Abstract
Purpose
Endovascular aneurysm repair (EVAR) has lower perioperative mortality and morbidity rates and shorter hospital stays when compared to open surgical repair (OSR) in octogenarian patients. However, its long-term results remain unclear. Hence, we aimed to analyze and compare the long-term outcomes of OSR and EVAR in this aging population.
Methods
This single-center, retrospective, observational study analyzed the data of patients older than 80 years who underwent primary repair of an abdominal aortic aneurysm (AAA) between 2011 and 2016 in our hospital. The primary outcomes were in-hospital complications and 30-day mortality, while the secondary outcomes included all-cause mortality and reintervention rate.
Results
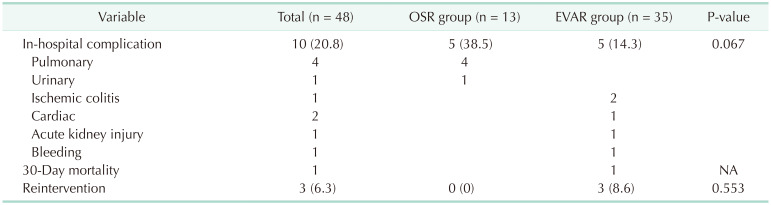
Among the 48 patients with elective AAA repair, 13 underwent OSR and 35 underwent EVAR. In-hospital complications occurred in 10 patients (20.8%), 5 for OSR (38.5%) and 5 for EVAR (14.3%) with no significant difference between the groups (P = 0.067). In the OSR group, pulmonary complications were the most common events; in the EVAR group, 2 patients had ischemic colitis diagnosed with sigmoidoscopy and recovered by conservative treatment. The 1- and 5-year survival rates were 77.8% and 55.6% in the OSR group, and 66.0% and 54.9% in the EVAR group, respectively. The reintervention rate was 8.6% for the EVAR group; none of the OSR group were readmitted.
Endovascular aneurysm repair (EVAR) is the standard treatment for infrarenal abdominal aortic aneurysms (AAAs) [1]. Compared with open surgical repair (OSR), EVAR has lower perioperative mortality and morbidity rates and shorter hospital stays [2]. In a previous large population-based study, EVAR had a higher survival rate (up to 3 years) than OSR [3].
According to the Society for Vascular Surgery guidelines, patients are advised to undergo AAA repair when an aneurysm diameter reaches 5.5 cm. The applicability of these guidelines to higher-risk populations must be considered on a case-by-case basis [4]. Unfortunately, whether these guidelines are appropriate for the older population remains unclear. Age is a well-known independent risk factor for death after AAA repair [2567]. Aside from AAA, the risk of death from any cause is substantially higher in octogenarians owing to their age.
The association between octogenarians and AAA repair has not been prospectively analyzed because patients older than 80 years are often excluded from or poorly represented in randomized trials. Knowledge on the long-term outcomes of OSR versus EVAR in octogenarian patients would provide insight into the appropriate treatment selection and management of these patients. In this study, we aimed to review our center’s data on AAA repair outcomes, specifically between EVAR and OSR in octogenarians, with regard to safety, short-term results, and long-term survival.
In this single-center, retrospective, observational study, we analyzed the data extracted from the medical records of patients aged over 80 years who underwent primary repair of AAAs between 2011 and 2016. The study period started in 2011 since there were only few cases of EVAR were performed before 2011; it ended in 2016 for a 5-year follow-up.
Institutional Review Board of the Asan Medical Center in the Republic of Korea approved the study protocol. Considering the retrospective study design, the requirement for informed patient consent was waived.
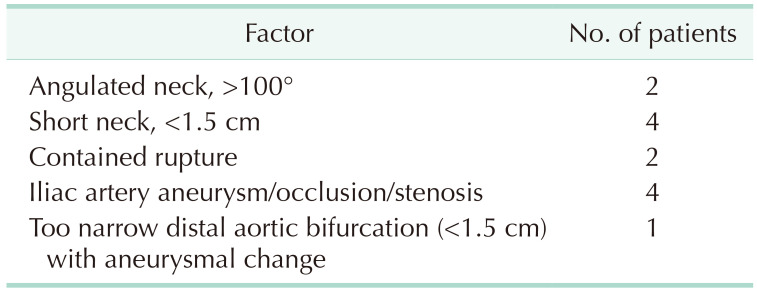
These patients underwent either EVAR or OSR. If the anatomy of the aorta was suitable for EVAR, then EVAR was performed; otherwise, OSR was performed. The most common reason for performing OSR was the existence of a hostile neck, which refers to an angulated neck or short neck of less than 15 mm. All procedures were performed electively. Those with ruptured AAAs were excluded from the study.
OSR was performed using a midline incision and the transperitoneal approach with an infrarenal clamp and bifurcated graft. Patients who required suprarenal clamping were excluded. Meanwhile, EVAR was performed with Endurant (Medtronic Inc, Minneapolis, MN, USA), Zenith (Cook Medical, Bloomington, IN, USA), or Excluder (W. L. Gore & Associates, Inc., Newark, DE, USA) endografts. There were 2 operators; one preferred femoral artery cut-down access under general anesthesia, and the other preferred totally percutaneous approach under local anesthesia. Unilateral internal iliac artery embolization was done for 5 patients due to ipsilateral common iliac artery aneurysm. One of the patients underwent the iliac branch device to preserve the internal iliac artery.
A cerebrovascular attack was defined as a history of stroke or transient ischemic attack. Having an abnormal stress test, previous myocardial infarction, or a history of coronary artery revascularization indicated ischemic heart disease. Preoperative chronic kidney disease was defined as a serum creatinine level of >2.0 mg/dL or dependence on dialysis. A history of radiological or surgical interventions for peripheral arterial occlusive disease (PAOD) or an ankle-brachial index of ≤0.9, as measured with Doppler ultrasound, indicated PAOD [8]. A positive pulmonary function test or the frequent need for an inhaler or steroid treatment indicated chronic obstructive pulmonary disease (COPD). Smoking history was gathered according to self-reports (current or ex-smoker) in a medical questionnaire.
The primary outcomes were in-hospital complications and 30-day mortality, while the secondary outcomes included all-cause mortality and reintervention rate. An in-hospital complication was defined as when the expected hospitalization period was extended because of a specific health problem.
The patients’ baseline and clinical characteristics, exact time of death, and clinical outcomes were recorded. Categorical variables are presented as frequencies or percentages and continuous variables are presented as means and standard deviation. Differences between the OSR and EVAR groups were analyzed using chi-square tests for categorical variables and Student t-tests for continuous variables. Cox proportional hazard models were used for univariate and multivariate analyses of the associations between clinical variables. The univariate Cox proportional hazard regression models were fitted to calculate the hazard ratios with 95% confidence intervals. Variables with a P-value of <0.1 for univariate analysis were included in multivariate Cox proportional hazard regression models. We considered a P-value of <0.05 to be statistically significant. All statistical data were analyzed using IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA).
Between January 1, 2011 and December 31, 2016, 550 consecutive patients aged over 40 years underwent elective primary repair of an infrarenal AAA. Among them, 272 underwent OSR (49.5%), and 278 underwent EVAR (50.5%). In particular, 48 consecutive patients aged ≥80 years underwent elective AAA repair, in which there were 13 OSR procedures and 35 EVAR procedures. The baseline comorbidities and the rates of hypertension, COPD, and PAOD were similar between both groups (Table 1).
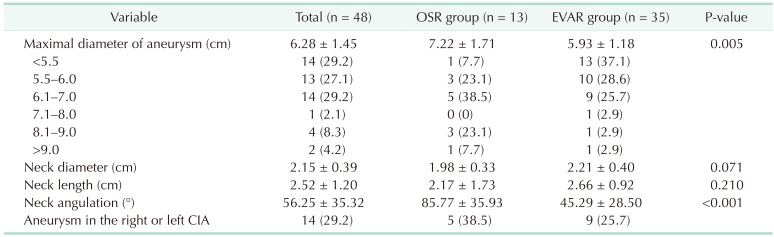
The anatomic differences between the OSR group and the EVAR group are summarized in Table 2. The average maximal diameter of aneurysm was greater in the OSR group than in the EVAR group (7.22 ± 1.71 cm vs. 5.93 ± 1.18 cm, P = 0.005). Neck angulation also was greater in the OSR group than in the EVAR group (85.77° ± 35.93° vs. 45.29° ± 28.50°, P < 0.001). Factors that EVAR was not applicable include short neck, angulated neck, aneurysmal involvement of iliac arteries, and narrow distal aorta (Table 3).
In the OSR group, bifurcated graft interposition was performed with Gelsoft grafts (Terumo Aortic, Tokyo, Japan) under general anesthesia. Meanwhile, the EVAR procedure involved either bifurcated graft insertion or aorto-uni-iliac endograft insertion using femoral-femoral bypass in 31 (88.6%) and 4 patients (11.4%), respectively. In the EVAR group, Medtronic Endurant, Cook Zenith, and Gore Excluder endografts were used in 24 (68.6%), 9 (25.7%), and 2 patients (5.7%), respectively. EVAR was performed under general anesthesia in 22 patients (62.9%) and local anesthesia in 13 patients (37.1%).
In-hospital complications occurred in 10 patients (20.8%), with 5 in the OSR group (38.5%) and 5 in the EVAR group (14.3%). No significant difference between the groups was noted (P = 0.067) (Table 4). In the OSR group, pulmonary complications were the most common events, which included atelectasis and pneumonia. In addition, 1 patient underwent a Double J stent insertion because of ureter injury. In the EVAR group, 2 patients had ischemic colitis diagnosed by sigmoidoscopy and recovered by conservative treatment. One patient experienced myocardial infarction, and another patient had acute kidney injury whose renal function was normal preoperatively. One patient required embolization due to bleeding in the femoral puncture site. Most common type of endoleak was type II originated from lumbar arteries or the inferior mesenteric artery. Seven patients (20.0%) had type II endoleaks on immediate follow-up CT scans taken 2 to 4 days after the procedure. Three patients required reintervention to treat endoleaks. The reintervention rate of 8.6% during 5 years after EVAR; 1 patient had a type Ib endoleak. None of the patients in the OSR group were readmitted.
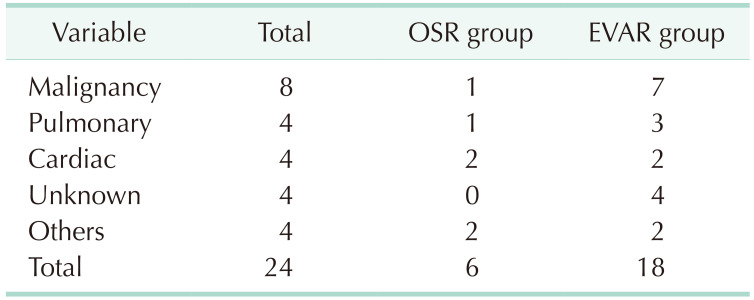
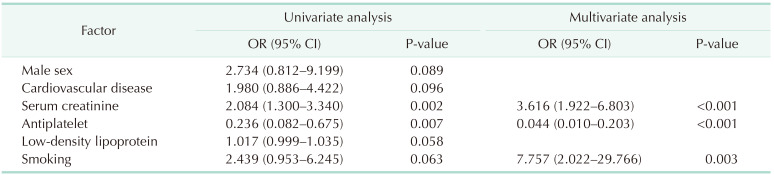
The median survival was 57.8 months in the OSR group and 56.42 months in the EVAR group, with no statistically significant difference between both groups (P = 0.686) (Fig 1). The 1-, 3-, and 5-year survival rates were 77.8%, 71.4%, and 55.6% in the OSR group and 66.0%, 43.2%, and 54.9% in the EVAR group, respectively. Within the study period, 24 out of 48 patients died, of which 6 were from the OSR group and 18 were from the EVAR group. The median follow-up period was 16.6 months for the OSR group and 22 months for the EVAR group. Table 5 enumerates the causes of death and Table 6 summarizes the factors affecting mortality. There were no aneurysm-related deaths during the follow-up period. For the OSR group, the median length of hospital stay after the operation was 11 days and the median length of the intensive care unit (ICU) stay was 1 day. For the EVAR group, the median length of hospital stay after the operation was 6 days and the median length of ICU stay was 1 day. Overall, the difference in procedures did not affect patient survival. The mortality rate tended to be higher in patients with high serum creatinine levels, no antiplatelets, and a history of smoking.
The risks and benefits of elective AAA repair in the older population remain controversial. Although enlarged aneurysms have a potential risk for rupture, the risks associated with both OSR and EVAR are substantial [9]. In octogenarian patients, EVAR has the benefits of lower perioperative mortality and morbidity rates and shorter hospital stays compared to OSR; however, its long-term results remain uncertain. In a recent review of the Vascular Quality Initiative database including 21,874 patients who underwent infrarenal AAA repair, an age of over 80 years increased the risks of 30-day and 1-year mortality by 223% and 187%, respectively [10].
In this study, we compared the short- and long-term results of OSR and EVAR in octogenarians. Patients aged 80 years and older who underwent elective OSR or EVAR had similar outcomes. Elective EVAR had no survival benefit at 1 and 5 years compared to OSR, which is inconsistent with other recent findings. Scallan et al. [11] demonstrated the survival rate at 1 year was significantly higher for the elective EVAR group at 93% compared with 84% in the elective OSR group using a Kaplan-Meier survival analysis; however, the survival at 5 years showed no significant difference between the EVAR group (57%) and the OSR group (59%).
The underlying cause of AAA repair poor outcomes in octogenarian patients is unknown, but it could be related to the greater comorbidity burden seen in this population [10]. The present study showed that the short-term morbidity and mortality rates of OSR and EVAR were not high. In the OSR group, the predominant cause of in-hospital complications was pneumonia with delayed ventilation care. Postoperatively, 1 patient in the EVAR group died due to myocardial infarction, whereas no one died in the OSR group. During the follow-up period, malignancy, cardiac disease, and lung disease affected mortality, with malignancy as the most common cause of mortality. Notably, no death caused by AAA-related complications was confirmed. The difference in median survival from that reported in previous studies was that the malignancy-related mortality was high.
Moreover, the reintervention rate of 8.6% seen in this study was similar to that in the EVAR 1 and EVAR 2 trials, in which the secondary intervention rates were 7% and 9.4% for procedures using Zenith and Talent (Medtronic Inc.) endografts, respectively. Elderly patients often have more complex anatomy to treat, with severe atherosclerosis or tortuous vessels [11]. This might lead to a greater chance of instruction for use violations. These relatively high reintervention rates should serve as a caution against using standard EVAR in octogenarians with nonideal anatomy because nonadherence to the procedure instructions increases the risk for graft-related complications over time [1112]. Differences in the treatment methods for AAAs in older patients do not significantly affect patient prognosis. In determining the appropriate method, surgeons should first determine whether the treatment is currently needed in consideration of underlying diseases and life expectancy. Then the treatment method should be chosen in consideration of the patient’s anatomical variation.
This study showed short-term and long-term outcomes in AAA repair for the patients older than 80 years. However, our study had a few limitations. First, it was a single-center study with a retrospective analysis, which has inherent limitations. Selection and information biases on the part of physicians or patients are also possible. Additionally, other factors such as the operation time and intraoperative blood loss were not investigated. Smoking was investigated as an overall survival risk factor; however, the data on this could be inaccurate because it was self-reported by the patients and caregivers during treatment. The study also had a small sample size, thereby limiting our results. Furthermore, our study population only consisted of patients of Asian descent.
In conclusion, the difference in procedures did not affect patient survival. Nevertheless, AAA repair should be performed with extreme caution in octogenarians, age being a well-known independent risk factor for death after AAA repair. Compared to other studies, this study showed that the 1-year survival rate was lowered in patients who underwent EVAR than in those who underwent OSR, although the 5-year survival rates were similar between the procedures. The reintervention rate was similar to the previous studies. Therefore, OSR does not necessarily have a worse prognosis than EVAR; for selected patients, OSR is a feasible option. Individual risk stratification must be preceded before the selection of an appropriate treatment method.
References
1. Speziale F, Ruggiero M, Sbarigia E, Marino M, Menna D. Factors influencing outcome after open surgical repair of juxtarenal abdominal aortic aneurysms. Vascular. 2010; 18:141–146. PMID: 20470684.
2. Henebiens M, Vahl A, Koelemay MJ. Elective surgery of abdominal aortic aneurysms in octogenarians: a systematic review. J Vasc Surg. 2008; 47:676–681. PMID: 18207352.
3. Lange C, Leurs LJ, Buth J, Myhre HO. EUROSTAR collaborators. Endovascular repair of abdominal aortic aneurysm in octogenarians: an analysis based on EUROSTAR data. J Vasc Surg. 2005; 42:624–630. PMID: 16242543.
4. Brewster DC, Cronenwett JL, Hallett JW Jr, Johnston KW, Krupski WC, Matsumura JS, et al. Guidelines for the treatment of abdominal aortic aneurysms: report of a subcommittee of the Joint Council of the American Association for Vascular Surgery and Society for Vascular Surgery. J Vasc Surg. 2003; 37:1106–1117. PMID: 12756363.
5. Ambler GK, Gohel MS, Mitchell DC, Loftus IM, Boyle JR. Audit and Quality Improvement Committee of the Vascular Society of Great Britain and Ireland. The Abdominal Aortic Aneurysm Statistically Corrected Operative Risk Evaluation (AAA SCORE) for predicting mortality after open and endovascular interventions. J Vasc Surg. 2015; 61:35–43. PMID: 24985535.
6. Tang T, Walsh SR, Prytherch DR, Lees T, Varty K, Boyle JR, et al. VBHOM, a data economic model for predicting the outcome after open abdominal aortic aneurysm surgery. Br J Surg. 2007; 94:717–721. PMID: 17514694.
7. Shahidi S, Schroeder TV, Carstensen M, Sillesen H. Outcome and survival of patients aged 75 years and older compared to younger patients after ruptured abdominal aortic aneurysm repair: do the results justify the effort? Ann Vasc Surg. 2009; 23:469–477. PMID: 19136232.
8. Huber TS, Carter JW, Carter RL, Seeger JM. Patency of autogenous and polytetrafluoroethylene upper extremity arteriovenous hemodialysis accesses: a systematic review. J Vasc Surg. 2003; 38:1005–1011. PMID: 14603208.
9. Hicks CW, Obeid T, Arhuidese I, Qazi U, Malas MB. Abdominal aortic aneurysm repair in octogenarians is associated with higher mortality compared with nonoctogenarians. J Vasc Surg. 2016; 64:956–965. PMID: 27364946.
10. Lagergren E, Chihade D, Zhan H, Perez S, Brewster L, Arya S, et al. Outcomes and durability of endovascular aneurysm repair in octogenarians. Ann Vasc Surg. 2019; 54:33–39. PMID: 30244017.
11. Scallan O, Novick T, Power AH, DeRose G, Duncan A, Dubois L. Long-term outcomes comparing endovascular and open abdominal aortic aneurysm repair in octogenarians. J Vasc Surg. 2020; 71:1162–1168. PMID: 31519509.
12. Herman CR, Charbonneau P, Hongku K, Dubois L, Hossain S, Lee K, et al. Any nonadherence to instructions for use predicts graft-related adverse events in patients undergoing elective endovascular aneurysm repair. J Vasc Surg. 2018; 67:126–133. PMID: 28760581.
Fig. 1
A cumulative Kaplan-Meier graph of the overall survival of patients who underwent abdominal aortic aneurysm repair based on the open surgical repair (OSR) or endovascular aneurysm repair (EVAR) procedure methods.
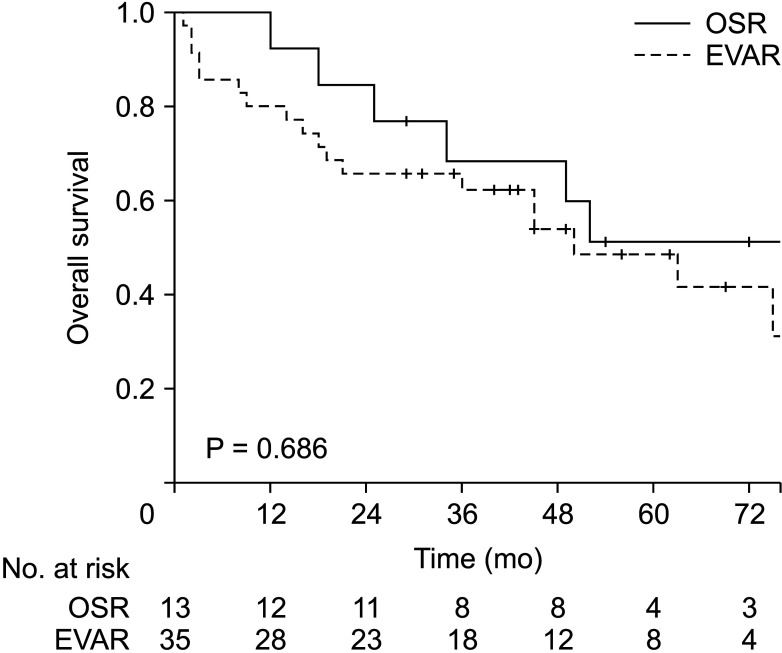
Table 1
Baseline characteristics of patients in each group
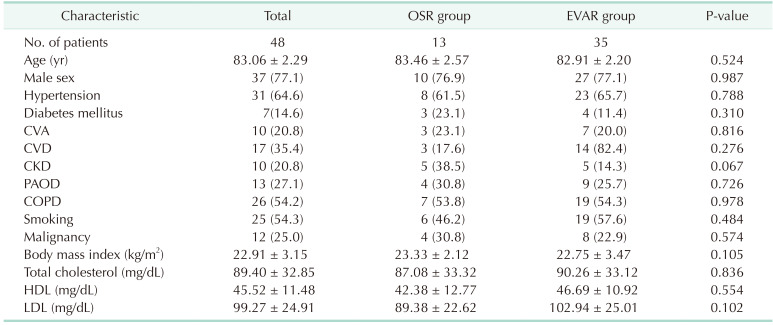
Values are presented as number only, mean ± standard deviation, or number (%).
OSR, open surgical repair; EVAR, endovascular aneurysm repair; CVA, cerebrovascular accident; CVD, cardiovascular disease; CKD, chronic kidney disease; PAOD, peripheral arterial occlusive disease; COPD, chronic obstructive pulmonary disease; HDL, high-density lipoprotein; LDL, low-density lipoprotein.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download