1. Kosyluk KA, Conner KO, Al-Khouja M, Bink A, Buchholz B, Ellefson S, et al. Factors predicting help seeking for mental illness among college students. J Ment Health. 2021; 30(3):300–307. PMID:
32191145.
2. Cornally N, McCarthy G. Help-seeking behaviour for the treatment of chronic pain. Br J Community Nurs. 2011; 16(2):90–98. PMID:
21378675.
3. Substance Abuse and Mental Health Services Administration. National Mental Health Services Survey (N-MHSS). Rockville, MD, USA: Substance Abuse and Mental Health Services Administration;2020.
4. National Center for Mental Health. The National Survey on Mental Health Knowledge and Attitude. Seoul, Korea: National Center for Mental Health;2021.
5. Murthy RS. National mental health survey of India 2015–2016. Indian J Psychiatry. 2017; 59(1):21. PMID:
28529357.
8. Noh SJ, Yoon Y. Analyzing online news media coverage of depression. Korean J Commun Inf. 2013; 61(1):5–27.
9. Pescosolido BA, Martin JK, Long JS, Medina TR, Phelan JC, Link BG. “A disease like any other”? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. Am J Psychiatry. 2010; 167(11):1321–1330. PMID:
20843872.
10. Maulik PK, Devarapalli S, Kallakuri S, Tewari A, Chilappagari S, Koschorke M, et al. Evaluation of an anti-stigma campaign related to common mental disorders in rural India: a mixed methods approach. Psychol Med. 2017; 47(3):565–575. PMID:
27804895.
11. Harré JR. The role of biological and genetic causal beliefs in the stigmatisation of mental patients. J Ment Health. 2001; 10(2):223–235.
12. Cohen CI. The biomedicalization of psychiatry: a critical overview. Community Ment Health J. 1993; 29(6):509–521. PMID:
8275674.
13. Conrad P. The Medicalization of Society: on the Transformation of Human Conditions Into Treatable Disorders. Baltimore, MD, USA: Johns Hopkins University Press;2007.
14. Han DY, Chen SH. Reducing the stigma of depression through neurobiology-based psychoeducation: a randomized controlled trial. Psychiatry Clin Neurosci. 2014; 68(9):666–673. PMID:
24521323.
15. Cheng ZH. Asian Americans and European Americans’ stigma levels in response to biological and social explanations of depression. Soc Psychiatry Psychiatr Epidemiol. 2015; 50(5):767–776. PMID:
25539590.
16. Zafar SN, Syed R, Tehseen S, Gowani SA, Waqar S, Zubair A, et al. Perceptions about the cause of schizophrenia and the subsequent help seeking behavior in a Pakistani population - results of a cross-sectional survey. BMC Psychiatry. 2008; 8(1):56. PMID:
18637176.
17. Wrigley S, Jackson H, Judd F, Komiti A. Role of stigma and attitudes toward help-seeking from a general practitioner for mental health problems in a rural town. Aust N Z J Psychiatry. 2005; 39(6):514–521. PMID:
15943655.
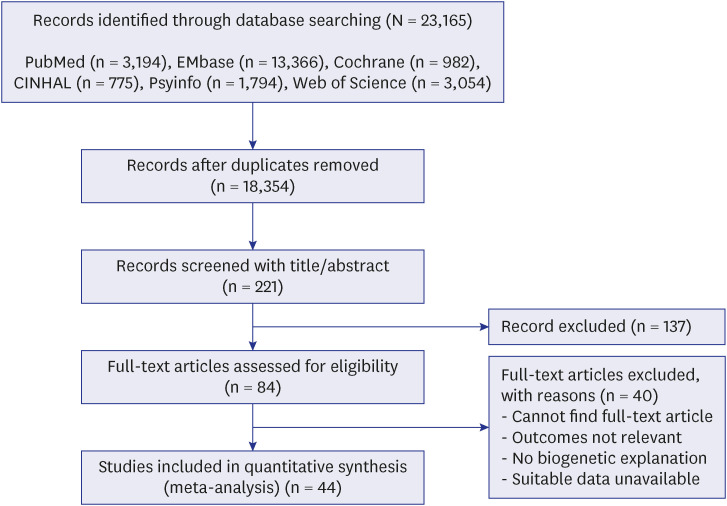
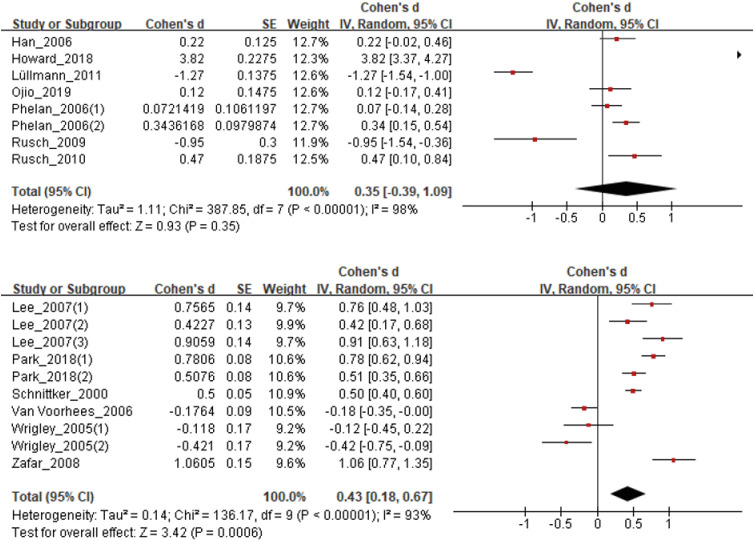
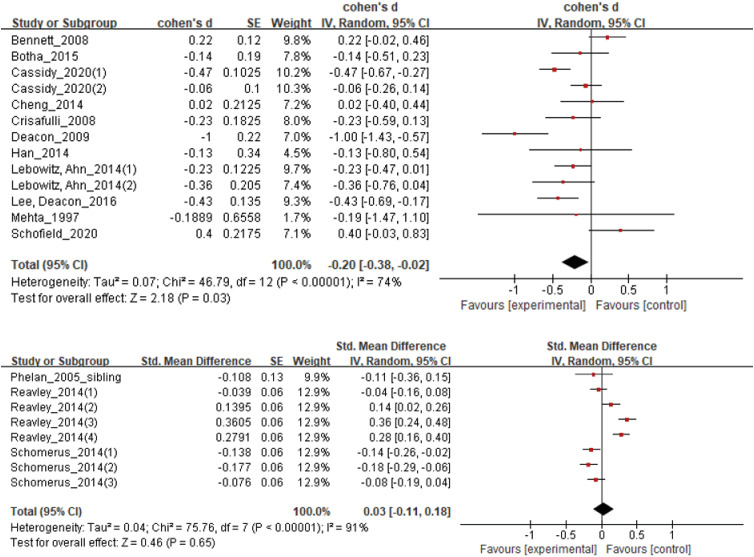
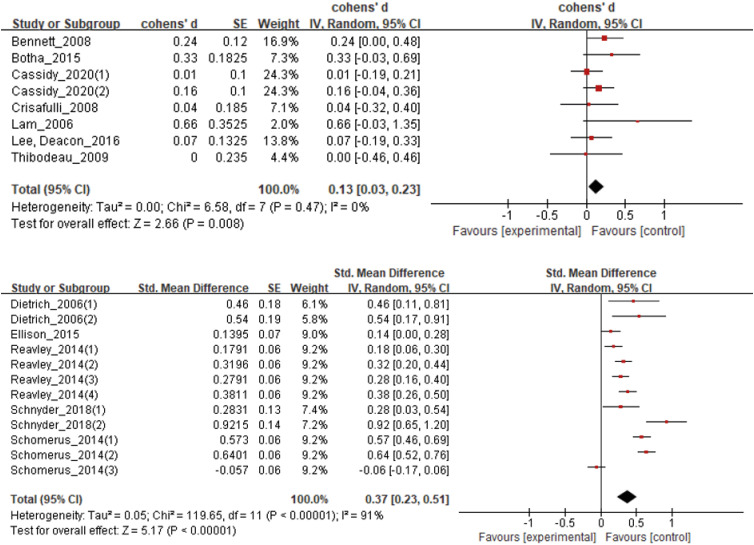
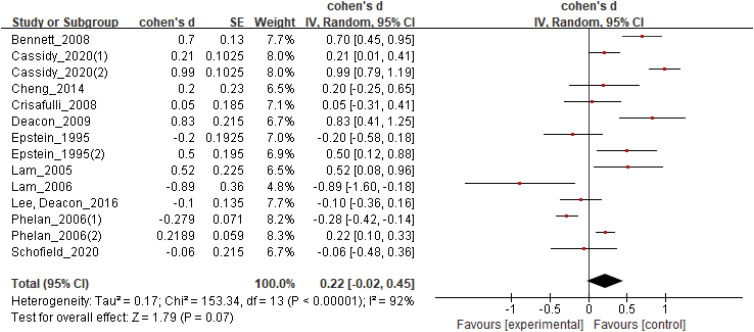
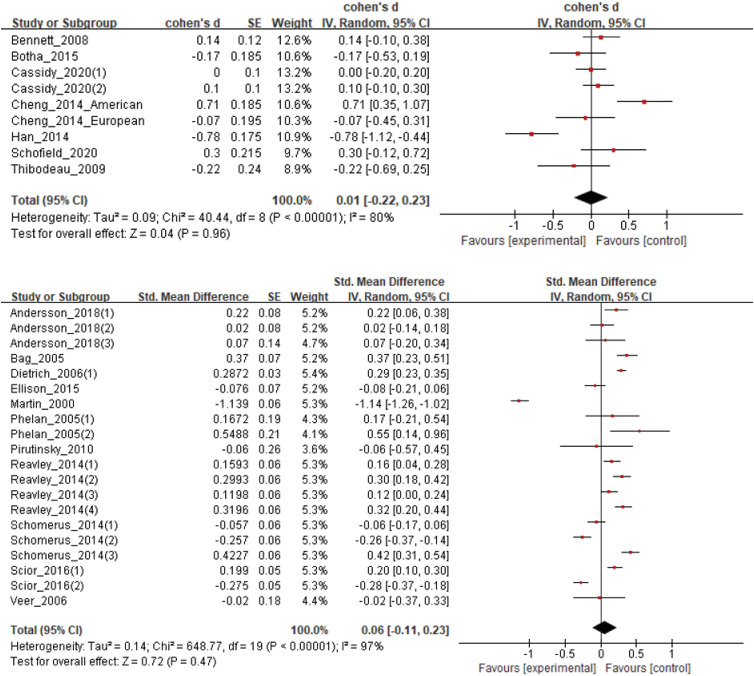
18. Kvaale EP, Gottdiener WH, Haslam N. Biogenetic explanations and stigma: a meta-analytic review of associations among laypeople. Soc Sci Med. 2013; 96(96):95–103. PMID:
24034956.
19. Kvaale EP, Haslam N, Gottdiener WH. The ‘side effects’ of medicalization: a meta-analytic review of how biogenetic explanations affect stigma. Clin Psychol Rev. 2013; 33(6):782–794. PMID:
23831861.
20. Loughman A, Haslam N. Neuroscientific explanations and the stigma of mental disorder: a meta-analytic study. Cogn Res Princ Implic. 2018; 3(1):43. PMID:
30426319.
21. Bennett L, Thirlaway K, Murray AJ. The stigmatising implications of presenting schizophrenia as a genetic disease. J Genet Couns. 2008; 17(6):550–559. PMID:
18773286.
22. Botha FB, Dozois DJA. The influence of emphasizing psychological causes of depression on public stigma. Can J Behav Sci. 2015; 47(4):313–320.
23. Lam DC, Salkovskis PM. An experimental investigation of the impact of biological and psychological causal explanations on anxious and depressed patients’ perception of a person with panic disorder. Behav Res Ther. 2007; 45(2):405–411. PMID:
16684503.
24. Krendl AC, Pescosolido BA. Countries and cultural differences in the stigma of mental illness: the east–west divide. J Cross Cult Psychol. 2020; 51(2):149–167.
25. Haslam N. Genetic essentialism, neuroessentialism, and stigma: commentary on Dar-Nimrod and Heine (2011). Psychol Bull. 2011; 137(5):819–824. PMID:
21859181.
26. Schnyder N, Panczak R, Groth N, Schultze-Lutter F. Association between mental health-related stigma and active help-seeking: systematic review and meta-analysis. Br J Psychiatry. 2017; 210(4):261–268. PMID:
28153928.
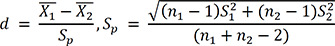
27. Cho JH. Theory and practice of meta-analysis. J Rhinol. 2020; 27(2):83–89.
28. Hwang SD. Meta-Analysis: From Forest Plot to Network Meta-Analysis. Seoul, Korea: Hannarae Publishing Co.;2018.
29. Jang Y, Chiriboga DA, Okazaki S. Attitudes toward mental health services: age-group differences in Korean American adults. Aging Ment Health. 2009; 13(1):127–134. PMID:
19197698.
30. Pang S, Liu J, Mahesh M, Chua BY, Shahwan S, Lee SP, et al. Stigma among Singaporean youth: a cross-sectional study on adolescent attitudes towards serious mental illness and social tolerance in a multiethnic population. BMJ Open. 2017; 7(10):e016432.
31. Bonabi H, Müller M, Ajdacic-Gross V, Eisele J, Rodgers S, Seifritz E, et al. Mental health literacy, attitudes to help seeking, and perceived need as predictors of mental health service use: a longitudinal study. J Nerv Ment Dis. 2016; 204(4):321–324. PMID:
27015396.
32. Barker G, Olukoya A, Aggleton P. Young people, social support and help-seeking. Int J Adolesc Med Health. 2005; 17(4):315–335. PMID:
16445071.
33. Abdullah T, Brown TL. Mental illness stigma and ethnocultural beliefs, values, and norms: an integrative review. Clin Psychol Rev. 2011; 31(6):934–948. PMID:
21683671.
34. Park JE, Cho SJ, Lee JY, Sohn JH, Seong SJ, Suk HW, et al. Impact of stigma on use of mental health services by elderly Koreans. Soc Psychiatry Psychiatr Epidemiol. 2015; 50(5):757–766. PMID:
25491446.
35. Weiner B, Perry RP, Magnusson J. An attributional analysis of reactions to stigmas. J Pers Soc Psychol. 1988; 55(5):738–748. PMID:
2974883.
36. Weiner BJ. Searching for order in social motivation. Psychol Inq. 1996; 7(3):199–216.
37. Corrigan PW, Shapiro JR. Measuring the impact of programs that challenge the public stigma of mental illness. Clin Psychol Rev. 2010; 30(8):907–922. PMID:
20674114.
38. Read J, Law A. The relationship of causal beliefs and contact with users of mental health services to attitudes to the ‘mentally ill’. Int J Soc Psychiatry. 1999; 45(3):216–229. PMID:
10576088.
39. Walker I, Read J. The differential effectiveness of psychosocial and biogenetic causal explanations in reducing negative attitudes toward “mental illness”. Psychiatry. 2002; 65(4):313–325. PMID:
12530335.
40. Lebowitz MS, Ahn WK. Effects of biological explanations for mental disorders on clinicians’ empathy. Proc Natl Acad Sci U S A. 2014; 111(50):17786–17790. PMID:
25453068.





 PDF
PDF Citation
Citation Print
Print



 .
. .
. ,
,
 XML Download
XML Download