Abstract
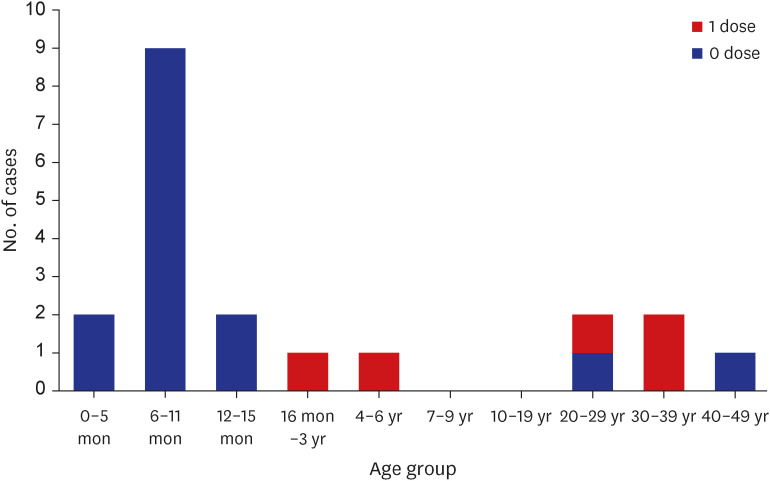
A measles outbreak with 20 confirmed cases occurred at a local children’s hospital in Daejeon from March 28 to April 21, 2019. The index patient was a 7-month-old girl with a recent history of travel to Vietnam. Contact tracing, active surveillance, and post-exposure prophylaxis were conducted by health authorities. Among the 20 patients, 11 (55%) were infants (0–11 months of age), three (15%) were aged 1–3 years, one (5%) was aged 4 years, and five (25%) were adults. Fifteen (75%) patients did not have a history of measles vaccination, and five (25%) had received only one vaccine dose. This study described the importance of prompt application of infection control measures in susceptible environments, including hospitals. Age-appropriate vaccination and providing information on infectious diseases to international travelers and multicultural families in Korea is vital.
Graphical Abstract
Measles is a highly contagious disease with classic symptoms including fever, cough, coryza, and conjunctivitis, followed by maculopapular rash. Although a safe and effective vaccine has been available, measles still causes considerable morbidity and mortality in the world.1 In particular, a resurgence of measles occurred in 2019 that was driven by multiple potential factors, including conflict, poor health education, lack of access to medical care, complacency, and increased vaccine hesitancy.2 Since 2020, the coronavirus disease 2019 (COVID-19) pandemic has seriously affected vaccination programs, raising concerns about further resurgences of measles as pandemic control measures are relaxed.1
The Republic of Korea declared measles eliminated in 2006, and it was verified as measles-free by the World Health Organization Western Pacific Region Office in 2014.3 However, individual imported cases and small outbreaks of measles have continued to occur. In 2019, measles outbreaks were documented in various regions, such as Daegu, Gyeonggi-do, Incheon, Gyeongsangbuk-do, Daejeon, Seoul, and Jeollanam-do.4
Among them was an outbreak in Daejeon in a local children’s hospital, a high-risk environment containing infants and young children that are susceptible to measles. The outbreak occurred from March 28 to April 21, 2019 and had 20 confirmed cases. The hospital where the measles outbreak occurred was a pediatric hospital for patients in Daejeon, Sejong and areas of Chungcheongnam-do. The facility used a single building, with inpatient wards on three floors (floors 4–6) with 66 beds in 42 rooms (33 single-patient rooms, three 3-bed rooms, and six 4-bed rooms). There was no negative pressure room. The children were hospitalized with their guardians and could change rooms during hospitalization. Additionally, each floor contained a lounge, allowing for contact among patients and caregivers from different rooms.
An outbreak response was carried out by the Public Health and Welfare Bureau of Daejeon City with recommendations from the Korea Centers for Disease Control and Prevention (KCDC). Contact tracing, active surveillance, prompt post-exposure prophylaxis, and public announcements via the press were conducted. Diagnosis of measles was performed according to KCDC guideline, with laboratory confirmation in suspected cases. Measles was suspected in any person with clinical symptoms (i.e., fever, rash, cough, coryza, conjunctivitis) or epidemiological links. Additionally, laboratory confirmation by detection of viral RNA by reverse transcriptase-polymerase chain reaction, detection of specific immunoglobulin (Ig) M, a four-fold increase in IgG antibody concentration in paired acute and convalescent serum specimens, or isolation of the virus in cell culture was performed.56 In confirmed cases, demographic characteristics, epidemiologic data, and clinical manifestations were documented. Immunization status was confirmed using medical records, including the National Immunization Registry, and descriptive analyses were performed. Vaccine-associated measles was excluded if the rash occurred within 56 days after vaccination and was genotype A, according to the KCDC guideline.5
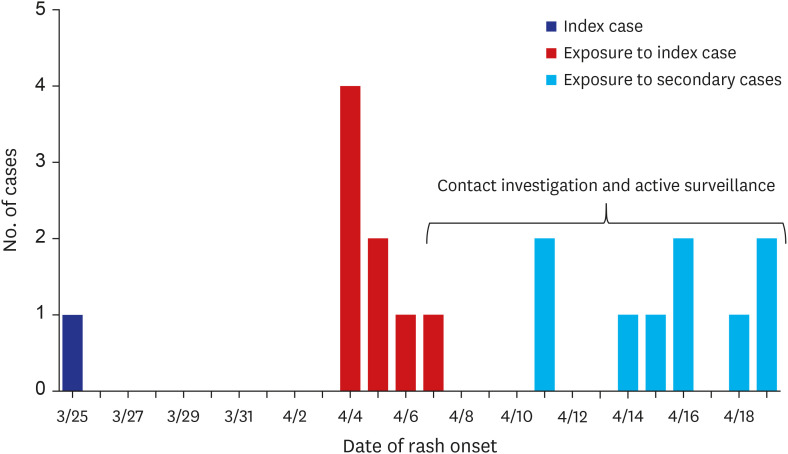
The index patient was a 7-month-old girl who was initially admitted on March 23, 2019 with suspected pneumonia due to fever, cough, and rhinorrhea. A rash developed on March 25, and she was subsequently transferred to a university hospital on March 27 for continued fever and rash. The patient was diagnosed with measles on March 28. Before the onset of symptoms, she had traveled to her mother’s home country of Vietnam and had not been vaccinated against measles.
Four secondary cases were reported from April 4–6, all of which had had contact with the index patient in the hospital between March 23 and 27. On April 7, outbreak control was initiated by the health department. A measles-containing vaccine (measles-mumps-rubella, MMR) was recommended for susceptible contacts aged ≥ 6 months, and Igs were administered to infants aged < 6 months within six days of exposure.56 Contacts with symptoms, such as fever or rash, were instructed to visit screening centers for laboratory examination and treatment. One dose of MMR vaccination for infants aged 6–11 months and a catch-up MMR vaccination for children aged ≥ 12 months were recommended in Daejeon by the KCDC.
From April 8–12, eight additional cases were reported, all of which had also had contact with the index patient in the hospital between March 23 and 27. Moreover, from April 15–21, seven cases, which had been exposed to the secondary cases, were confirmed. On May 13, monitoring of the contacts was completed as no additional cases during the 21-day incubation period were documented. Health authorities actively monitored a total of 2,286 contacts in Daejeon, Sejong, and Chungcheongnam-do (Fig. 1).
A total of 20 cases of measles among infants, children, guardians, and healthcare workers were diagnosed during the outbreak. Of these, 11 (55%) were infants (aged 0–11 months), three (15%) were aged 1–3 years, one (5%) was aged 4 years, and five (25%) were adults. All 15 infants and children had a history of hospitalization. Among the five adults, four were guardians and one was a nursing student. Fifteen (75%) patients did not have a history of measles vaccination, and five (25%) patients only had one vaccine dose (Fig. 2).
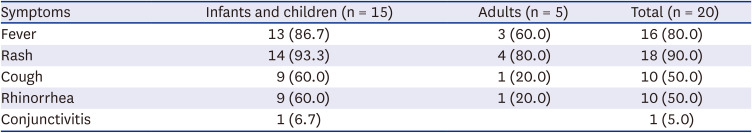
Among the 20 cases, rash (n = 18, 90%) and fever (n = 16, 80%) were the most common symptoms. Cough and rhinorrhea were present in 10 (50%) cases, and only one case of conjunctivitis was reported. Infants and children showed more symptoms compared with adults (Table 1). Excluding the index patient, five of the 19 patients, aged 5, 6, 9, 13 months, and 4 years, were hospitalized at the Chungnam National University Hospital. Fever persisted for seven (range: 6–10) days in the hospitalized patients. Additionally, four patients had otitis media, and two had concomitant pneumonia. Three patients were co-infected with influenza B virus, metapneumovirus and rhinovirus, and norovirus, respectively. All patients fully recovered after treatment.
The 2019 measles outbreak in Daejeon highlighted the characteristics of an outbreak occurring due to an imported case and in a local children’s hospital. Due to the particular location, 75% of the cases were infants and children. As infants and young children are known to be at high risk of measles,6 six patients with long-lasting fever and complications such as pneumonia and otitis media required admission to a university hospital. In addition, co-infections were noted along with measles infections, which may have led to confusion in diagnoses and exacerbations in conditions. As children are vulnerable to various infectious diseases, including measles, a policy of preemptive isolation in hospital settings, even with an unknown source, is vital in preventing the spread.
The initial clinical presentation of measles is similar to that of common respiratory viral infections. With the elimination of measles in Korea, fewer opportunities exist for young healthcare workers to get familiar with measles. Foreign importations of measles can occur at any time, with the clustering of susceptible individuals potentially causing outbreaks. Therefore, clinicians should be alert to pertinent symptoms and obtain a detailed medical history, including travel history.
In this outbreak, 75% of the cases had not received a measles vaccine, although most of them were aged < 12 months. In Korea, the first dose of MMR vaccination is recommended at 12–15 months of age, and the second dose is recommended at school entry, at 4–6 years of age.5 However, in this outbreak, all six patients aged ≥ 4 years including the nursing student, had not received two doses of MMR vaccination. In a 2014 study, a progressive decline in measles seropositivity was observed after vaccination in infancy, adolescence, and young adulthood. In the absence of natural boosting by wild viruses, measles susceptibility may be increasing in Korea.7 Therefore, the importance of having immunity to measles including completing age-appropriate vaccinations should be emphasized.
Infants aged 6–11 months are recommended to be vaccinated when traveling to areas where measles is endemic.5 However, the index patient in this outbreak had not been vaccinated for measles, despite traveling to Vietnam. According to the Korean National Tourism Survey 2019, international travel has gradually increased, particularly to Vietnam and the Philippines, where measles is prevalent.8 In addition, the number of international marriages had increased before COVID-19, and the proportion of births from international marriages among domestic births increased, to 6% in 2021.9 Multicultural families tend to visit their home countries, and children are more likely to travel abroad with their parents. International travel has temporarily decreased due to the pandemic, but may increase again as social activities restart. Pre-travel consultations for international travelers as well as support for multicultural families that include information on travel-related infectious diseases and immunizations are vital. In the 2014 measles seroprevalence study, the overall seropositivity was 71.5% and the lowest was detected in adolescents and young adults (1990–2001 birth year group).7 As susceptibility to measles was increasing in adolescents and young adults in Korea, counseling on this aspect is important.
This study presented a measles outbreak that occurred in a local children’s hospital in a measles-free country. We described the clinical presentations, the importance of preemptive isolation of infectious diseases such as measles, and the prompt application of infection control measures in hospitals. Information on infectious diseases and preventive measures should be provided to the increasing number of international travelers and multicultural families in Korea.
ACKNOWLEDGMENTS
The authors thank the Public Health and Welfare Bureau of Daejeon City and the Infection Control Department at Chungnam National University Hospital for their great work in outbreak control.
Notes
Author Contributions:
Conceptualization: Cho EY.
Data curation: So H, Cho EY.
Formal analysis: So H, Cho EY.
Investigation: So H, Kim KM, Bae EY, Cho EY.
Methodology: So H, Kim KM, Bae EY, Cho EY.
Software: Cho EY.
Validation: Cho EY.
Visualization: Bae EY, Cho EY.
Writing - original draft: So H.
Writing - review & editing: Kim KM, Cho EY.
References
1. Hübschen JM, Gouandjika-Vasilache I, Dina J. Measles. Lancet. 2022; 399(10325):678–690. PMID: 35093206.
2. Cousins S. Measles: a global resurgence. Lancet Infect Dis. 2019; 19(4):362–363. PMID: 31002077.
3. Choe YJ, Jee Y, Oh MD, Lee JK. Measles elimination activities in the Western Pacific Region: experience from the Republic of Korea. J Korean Med Sci. 2015; 30(Suppl 2):Suppl 2. S115–S121. PMID: 26617443.
4. Choi S, Cho EH. Analysis of the occurrence of measles in Korea, 2019. Public Health Wkly Rep. 2020; 13:2445–2458.
5. Korea Centers for Disease Control and Prevention (KCDC). Guidelines for Measles Outbreak Investigation and Response. Osong, Korea: KCDC;2019.
6. American Academy of Pediatrics. Measles. Kimberlin DW, Barnett ED, Lynfield R, Sawyer MH, editors. Red Book: 2021 Report of the Committee on Infectious Diseases. Itasca, IL, USA: American Academy of Pediatrics;2021. p. 503–519.
7. Kang HJ, Han YW, Kim SJ, Kim YJ, Kim AR, Kim JA, et al. An increasing, potentially measles-susceptible population over time after vaccination in Korea. Vaccine. 2017; 35(33):4126–4132. PMID: 28669617.
8. Korea Ministry of Culture Sports and Tourism. Korea National Tourism Survey, 2019. Sejong, Korea: Korea Ministry of Culture Sports and Tourism;2020. p. 170–172.
9. Statistics Korea. Multicultural Population Dynamics in 2020. Daejeon, Korea: Statistics Korea;2021.
Fig. 1
Outbreak of measles in a local children’s hospital in Daejeon, Korea, 2019. Cases without rash (n = 2) are not included in this figure.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download