Abstract
Purpose
Limited data are available on the nationwide trend of treatments for chronic venous disease (CVD). The aim of the present study was to identify the nationwide trends of CVD treatments in Korea.
Methods
A serial, cross-sectional study was conducted with the use of time trends to analyze patients with CVD between 2010 and 2020. The trends in the number of patients and procedures were analyzed including sclerotherapy, open surgery, and endovenous thermal ablation (ETA). Health Insurance Review and Assessment Service data were used to analyze the trends. For the statistical analysis, MedCalc Statistical software was used. P < 0.05 was considered statistically significant.
Results
A total of 1,867,307 patients with CVD were managed in Korea between 2010 and 2020. The annual number of patients with CVD increased from 143,108 in 2010 to 219,319 in 2020 (risk ratio [RR], 1.53; P < 0.001). The percentage of patients with CVD who had venous ulcer gradually decreased from 3.1% in 2010 to 1.7% in 2020 (RR, 0.86; P < 0.001). The number of conventional surgeries including stripping and local resection of varicose veins decreased from 32,384 in 2010 to 21,792 in 2020 (RR, 0.67; P < 0.001). The number of ETAs performed increased, from 290 in 2011 to 12,126 procedures in 2020 (RR, 41.81; P < 0.001).
Chronic venous disease (CVD) encompasses a spectrum of venous diseases from simple telangiectasia and varicose veins to venous ulcers [1]. The disease is common but is often overlooked by healthcare services because of the underestimation of the severity and impact of the problem and incomplete recognition of the various symptoms of primary and secondary venous disorders [2]. Although many people seek medical attention for varicose veins because of their cosmetic appearance or associated symptoms, venous ulcerations have a marked impact on individuals’ social and occupational activities, quality of life, and financial resources. CVD has a significant impact on healthcare resources. Varicose veins affect more than 25 million adults in the United States, and more than 6 million people have advanced venous disease [3].
Open surgery such as stripping with high ligation of saphenous veins followed by phlebectomy has been the choice of treatment for a long time. Although this modality efficiently reduces symptoms and recurrences compared to those following only high ligation, surgery may often be related to significant postoperative complications such as bleeding, surgical site infection, thrombophlebitis, and nerve damage [45]. In 1999, a new and minimally invasive treatment for CVD was introduced, namely, endovenous thermal ablation (ETA). Currently, this procedure is the mainstream treatment for CVD because of its simplicity and several advantages over open surgery [6].
In England, the number of patients undergoing open surgery fell by 47% between 1998 and 2001, and the number of cases of transluminal procedures, including radiofrequency ablation (RFA) and endovenous laser ablation, in 2008 was twice that in 2006 [7]. According to the data from the Varicose Vein module of the American Venous Registry, ETA was the most frequently performed procedure for treatment of symptomatic saphenous vein reflux [8].
Until now, limited data on the nationwide trend of CVD treatments have been available in Korea. The aim of the present study was to identify the national trends of CVD treatments in Korea.
The present study was approved by the Institutional Review Board of Kyung Hee University Hospital at Gangdong (No. 2015-01-027). It was performed in accordance with the Declaration of Helsinki and written informed consent was waived due to its retrospective nature.
A serial, cross-sectional study was conducted using time trends to analyze patients with CVD between 2010 and 2020 in Korea. The present study endeavored to analyze trends in the number of patients with and procedures performed for CVD including sclerotherapy, conventional open surgery, RFA, and nonthermal ablation including cyanoacrylate glue (CAG) closure, and mechanochemical ablation (MOCA).
Data were collected from the Health Insurance Review and Assessment Service (HIRA). More than 98% of the Korean population is covered by National Health Insurance due to the universal health coverage system provided by the government. The HIRA gathers and accumulates the claims data nationally when Korean healthcare service providers seek reimbursements for healthcare services that the National Health Insurance Corporation agrees to cover. These national data correspond to the number of claims that are submitted by patients for inclusive healthcare services [9]. However, ETA, CAG closure, and MOCA are not reimbursed by the National Health Insurance. Therefore, the data on RFA and nonthermal ablation were collected from one of the device-supplying companies. The catheter types for which the number of sales were investigated to estimate the number of procedures were as follows; Closurefastand Venaseal (Medtronic, Minneapolis, MN, USA), and Clarivein (Merit Medical, South Jordan, UT, USA).
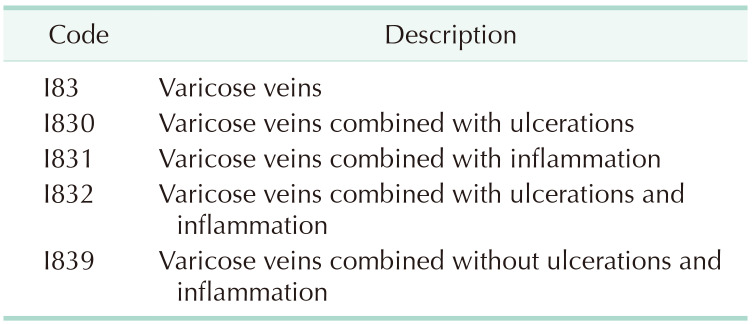
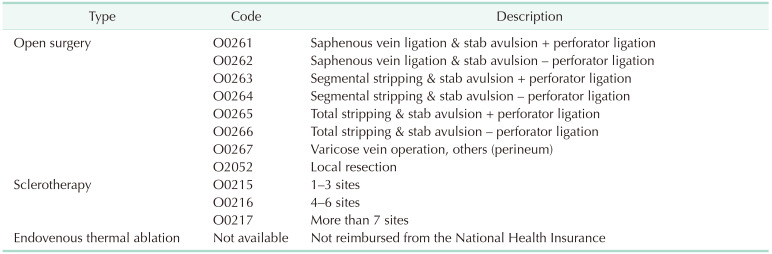
The HIRA contains the Electronic Data Interchange (EDI) database, which contains the disease, operation, and management codes. We collected the data on CVD using EDI codes. Table 1 summarizes the disease codes for CVD. There are 5 EDI codes related to CVD. I830 and I831 are relevant codes for varicose veins with ulcerations and inflammation, respectively. If a patient has an advanced form of CVD combined with ulcerations and inflammation, the condition is allocated disease code I832. I839 is the code for varicose veins without ulcerations and inflammation. I83 is the code that is representative of varicose veins. There are 11 EDI codes for procedures for CVD (Table 2). Open surgery, such as stripping with and without perforator ligation, has 8 codes. There are 3 EDI codes for sclerotherapy depending on the extent of treatment. Codes are not available for ETA because this procedure is not reimbursed by the National Health Insurance.
For the evaluation of trends in CVD treatment, we calculated the total number of patients treated for CVD and their sex distribution. For the evaluation of age distribution for each procedure, we calculated the number of procedures per 10-year intervals. For the evaluation of the trends in CVD treatments for the past 11 years, we analyzed the trend for the codes O0261–O0267 and O2052 for open surgery and the codes O0215–O0217 for sclerotherapy.
For statistical analysis, a linear-by-linear association was performed to determine trends in CVD treatments for this period. The Bland-Altman method was used to evaluate trends in population-adjusted frequencies. We measured the relative risk to evaluate trends using MedCalc Statistical software (Ostend, Belgium). A P-value less than 0.05 (2-sided) was considered statistically significant.
A total of 1,867,307 patients with CVD were managed in Korea between 2010 and 2020. The annual number of patients with CVD increased from 143,108 in 2010 to 219,319 in 2020 (risk ratio [RR], 1.53; P < 0.001) (Fig. 1). The total number of female patients was approximately twice that of male patients. The annual numbers of patients, of the male and female sexes, with CVD increased by 1.49 (P < 0.001) and 1.53 (P < 0.001) times, respectively.
The percentage of patients with CVD who has venous ulcer gradually decreased during the study period from 3.1% in 2010 to 1.7% in 2020. During the study period, the number of patients with CVD without venous ulcer increased from 138,653 in 2010 to 215,482 in 2020 (RR, 1.55; P < 0.001) (Fig. 2).
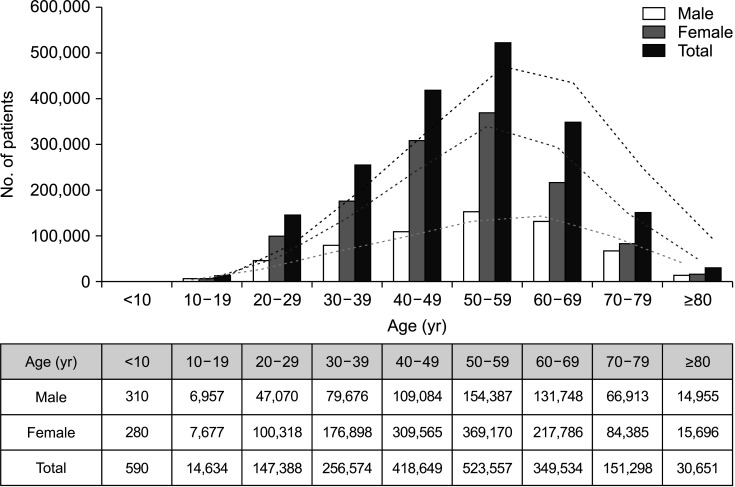
The number of patients who were diagnosed with CVD showed a parabolic pattern with age (Fig. 3). The number of procedures increased with age in patients aged up to 50 years and then decreased in those older than 50 years. The procedures were most frequently performed in patients in their 50s, followed by those in their 40s and 60s.
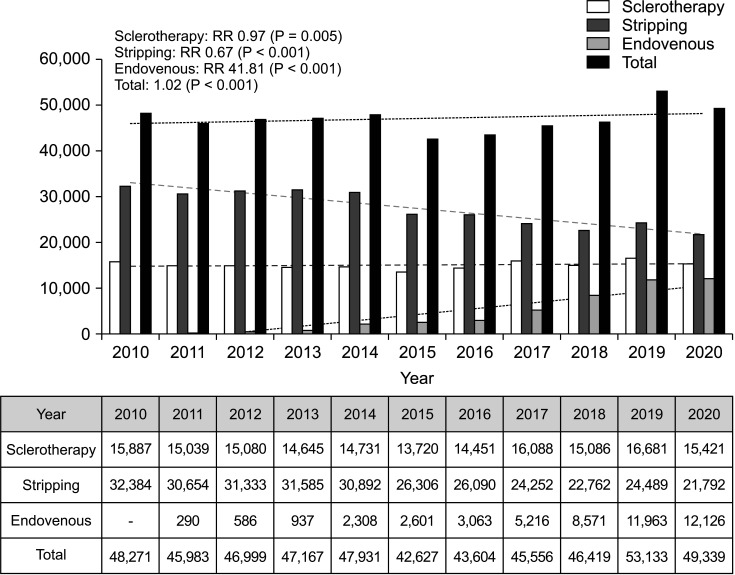
The number of conventional surgeries performed, including stripping and local resection of varicose veins, slightly decreased, from 32,384 in 2010 to 21,792 in 2020 (RR, 0.67; P < 0.001) (Fig. 4). The number of sclerotherapy procedures performed also slightly decreased, from 15,887 in 2010 to 15,421 in 2020 (RR, 0.97; P = 0.005). The number of ETAs performed markedly increased, from 290 in 2011 to 12,126 procedures in 2020 (RR, 41.81; P < 0.001).
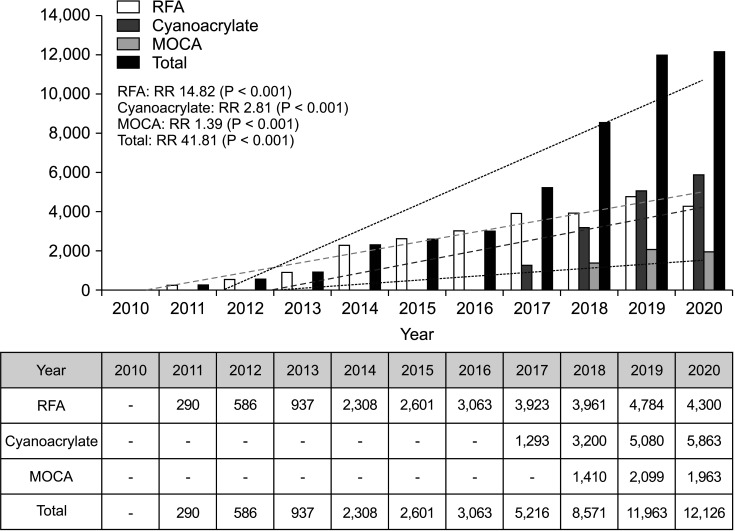
The annual trend for CVD treatment by ETA is changing. RFA was first started in ETA. It began in 2011 with 290 cases and the number performed gradually increased to 4,300 cases in 2020 (RR, 14.82; P < 0.001). In 2017, CAG closure was introduced and has increased dramatically over 4 years, from 1,293 instances in 2017 to 5,863 instances in 2020, and was the most applied procedure in ETA (RR, 2.81; P < 0.001). In 2018, MOCA was introduced, and it gradually increased from 1,410 instances in 2018 to 1,963 instances in 2020 (RR, 1.39; P < 0.001) (Fig. 5).
This study revealed nationwide trends in CVD treatments in Korea. The total number of patients with CVD increased by 1.53 times in the past 11 years. The number of procedures performed increased with age, with the peak in patients in their 50s. In the past 11 years, the number of open surgeries performed decreased by 33%, which is statistically significant, and the number of sclerotherapy procedures decreased by 3%. However, the number of EVTs significantly increased, by up to 41.8 times.
The annual number of patients with CVD gradually increased, which may be explained by several factors. First, the number of patients who prefer to receive treatment has increased because of the increased interest in personal health and quality of life. Second, the population of those older in age has increased. In general, older age is the most relevant risk factor for CVD [1011]. The population of South Korea is aging more rapidly than the population of any other country. It became an aging society in 2000, was an aged society by 2018, and will be a super-aged society by 2026. The percentage of individuals at least 50 years old was 25% in 2010 and expected to exceed 33% in 2020 [12].
Obesity is another important risk factor for the development of CVD [13]. Obesity is associated with higher intraabdominal pressure, which reduces venous return from the limbs [14]. Studies have demonstrated the efficacy of weight loss after gastric surgery on the healing of severe venous stasis disease [15]. Han et al. [16] examined the national trends in adolescent obesity in South Korea. The prevalence of obesity in 2013 increased from that in 2006 in South Korean adolescents of both sexes and of various age groups. Interestingly, the prevalence of obesity in adolescent males in each age group was about twice as high compared to that in adolescent females.
Trends in annual numbers of patients with CVD and procedures performed showed increasing patterns, except in 2015. There are several reasons for the decreasing numbers in 2015. It may be presumed that the downward economic condition and the outbreak of the Middle East respiratory syndrome (MERS) in 2015 [17]. During the outbreak of MERS, the socioeconomic impact in Korea was significant. The MERS epidemic was not a simple public health problem for Koreans at the time of the outbreak but showed implications for the state of the overall economy and society beyond the healthcare sector in Korea. The number of foreign tourists decreased by 41% compared to that in the same month of the previous year. Eventually, Korea lost US$ 10 billion, which was expected to reduce the gross domestic product growth rate by 0.1% in 2015 [18].
From our study, we can determine that the proportion of RFAs performed has increased, while that of conventional open surgeries performed has decreased. As can be inferred from many studies comparing RFA and open surgery, RFA has many advantages [1920212223]. RFA can be performed with a very small skin incision compared to that in open surgery. Therefore, postoperative pain is lower, the hospitalization period is shorter, and patients can resume daily life activities faster than after undergoing open surgery. In addition, there is little scarring due to small wounds, which is better cosmetically. There are few complications of RFA, but the treatment results are similar to or even superior to those of open surgery.
There are several limitations in our study. There was an inevitable limit to the number of variables that could be measured, because the study was a retrospective analysis with the HIRA dataset, an administrative database. Follow-up data, long-term outcomes, and data on non-benefit insurance were unavailable. HIRA database does not provide patient-specific information. Therefore, it was impossible to remove duplication, and there were duplicate data in the annual patient number. Also, the patient number may be overestimated, since the code used to search for CVD can be used without objective tests such as ultrasonography.
The most frequently performed ETA in Korea is laser ablation but since our design contains only the data from HIRA, public health insurance, and the result could not match the reality. Further studies are required with the collection of more detailed data, such as treatment results, postoperative complications, and degree of patient satisfaction with each treatment. There are only a few studies and collected data on venous procedures in Korea. Despite the limitation, our study shows strength in analyzing the venous procedures performed in Korea.
In conclusion, the number of patients with CVD in Korea annually was between about 140,000 and 210,000; the numbers have increased slightly during the past 11 years. The percentage of patients with CVD with venous ulcer gradually decreased. The number of female patients was about twice the number of male patients, and patients with CVD were most commonly in their 50s. The number of cases of open surgery and sclerotherapy decreased, whereas those of endovenous therapy increased.
References
1. White JV, Ryjewski C. Chronic venous insufficiency. Perspect Vasc Surg Endovasc Ther. 2005; 17:319–327. PMID: 16389426.
2. Eberhardt RT, Raffetto JD. Chronic venous insufficiency. Circulation. 2005; 111:2398–2409. PMID: 15883226.
3. Beebe-Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol. 2005; 15:175–184. PMID: 15723761.
4. Durkin MT, Turton EP, Wijesinghe LD, Scott DJ, Berridge DC. Long saphenous vein stripping and quality of life: a randomised trial. Eur J Vasc Endovasc Surg. 2001; 21:545–549. PMID: 11397030.
5. Perkins JM. Standard varicose vein surgery. Phlebology. 2009; 24 Suppl 1:34–41. PMID: 19307439.
6. Joh JH, Kim WS, Jung IM, Park KH, Lee T, Kang JM. Consensus for the treatment of varicose vein with radiofrequency ablation. Vasc Specialist Int. 2014; 30:105–112. PMID: 26217628.
7. Kanwar A, Hansrani M, Lees T, Stansby G. Trends in varicose vein therapy in England: radical changes in the last decade. Ann R Coll Surg Engl. 2010; 92:341–346. PMID: 20501021.
8. Almeida J, Kabnick L, Wakefield T, Raffetto J, McLafferty R, Pappas P, et al. Management trends for chronic venous insufficiency across the United States: a report from the American Venous Registry. J Vasc Surg Venous Lymphat Disord. 2013; 1:100.
9. Kim L, Kim JA, Kim S. A guide for the utilization of health insurance review and assessment service national patient samples. Epidemiol Health. 2014; 36:e2014008. PMID: 25078381.
10. Kroeger K, Ose C, Rudofsky G, Roesener J, Hirche H. Risk factors for varicose veins. Int Angiol. 2004; 23:29–34. PMID: 15156127.
11. Callam MJ. Epidemiology of varicose veins. Br J Surg. 1994; 81:167–173. PMID: 8156326.
12. Park J, Kim SG, Park JS, Han B, Kim KB, Kim Y. Hazards and health problems in occupations dominated by aged workers in South Korea. Ann Occup Environ Med. 2017; 29:27. PMID: 28670457.
13. Lee AJ, Evans CJ, Allan PL, Ruckley CV, Fowkes FG. Lifestyle factors and the risk of varicose veins: Edinburgh Vein Study. J Clin Epidemiol. 2003; 56:171–179. PMID: 12654412.
14. Segiet OA, Brzozowa-Zasada M, Piecuch A, Dudek D, Reichman-Warmusz E, Wojnicz R. Biomolecular mechanisms in varicose veins development. Ann Vasc Surg. 2015; 29:377–384. PMID: 25449990.
15. Sugerman HJ, Sugerman EL, Wolfe L, Kellum JM, Schweitzer MA, DeMaria EJ. Risks and benefits of gastric bypass in morbidly obese patients with severe venous stasis disease. Ann Surg. 2001; 234:41–46. PMID: 11460821.
16. Han K, Park S, Symanzik J, Choi S, Ahn J. Trends in obesity at the national and local level among South Korean adolescents. Geospat Health. 2016; 11:381. PMID: 27245793.
17. Oh MD, Park WB, Park SW, Choe PG, Bang JH, Song KH, et al. Middle East respiratory syndrome: what we learned from the 2015 outbreak in the Republic of Korea. Korean J Intern Med. 2018; 33:233–246. PMID: 29506344.
18. Lee SI. Costly lessons from the 2015 Middle East respiratory syndrome coronavirus outbreak in Korea. J Prev Med Public Health. 2015; 48:274–276. PMID: 26639740.
19. Lurie F, Creton D, Eklof B, Kabnick LS, Kistner RL, Pichot O, et al. Prospective randomized study of endovenous radiofrequency obliteration (closure procedure) versus ligation and stripping in a selected patient population (EVOLVeS Study). J Vasc Surg. 2003; 38:207–214. PMID: 12891099.
20. Lurie F, Creton D, Eklof B, Kabnick LS, Kistner RL, Pichot O, et al. Prospective randomised study of endovenous radiofrequency obliteration (closure) versus ligation and vein stripping (EVOLVeS): two-year follow-up. Eur J Vasc Endovasc Surg. 2005; 29:67–73. PMID: 15570274.
21. Goode SD, Chowdhury A, Crockett M, Beech A, Simpson R, Richards T, et al. Laser and radiofrequency ablation study (LARA study): a randomised study comparing radiofrequency ablation and endovenous laser ablation (810 nm). Eur J Vasc Endovasc Surg. 2010; 40:246–253. PMID: 20537570.
22. Nordon IM, Hinchliffe RJ, Brar R, Moxey P, Black SA, Thompson MM, et al. A prospective double-blind randomized controlled trial of radiofrequency versus laser treatment of the great saphenous vein in patients with varicose veins. Ann Surg. 2011; 254:876–881. PMID: 21934487.
23. Rasmussen LH, Lawaetz M, Bjoern L, Vennits B, Blemings A, Eklof B. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Br J Surg. 2011; 98:1079–1087. PMID: 21725957.
Fig. 1
Total number of patients with chronic venous diseases per year analyzed using the Bland-Altman method. RR, risk ratio.

Fig. 2
Total number of patients with and without venous ulcer analyzed using the Bland-Altman method. RR, risk ratio.
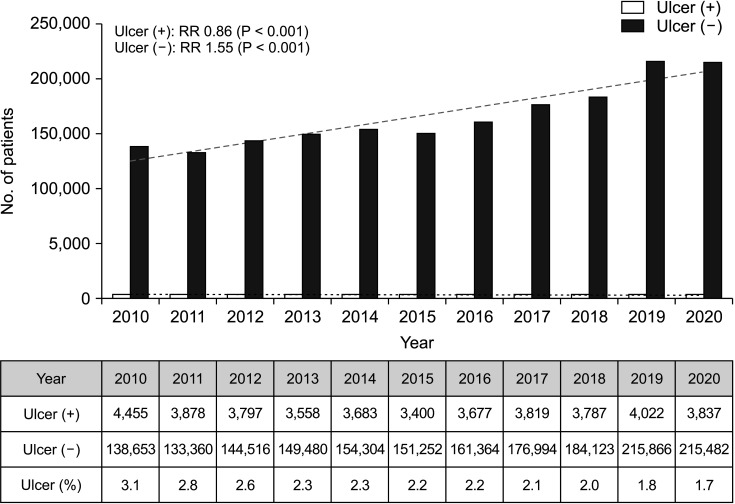
Fig. 4
Trends of sclerotherapy, surgical stripping, and endovenous procedures per year. Sclerotherapy was counted by procedure and endovenous procedures included radiofrequency ablation, cyanoacrylate glue closure, and mechanochemical ablation. RR, risk ratio.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download