Coronavirus disease 2019 (COVID-19) is usually a mild or self-limited illness, but severe clinical manifestations, including croup, pneumonia, neurologic manifestations, myocarditis, and death, can rarely occur in children.
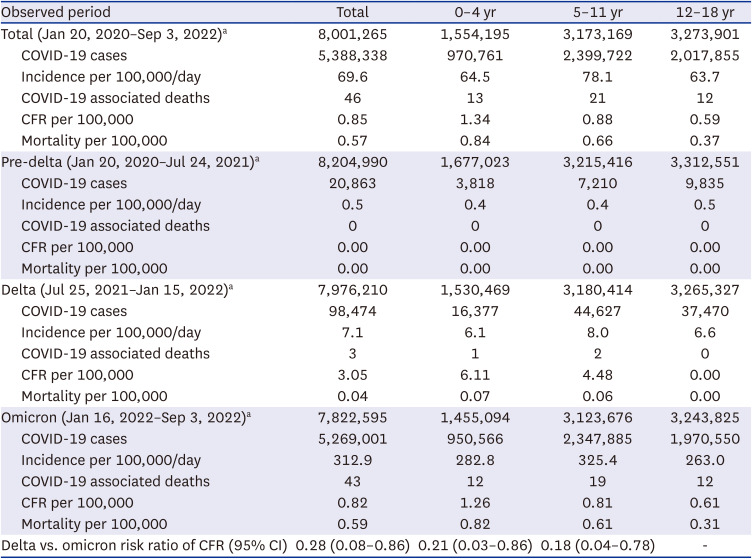
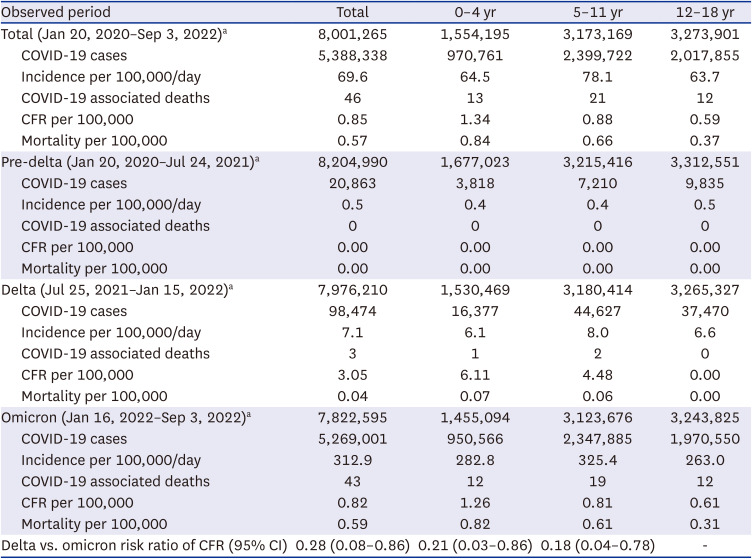
12 As of September 3, 2022, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus has resulted a 5,388,338 cases and 46 deaths in children and adolescents aged 18 year or younger in the Republic of Korea.
3
Although fatal outcomes of SARS-CoV-2 infection are rarely reported in children, clinical analysis of fatal cases and assessment of the risk factors for COVID-19-associated mortality in children is important to define critical cases for which early, aggressive treatment is needed and to help inform target groups for vaccination policy. During early 2022, the Korea Disease Control and Prevention Agency (KDCA) noted an increase in the number of COVID-19 associated deaths in children. In this report, we describe COVID-19 associated pediatric mortality from 2020 to 2022, in aim to provide evidence to strengthen public health policies for children.
Since the beginning of the COVID-19 pandemic, all fatal cases have been reported to the KDCA and are subject of epidemiologic investigation by the Central Disease Control Headquarters. COVID-19 associated death was defined as cases with no alternative cause of death and one of the following criteria; 1) death occurred in confirmed COVID-19 cases during the quarantine period, 2) COVID-19 confirmed after death or 3) cases confirmed by medical personnel as to related to COVID-19 even after quarantine period. This report describes clinical manifestation of the COVID-19 associated fatal cases ≤ 18 years of age.
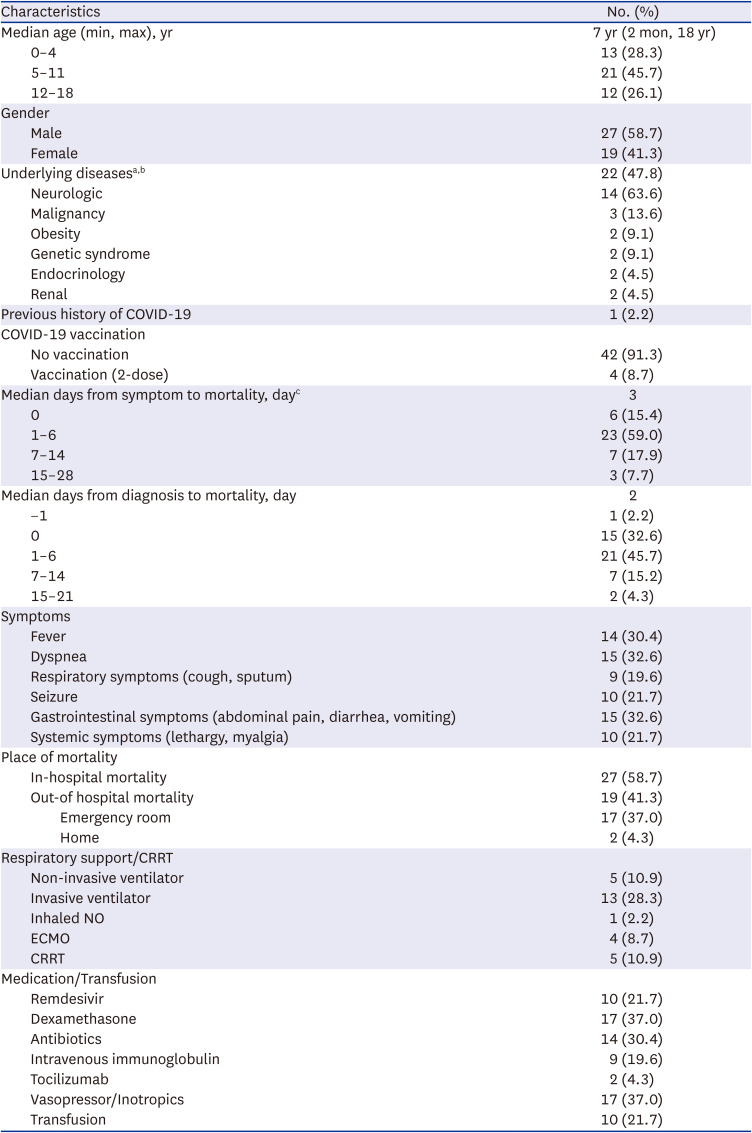
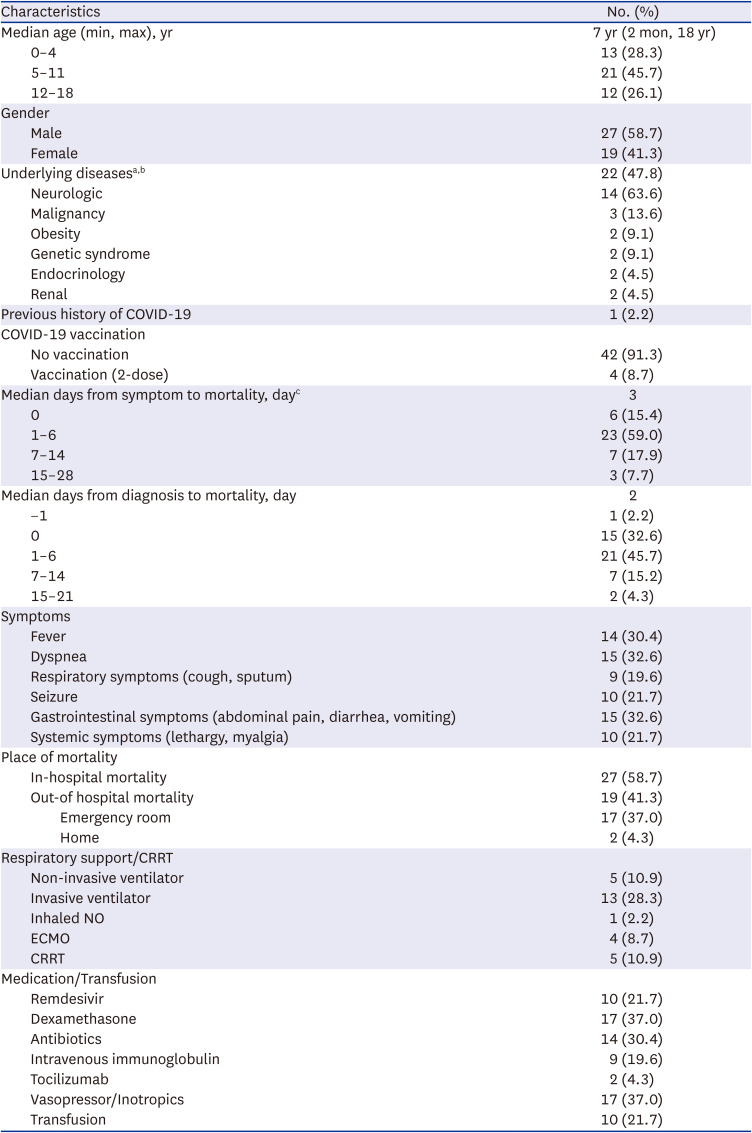
Up to September 3, 2022, 46 cases of COVID-19 associated deaths ≤ 18 years old were reported (
Table 1). Male subjects accounted for 58.7% (n = 27). The median age was 7 years (range: 2 months–18 years); 45.7% (n = 21) were 5–11 years of age, 28.3% (n = 13) were 0–4 years of age, and 26.1% (n = 12) were 12–18 years of age.
Table 1
COVID-19 cases in children in Korea during February 7, 2020 up to September 3, 2022
|
Observed period |
Total |
0–4 yr |
5–11 yr |
12–18 yr |
|
Total (Jan 20, 2020–Sep 3, 2022)a
|
8,001,265 |
1,554,195 |
3,173,169 |
3,273,901 |
|
COVID-19 cases |
5,388,338 |
970,761 |
2,399,722 |
2,017,855 |
|
Incidence per 100,000/day |
69.6 |
64.5 |
78.1 |
63.7 |
|
COVID-19 associated deaths |
46 |
13 |
21 |
12 |
|
CFR per 100,000 |
0.85 |
1.34 |
0.88 |
0.59 |
|
Mortality per 100,000 |
0.57 |
0.84 |
0.66 |
0.37 |
|
Pre-delta (Jan 20, 2020–Jul 24, 2021)a
|
8,204,990 |
1,677,023 |
3,215,416 |
3,312,551 |
|
COVID-19 cases |
20,863 |
3,818 |
7,210 |
9,835 |
|
Incidence per 100,000/day |
0.5 |
0.4 |
0.4 |
0.5 |
|
COVID-19 associated deaths |
0 |
0 |
0 |
0 |
|
CFR per 100,000 |
0.00 |
0.00 |
0.00 |
0.00 |
|
Mortality per 100,000 |
0.00 |
0.00 |
0.00 |
0.00 |
|
Delta (Jul 25, 2021–Jan 15, 2022)a
|
7,976,210 |
1,530,469 |
3,180,414 |
3,265,327 |
|
COVID-19 cases |
98,474 |
16,377 |
44,627 |
37,470 |
|
Incidence per 100,000/day |
7.1 |
6.1 |
8.0 |
6.6 |
|
COVID-19 associated deaths |
3 |
1 |
2 |
0 |
|
CFR per 100,000 |
3.05 |
6.11 |
4.48 |
0.00 |
|
Mortality per 100,000 |
0.04 |
0.07 |
0.06 |
0.00 |
|
Omicron (Jan 16, 2022–Sep 3, 2022)a
|
7,822,595 |
1,455,094 |
3,123,676 |
3,243,825 |
|
COVID-19 cases |
5,269,001 |
950,566 |
2,347,885 |
1,970,550 |
|
Incidence per 100,000/day |
312.9 |
282.8 |
325.4 |
263.0 |
|
COVID-19 associated deaths |
43 |
12 |
19 |
12 |
|
CFR per 100,000 |
0.82 |
1.26 |
0.81 |
0.61 |
|
Mortality per 100,000 |
0.59 |
0.82 |
0.61 |
0.31 |
|
Delta vs. omicron risk ratio of CFR (95% CI) |
0.28 (0.08–0.86) |
0.21 (0.03–0.86) |
0.18 (0.04–0.78) |
- |

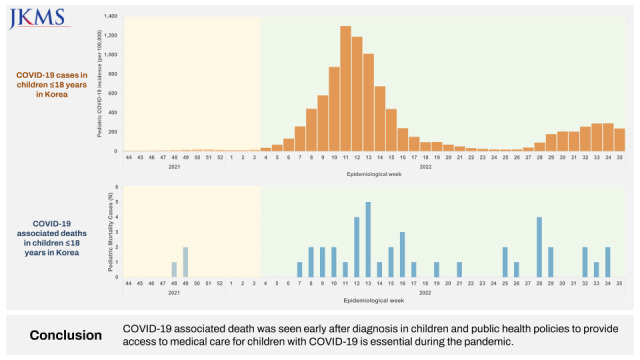
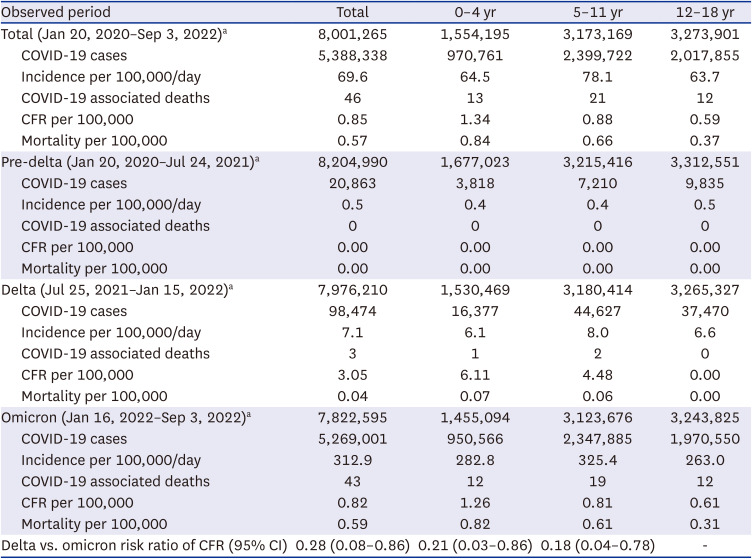
The incidence of pediatric COVID-19 cases and fatal cases by epidemiologic week are shown in
Fig. 1. Among children and adolescents ≤ 18 years of age, 5,388,338 cases were diagnosed with COVID-19 which accounts for 67.3% of the population. Forty-six cases of COVID-19 associated deaths occurred which shows a case fatality rate (CFR) of 0.85 per 100,000 cases in this population. According to age groups, the overall CFR for children 0–4 years of age was 1.34 per 100,000, for 5–11 years of age 0.88 per 100,000 and for 12–18 years of age 0.59 per 100,000. According to the period regarding variant of SARS-CoV-2 circulating, CFR of children ≤ 18 years of age decreased from 3.05 per 100,000 ≤ 18 years in the Delta dominant period (July 25, 2021–January 15, 2022) to 0.82 per 100,000 ≤ 18 years in the omicron dominant period (January 16, 2022–September 3, 2022).
3 During the surge of the highly transmissible omicron variant,
4 97.8% of all confirmed pediatric cases occurred and 93.5% of fatal cases were reported.
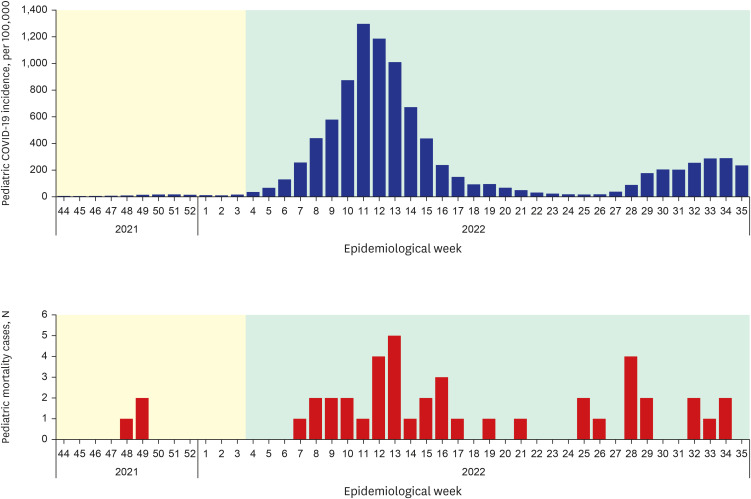 | Fig. 1Incidence of pediatric coronavirus disease 2019 cases and mortality cases per epidemiologic week. Yellow shade indicates the period with delta variant and green shade indicates period of dominancy of the omicron variant.
|
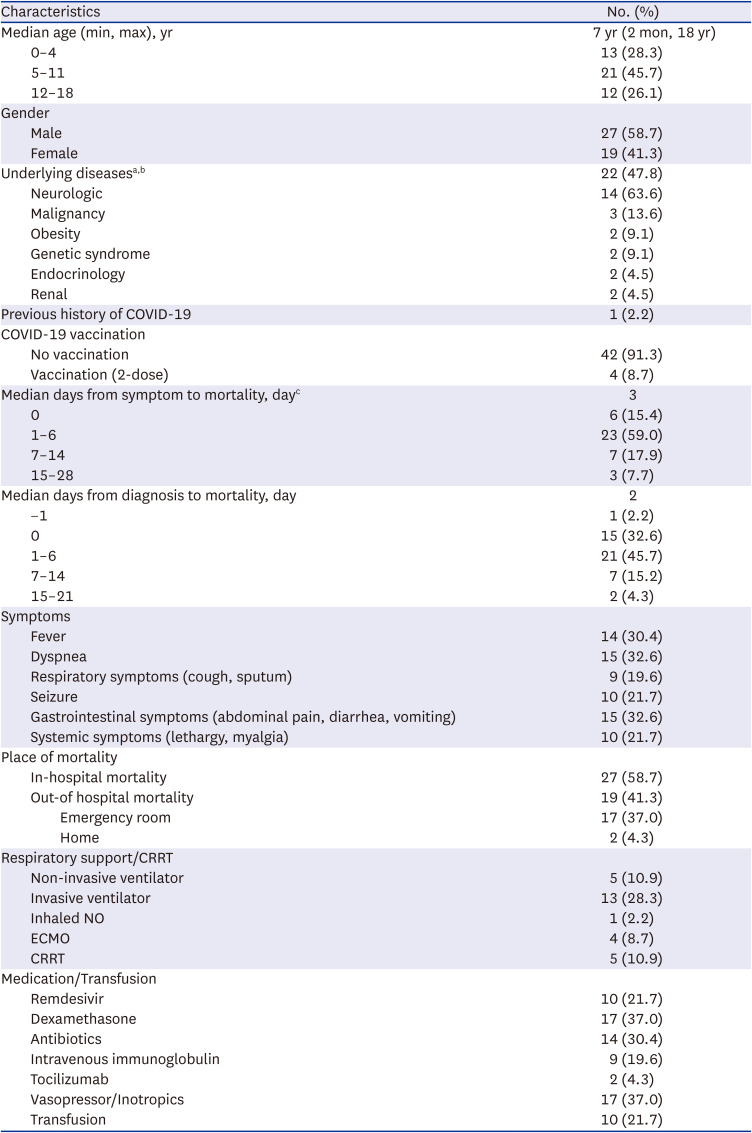
Demographics, comorbidities, and clinical presentation of fatal cases are shown in
Table 2. Among all cases, 47.8% (n = 22) had underlying diseases including neurologic diseases (n = 14), malignancy (n = 3), endocrinologic diseases (n = 2), obesity (n = 2), genetic syndrome (n = 2) and renal diseases (n = 2). Among these, one case had neurologic, endocrinologic and renal disease and one case had malignancy combined with renal disease. Among the 24 children with no underlying diseases, the reason for death was documented in 13 cases; myocarditis (n = 6), multiorgan failure (n = 3), disseminated coagulopathy (n = 1), brain swelling (n = 2), and encephalitis (n = 1). Among the 22 children with underlying diseases, the cause for death was documented in 9 cases and respiratory failure (n = 3), sepsis (n = 2), pneumonia (n = 1), pulmonary embolism (n = 1), cardiomyopathy (n = 1), and encephalitis (n = 1). One case was re-infected after 4 months in an immunocompromised child with malignancy. Four cases were vaccinated with 2 doses, all 12–18 years of age with underlying diseases (neurologic disease n = 2; obesity, n = 1; genetic disease n = 1) and 91.3% (n = 42) were not vaccinated. Among unvaccinated cases, 13 cases were 0–4 years of age and 8 cases and 21 cases were 12–18 years and 5–11 years of age, respectively.
Table 2
Demographics, comorbidities, and clinical presentation of children with mortality
|
Characteristics |
No. (%) |
|
Median age (min, max), yr |
7 yr (2 mon, 18 yr) |
|
0–4 |
13 (28.3) |
|
5–11 |
21 (45.7) |
|
12–18 |
12 (26.1) |
|
Gender |
|
|
Male |
27 (58.7) |
|
Female |
19 (41.3) |
|
Underlying diseasesa,b
|
22 (47.8) |
|
Neurologic |
14 (63.6) |
|
Malignancy |
3 (13.6) |
|
Obesity |
2 (9.1) |
|
Genetic syndrome |
2 (9.1) |
|
Endocrinology |
2 (4.5) |
|
Renal |
2 (4.5) |
|
Previous history of COVID-19 |
1 (2.2) |
|
COVID-19 vaccination |
|
|
No vaccination |
42 (91.3) |
|
Vaccination (2-dose) |
4 (8.7) |
|
Median days from symptom to mortality, dayc
|
3 |
|
0 |
6 (15.4) |
|
1–6 |
23 (59.0) |
|
7–14 |
7 (17.9) |
|
15–28 |
3 (7.7) |
|
Median days from diagnosis to mortality, day |
2 |
|
−1 |
1 (2.2) |
|
0 |
15 (32.6) |
|
1–6 |
21 (45.7) |
|
7–14 |
7 (15.2) |
|
15–21 |
2 (4.3) |
|
Symptoms |
|
|
Fever |
14 (30.4) |
|
Dyspnea |
15 (32.6) |
|
Respiratory symptoms (cough, sputum) |
9 (19.6) |
|
Seizure |
10 (21.7) |
|
Gastrointestinal symptoms (abdominal pain, diarrhea, vomiting) |
15 (32.6) |
|
Systemic symptoms (lethargy, myalgia) |
10 (21.7) |
|
Place of mortality |
|
|
In-hospital mortality |
27 (58.7) |
|
Out-of hospital mortality |
19 (41.3) |
|
|
Emergency room |
17 (37.0) |
|
|
Home |
2 (4.3) |
|
Respiratory support/CRRT |
|
|
Non-invasive ventilator |
5 (10.9) |
|
Invasive ventilator |
13 (28.3) |
|
Inhaled NO |
1 (2.2) |
|
ECMO |
4 (8.7) |
|
CRRT |
5 (10.9) |
|
Medication/Transfusion |
|
|
Remdesivir |
10 (21.7) |
|
Dexamethasone |
17 (37.0) |
|
Antibiotics |
14 (30.4) |
|
Intravenous immunoglobulin |
9 (19.6) |
|
Tocilizumab |
2 (4.3) |
|
Vasopressor/Inotropics |
17 (37.0) |
|
Transfusion |
10 (21.7) |

Among fatal cases, 58.7% (n = 27) occurred during admission whereas 41.3% (n = 19) occurred before admission. 4.3% (n = 2) were found dead before or on arrival and 37.0% (n = 17) died in the emergency department before hospitalization. The median days from diagnosis to death was 2 days (range: −1 day to 21 days). Thirty-seven percent (n = 17) died on the day of diagnosis; 41.3% (n = 19) within 1 to 5 days after diagnosis, 17.4% (n = 8) at 6 to 14 days, 4.3% (n = 2) at 15 to 21 days from the diagnosis. One patient was diagnosed with COVID-19 one day after death. Among the 39 subjects in which date of symptom onset was available, median time from symptom onset to death was 3 days (range: 0 day to 23 days). Of those, 15.4% (n = 6) died on the day of symptom onset and 59.0% (n = 23) at 1 to 5 days, 17.9% (n = 7) at 6 to 14 days, and 7.7% (n = 3) at 15 to 28 days after symptom onset.
When analyzing the symptoms of the cases, fever was reported in 30.4% (n = 14), respiratory symptoms (cough, sputum) in 19.6% (n = 9), dyspnea in 32.6% (n = 15), myalgia or lethargy in 21.7% (n = 10), altered consciousness in 26.1% (n = 12), seizure in 21.7% (n = 10) and gastrointestinal symptoms in 32.6% (n = 15). Pneumonia was diagnosed in 17.4% (n = 8) and two cases had combined bacteremia due to methicillin-resistant Staphylococcus aureus and Acinetobacter spp, respectively. Pharmacological treatments administered were remdesivir in 21.7% (n = 10), dexamethasone in 37.0% (n = 17), intravenous immunoglobulin in 19.6% (n = 9), tocilizumab in 4.3% (n = 2), and antibiotics in 30.4% (n = 14). None of the children had received nirmatrelvir/ritonavir or molnupiravir.
For respiratory support, 28.3% (n = 13) were on mechanical ventilation, 2.2% (n = 1) used inhaled nitrogen oxide and 8.7% (n = 4) applied extracorporeal membrane oxygenation.
In this report, we analyzed 46 COVID-19 associated pediatric deaths from the beginning of the pandemic up to September 3, 2022. Among fatal cases ≤ 18 years of age, approximately half had underlying diseases, which is similar with reports from other countries.
5 Only four cases were vaccinated, all with underlying diseases and 91.3% were unvaccinated among which 69.0% (n = 29) were ≥ 5 years of age. Currently, vaccination is recommended for all adolescents 12–18 years of age, booster is highly recommended for high risk groups and is optional for healthy adolescents.
6 Also, vaccination is optional for all children 5–11 years of age and highly recommended for high risk groups.
6 Further emphasis on vaccination in children especially with underlying diseases is important to prevent mortality in children with COVID-19.
COVID-19 associated pediatric deaths were none in 2020, three in 2021, and 43 cases up to September 3, 2022. However, the CFR was higher in 2021 compared with 2022. Thus, the overall increase in COVID-19 case number led to higher fatal case numbers in 2022. In 2022, the unprecedented surge of the highly transmissible omicron variant along with ease in social distancing attributed to the overall increase in COVID-19. A previous report also demonstrated that the increase in hospital admissions in children during the surge of omicron variant was related to the overall increase in disease rather than increase in disease severity.
7
The time to death from diagnosis in children was short and 41.3% of the COVID-19 deaths occurred out of hospital or in the emergency department. This is similar to a report in the US, which reported mortality out of the hospital of in the emergency department as 30.5% of children younger than 18 years.
8 Out of hospital mortality in children was more commonly seen in children in contrast to 10.4% of elders aged 64 to 74 years.
8 During the COVID-19 pandemic, screening and triage was emphasized to separate SARS-CoV-2 infected and non-infected individuals. Also, homecare was the primary healthcare measure for children with mild symptoms. Although these measures are important to prevent spread of SARS-CoV-2 infection in the hospital setting, this may also provide difficulties in access to the medical system due to the limited capacity for primary patient care in COVID-19 patients. Therefore, considering the relatively short interval from diagnosis to death in children and adolescents and the large proportion of COVID-19 deaths which occurred before admission in this population, primary care, patient referral and emergency care systems should be able to provide prompt and adequate care without delay for children and adolescents with COVID-19.
9
Although the overall incidence of pediatric COVID-19 deaths and CFRs are not high, there is an increase in cases since 2022. Comprehensive measures to protect children and adolescents will be necessary during the ongoing COVID-19 pandemic. These include vaccination policies to promote vaccination in high-risk groups, effort to increase alertness and awareness in medical personnel and the public for early detection of critical cases, public health measures to secure availability and access to medical care for children with COVID-19 and timely and effective treatment strategies.
Ethics statement
All data used in the analysis were collected during routine public health surveillance activities, as part of the legislated mandate of the health authority. This study was approved by the Institutional Review Board (IRB) of Korea University Anam Hospital (IRB No. 2022AN0413). Review from the IRB of the KDCA was exempted (2022-11-04-PE-A). We conducted the study in accordance with the principles of the Declaration of Helsinki.
Go to :