Children of 4 months age regarding hearing questionnaires and physical examination associated with auditory problem in Korea.
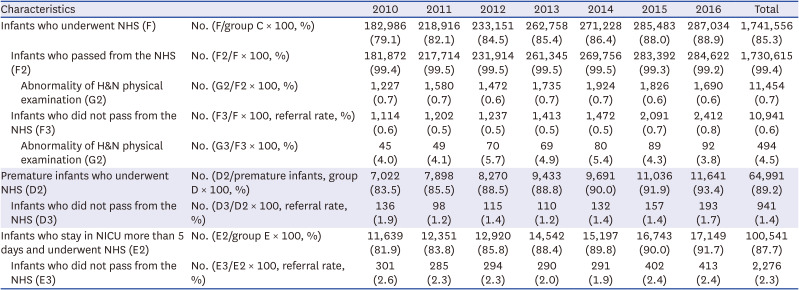
We analyzed the participation rate of the 4-month NHSPIC, the hearing screening rate of NHSPIC, and the abnormality rate of the head and neck examination. We also investigated the NHS performing rates and referral rates according to the total infants, premature infants, infants who were admitted to the NICU for more than 5 days, and the household income levels using the results of the hearing questionnaires in the NHSPIC.
Statistical analysis was performed using SAS software version 9.3 (SAS Institute, Cary, NC, USA). In the results, the continuous variable presented mean and standard deviation, and the categorical variable presented the frequency (%) value. Statistical significance was set to P values < 0.05. The statistical significance was assessed by Pearson χ2 test or Wilcoxon-test.
Ethics statement
This study was performed by the committee of the Korean Society of Otorhinolaryngology-Head and Neck Surgery, and reviewed and confirmed by the Korean Audiological Society. As a representative hospital, the study protocol was approved by the Institutional Review Board (IRB) of Hallym University Kangnam Sacred Heart Hospital (IRB file No. HKS 2016-08-105). The confidentiality of the infants was protected, and their information was anonymized and de-identified before analysis. Thus, informed consent was waived by the IRB because of retrospective database study nature.
DISCUSSION
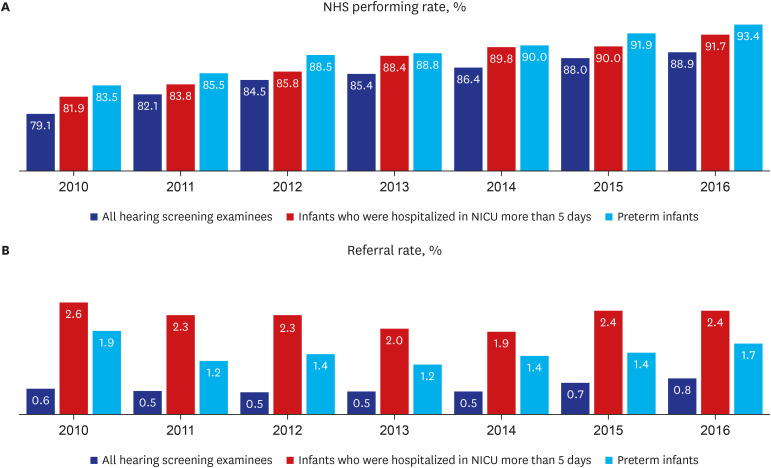
In Korea, the NHSPIC has been conducted since 2007, and it includes the preventive education for the health promotion of infants and children from birth through six years old. In the 4-months NHSPIC, there are hearing checkups by questionnaires which are meaningful in that they remind the importance of the hearing screening in the newborn period and the regular hearing checkups for infants who have risk factors for hearing loss. As for the NHS, there was a government-funded support for low-income class families prior to October 2018, but the NHS test was not yet supported to all the households as a national health insurance, therefore the parents themselves decided to perform the screening test and paid for it. However, the government-funded NHS pilot project which has been conducted from 2007 had helped to improve the national awareness of the NHS. As a result, the NHS performing rate had increased as the NHSPIC’s examination year went on; the NHS performing rate of the infants who participated in the 4-month NHSPIC was 79.1% in 2010, but it rose to 88.9% in 2016. In our study, the NHS performing rates in premature infants and in infants who were hospitalized for more than 5 days in NICU were higher than that of the overall infants. It is possible that due to the severity and the long hospitalization period in these infant groups compared to healthy newborns, there might have been sufficient time to inform parents and conduct the NHS test. But further studies are needed to find out more detailed causes.
In the present study, the overall average referral rates were 0.5% to 0.8%. Considering that the ideal referral rate suggested by the Joint Committee on Infant Hearing (JCIH) and various NHS guidelines is 1% to 4%,
91011 our overall referral rate was relatively low. The low referral rates of the NHS tests in Korea were also seen in the results of government-supported NHS pilot projects, and it is presumed to be due to the behavior of some screeners’ repeating the NHS tests more than three times.
12 According to the informal survey performed by the Ministry of Health and Welfare in 2010, it is reported that the maternity clinics which comprise 91.4% of hearing screening institution in Korea,
1213 had misconceptions in the beginning of the NHS program, misunderstood the screening tests for a confirmation test and performed the screening tests more than three times repeatedly. The manner of repeating the screening test for multiple times has a problem in that it lowers the referral and leads to false negative. The JCIH recommends that the screening test should be performed maximum twice, as it is possible to accidentally achieve a “pass” result when repeating the automated screening test.
91415 Subsequently, the Otolaryngology Society established annual off-line NHS workshops, an online NHS training site development (2013) and the publication of NHS guidelines and position statement (2010 and 2018) to increase the investigator proficiency.
11
The referral rates for premature infants and the infants admitted to the NICU for more than 5 days were 1.4% (1.2–1.9%) and 2.3% (1.9–2.6%) respectively, which is higher than the overall mean referral rate (0.5–0.8%). It is in accordance with other reported referral rates of NICU neonates which are 2.8–9.2% and much higher than overall referral rate.
1316171819 It is noted that the referral rate increases with raised incident of hearing loss and that NICU neonates show a high incidence of hearing loss, at a rate 10 times greater than that of well-babies.
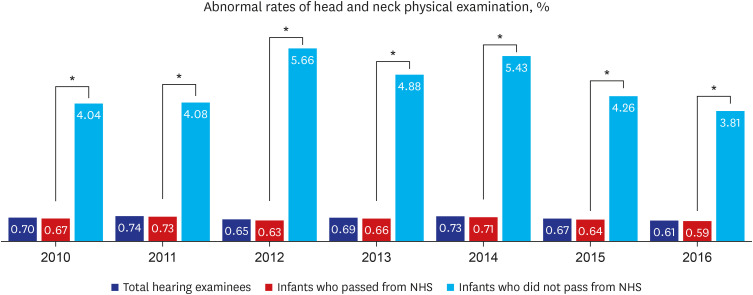
1320 In this study, the total infants were divided into the ‘pass group’ and the ‘refer group,’ and the proportion of head and neck abnormalities in the physical examination were analyzed. We identified that the head and neck abnormalities were statistically significantly higher in the ‘refer group’ than in the ‘pass group.’ External ear anomalies such as pre-auricular pit, lob ear, microtia or congenital atresia might occur with middle ear or inner ear anomalies. Congenital atresia is reported to have 12% of abnormal inner ear findings in radiologic examination.
2122 Cleft lip and cleft palate is commonly associated with otitis media with effusion and conductive hearing loss. Since head and neck anomalies have a tendency to accompany conductive hearing loss, sensorineural hearing loss or mixed hearing loss, it can be advised to the parents to have continuous hearing check-up when neonates have head and neck anomalies.
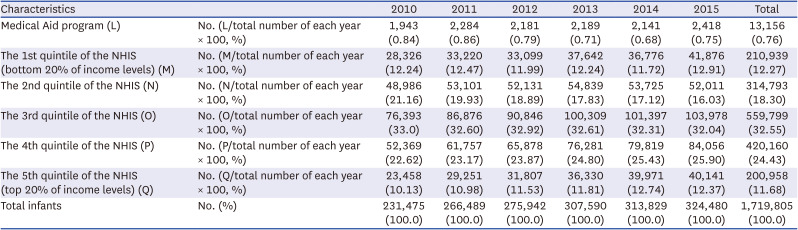
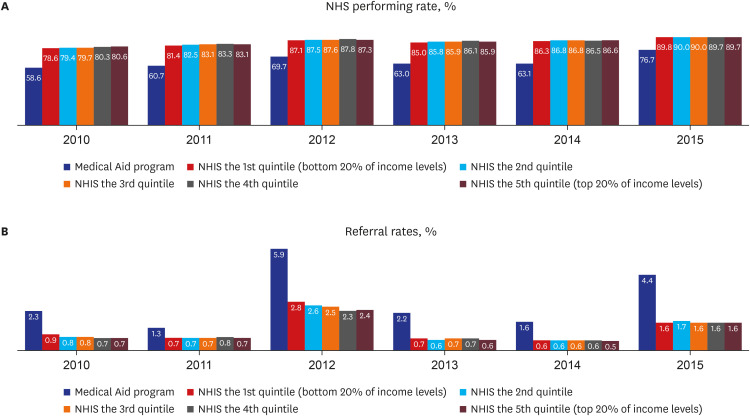
In the present study, the classification of income level was divided into a total of six groups, which were the Medical Aid group and five health insurance groups based on the health insurance premiums. The proportion of newborns and infants was not evenly distributed according to their classification. The Medical Aid group had the lowest percentage of infants (0.76%), and the health insurance groups had the highest percentage of infants in the order of 3rd (32.55%), 4th (24.43%), 2nd (18.30%), 1st (12.27%), and 5th (11.68%) quintile (the first quintile means the bottom 20%, and the fifth quintile the top 20%). Since the ratio of infants are not evenly distributed according to the household income levels as in our study (the 3rd quintile had the highest rate of infants as 32.6%), the governmental policy to support the target group should consider the actual rate of infants in the households. For example, if there is a policy to support up to the 3rd quartile of income level according to the health insurance from bottom, a budget to cover 64% of all infants should be prepared. However, if the policy was applied to the lower 2nd quintile, the budget to support 31% of all infants is required.
In this study, the NHS performing rates and referral rates were significantly different depending on the household income level. The Medical Aid group had a significantly lower NHS performing rate and the higher referral rate than the health insurance groups. Considering that government-funded NHS low-income household supporting NHS programs were going on during these periods, it can be assumed that the newborns or infants of the Medical Aid group still had difficulties visiting hospitals due to lack of time, or awareness about the NHS program. Currently (after the year 2018), the NHS test is covered by national health insurance up to two times, so there are no needs to pay for the test by the parents, which means that the economic burden for the hearing screening tests is reduced. In the future, further studies are needed to investigate the NHS performing rate according to the income level, the place of household residence and the screening institutions. Additional research is also needed to examine the reasons for the higher referral rate 3.1% (1.3–5.9%) of the Medical Aid group compared to the health insurance group 1.2%.
There are some limitations to the present study. First, it does not directly analyze the data of NHS but indirectly evaluate the data based on the questionnaires of NHSPIC for 4-months infants. That is, there might be dropouts (infants participated in NHS but have not participated in NHSPIC at-4 months of age) or a recall bias (NHS results are dependent on parents’ memories). Second, although we identified that the performing rates were low and the referral rates were high in infants enrolled in Medical Aid programs, we could not recognize the causes in this study. We need to examine the regional distribution of families enrolled in Medical Aid programs, and to inspect the parental awareness of NHS among these families in the future.
To our knowledge, this is the first study to report the results of NHS in total neonates before it was covered by the national insurance and became UNHS in Korea. Since approximately 80% of the total eligible infants participated in the 4-months NHSPIC in 2016, it is assumed that this data represents the overall NHS result in Korea. The estimated overall NHS performing rate was 88.9%, the overall referral rate was 0.6%, and it was significantly different depending on the infant’s health condition and household income levels. We assume that our finding would help to establish policies managing hearing impaired children, and to develop the customized hearing care service programs considering the household economic levels.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download