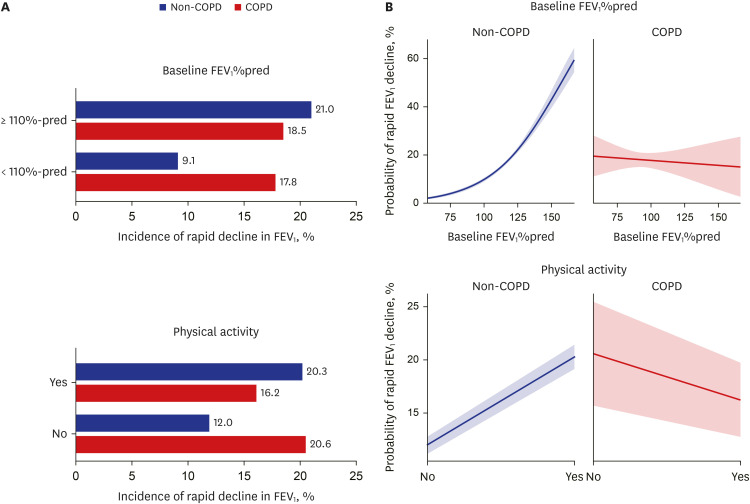
 | Fig. 1The risk of rapid function decline in FEV1 according to physical activity and baseline FEV1%pred. (A) Incidence of rapid decline in FEV1 between non-COPD and COPD groups. (B) Interaction plot of physical activity and baseline FEV1%pred for the risk of rapid lung function decline in FEV1.FEV1 = forced expiratory volume in 1 second, COPD = chronic obstructive pulmonary disease.
|
Abstract
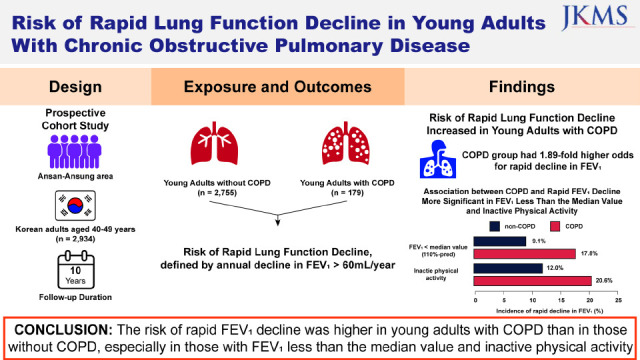
It is unclear whether young adults with chronic obstructive pulmonary disease (COPD) are at an increased risk of rapid lung function decline. A total of 2,934 Korean adults aged 40–49 years who had consecutive lung function measurements were included. COPD was defined as pre-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity < lower limit of normal. The risk of rapid decline in FEV1, defined as ≥ 60 mL/year, was assessed using multivariable logistic regression analysis. In the multivariable model, a significantly higher risk of rapid decline in FEV1 was observed for the COPD group compared with the non-COPD group (adjusted odds ratio, 1.89; 95% confidence interval, 1.18–2.95), which was especially significant in subjects with FEV1 less than the median value (< 110%pred) (Pinteraction = 0.017) and inactive physical activity (Pinteraction = 0.039). In conclusion, the risk of rapid FEV1 decline was higher in young adults with COPD than in those without COPD, especially in those with FEV1 less than the median value and inactive physical activity.
Go to : 
Graphical Abstract
Go to : 
Important factors deteriorating the natural course of chronic obstructive pulmonary disease (COPD) include early onset of the disease, rapid decline of lung function, and acute exacerbation of COPD.1 Regarding the importance of early onset of the disease, several recent studies have evaluated the development of COPD in young populations and its clinical significance, including acute exacerbation of COPD.23 However, few studies evaluated whether young adults with COPD are at a higher risk of rapid lung function decline compared to those without COPD. Thus, we aimed to evaluate the risk of rapid forced expiratory volume in 1 second (FEV1) decline in young adults with COPD.
The Ansan-Anseong cohort is a prospective ongoing observational cohort of Korea since 2001 to investigate factors associated with chronic diseases.4 The subjects’ baseline data were measured between May 2001 and February 2003, and the measurement of subsequent lung function was performed biennially thereafter. Ten-year follow-up data of adults aged 40–49 were obtained for this study.
Of 4,711 subjects, 212 who had missing values at baseline measurements and 66 who were previously diagnosed with asthma were excluded. We further excluded 978 subjects who were tested for additional lung function less than twice. Considering selection bias caused by a relatively large number of excluded subjects, we used 1:3 propensity score matching between excluded subjects (n = 978) and remaining subjects (n = 3,455) to establish a final analytic cohort for this study (n = 2,934). Of these, 179 (6.1%) had COPD.
COPD was defined as pre-bronchodilator FEV1/forced vital capacity (FVC) < lower limit of normal (LLN).5 Considering that Asian populations include a substantial number of never smokers with COPD, a smoking criterion was not used to define COPD.67 The outcome of the study was a rapid decline in FEV1, defined as ≥ 60 mL/year.8 This criterion was proposed by the Martinez research group8 and has been validated in several high-quality studies.910 Individual logistic regression analysis was performed for calculating annual changes in FEV1, and annual changes in FEV1 were determined using regression coefficients.
Trained investigators assessed subjects’ socioeconomic status, lifestyle habits, occupational exposure, and respiratory symptoms. Low income was classified as the lowest quartile. Active physical activity was defined as 60 min/day of moderate activity or 30 min/day of vigorous activity.11 Occupational exposure was defined in participants who had chemical or dust exposure using self-questionnaires. Hypertension was defined as a previous diagnosis of hypertension, systolic blood pressure >140 mmHg, or diastolic blood pressure > 90 mmHg. The presence of any respiratory symptoms was determined when participants had any of the following symptoms: dyspnea, chronic cough, or chronic sputum. Dyspnea was defined as a response to the question, ‘Do you feel shortness of breath when walking on plain ground?’. Chronic cough was defined as cough lasting three months or longer in recent months. Chronic sputum was defined as sputum production accompanied by cough for at least three months a year.
Multivariable logistic regression analysis adjusting for age, sex, body mass index (BMI), smoking status, occupational exposure, low income, college graduate, physical activity, respiratory symptom, baseline FEV1%pred, and hypertension was used for the analysis of the risk of rapid decline in FEV1. Subgroup analyses were performed on clinically significant variables (sex, smoking status, BMI, occupational exposure, baseline FEV1, and physical activity), and the cut-off value for subgroup analysis was determined as a median in BMI (24 kg/m2) and baseline FEV1 (110%pred). Although the Global Initiative for Chronic Obstructive Lung Disease guideline suggests a cut-off for moderate severity as an 80%pred of FEV1, this value does not apply to young adults with COPD because most people with airflow limitation had a mild degree of COPD (97.8%). Thus, we used the median value for subgroup analysis and plotted a survival probability for rapid FEV1 decline using the ‘predicted’ package of R. All analyses were performed using R version 4.1.2 (R core Team 2021; R Foundation for Statistical Computing, Vienna, Austria).
Of 2,934 adults aged 40–49, the median age was 44 (interquartile range [IQR], 42–46 years), and 48.5% were male. The median value of FVC, FEV1, and FEV1/FVC was 103%pred (IQR, 95–111%pred), 110%pred (IQR, 101–120%pred), and 83% (IQR, 79–86%), respectively.
Compared to the non-COPD group, the proportion of men (56.4% vs. 48.0%, P = 0.035), current or past smokers (54.2% vs. 43.4%, P = 0.006), low-income (45.3% vs. 30.3%, P < 0.001), active physical activity (62.0% vs. 43.0%, P < 0.001), and respiratory symptoms (12.8% vs. 7.4%, P = 0.012) were higher, but college graduate (12.3% vs. 20.2%, P = 0.013) was lower in the COPD group. Regarding baseline lung function, the COPD group had higher FVC (106 [99–116]%pred vs. 103 [95–111]%pred, P < 0.001) but lower FEV1 (96 [88–104]%pred vs. 111 [102–121]%pred, P < 0.001) and FEV1/FVC (70 [67–72]% vs. 83 [80–86]%, P < 0.001) than the non-COPD group.
During the median 9.7 (IQR, 7.9–9.8) years of follow-up, the incidence of rapid decline in FEV1 was not different between the non-COPD and COPD groups (15.5% vs. 17.9%, P = 0.404). However, among physically inactive subjects (20.6% vs. 12.0%, P = 0.034) and those with FEV1 < 110%pred (17.8% vs. 9.1%, P < 0.001), the proportion of rapid FEV1 decline was significantly higher in the COPD group than the non-COPD group (Fig. 1A).
In the multivariable model, a significantly higher risk of rapid decline in FEV1 was observed for the COPD group compared with the non-COPD group (adjusted odds ratio [aOR], 1.89; 95% confidence interval [CI], 1.18–2.95). The results of subgroup analyses showed a significantly increased risk of rapid decline in FEV1 in males (aOR, 2.15; 95% CI, 1.27–3.57), current or past smokers (aOR, 2.19; 95% CI, 1.28–3.69), high BMI (≥ 24 kg/m2) (aOR, 2.87; 95% CI, 1.55–5.16), those who had occupational exposure (aOR, 1.89; 95% CI, 1.18–2.94), FEV1 less than the median value (< 110%pred) (aOR, 2.22; 95% CI, 1.30–3.72), and physical inactivity (aOR, 3.22; 95% CI, 1.58–6.22). Of these variables, significant interaction effects were found in baseline FEV1%pred (Pinteraction = 0.017) and active physical activity (Pinteraction = 0.039) (Fig. 1B).
The previously proposed lung function trajectories leading to the development of COPD were low maximal FEV1 or normal FEV1 with rapid decline.12 Among these, COPD in young adults, defined as LLN, appears to be a small lung type, i.e., low maximal FEV1.13 However, our findings showed that young adults with COPD were not only a small lung type but also at a higher risk of rapid decline in FEV1. Therefore, our study suggests that the LLN criterion includes the concept of rapid decline and can be suitable for defining COPD in young adults.
Interestingly, our study showed a significant interaction between rapid FEV1 decline and physical activity or baseline FEV1%pred. Although the mechanisms are not precise, there are some possible explanations. First, sedentary behavior was suggested as a risk factor for the rapid decline in lung function.141516 Second, FEV1 less than the median value, which reflects the severity of COPD, is associated with more frequent respiratory symptoms and common exacerbations, known risk factors for the rapid decline in lung function.3 In summary, special attention should be paid to rapid lung function decline in young adults with COPD who have FEV1 less than the median value with a sedentary lifestyle.
Our study has some strengths. First, our findings were based on a large-scale, long-term prospective cohort. Second, possible bias was reduced as much as possible by using several statistical methods. Nevertheless, the limitations of this study should be addressed. First, pre-bronchodilator measurement was used to define COPD in young adults instead of post-bronchodilator measurement. However, between pre-and post-bronchodilator parameters, there is a debate with regard to which is optimal for determining COPD in young adults.17 Second, an evaluation of adults younger than 40 years was not performed in this study. However, previous studies including adults in their 20s and 30s reported that most young adults with COPD were in their 40s.18 Third, we used the median value as a cut-off value of baseline FEV1 arbitrarily in this study, since there is no known cut-off value of FEV1 in young adults with COPD. Fourth, as a local cohort was used, the subjects in this cohort might not represent the entire population of patients with COPD.
In conclusion, the risk of rapid FEV1 decline was higher in young adults with COPD than in those without COPD, especially in those with FEV1 less than median value and inactive physical activity.
This study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of Konkuk University Medical Center (IRB No. KUMC2022-03-032). Informed consent was waived because only de-identified database entries were accessed for analytical purposes.
Go to : 
ACKNOWLEDGMENTS
Data utilized in this study were obtained from the Korean Genome and Epidemiology Study (KoGES; 4851-302), National Research Institute of Health, Centers for Disease Control and Prevention, Ministry for Health and Welfare, Republic of Korea.
Go to : 
Notes
Data Availability Statement: The data used in our study are fully available upon reasonable request.
Go to : 
References
1. Marott JL, Ingebrigtsen TS, Çolak Y, Vestbo J, Lange P. Lung function trajectories leading to chronic obstructive pulmonary disease as predictors of exacerbations and mortality. Am J Respir Crit Care Med. 2020; 202(2):210–218. PMID: 32289231.
2. Soriano JB, Polverino F, Cosio BG. What is early COPD and why is it important? Eur Respir J. 2018; 52(6):1801448. PMID: 30309976.
3. Kalhan R, Dransfield MT, Colangelo LA, Cuttica MJ, Jacobs DR Jr, Thyagarajan B, et al. Respiratory symptoms in young adults and future lung disease. The CARDIA lung study. Am J Respir Crit Care Med. 2018; 197(12):1616–1624. PMID: 29369684.
4. Kim Y, Han BG. KoGES group. Cohort profile: the Korean Genome and Epidemiology Study (KoGES) Consortium. Int J Epidemiol. 2017; 46(2):e20. PMID: 27085081.
5. Hwang YI, Kim CH, Kang HR, Shin T, Park SM, Jang SH, et al. Comparison of the prevalence of chronic obstructive pulmonary disease diagnosed by lower limit of normal and fixed ratio criteria. J Korean Med Sci. 2009; 24(4):621–626. PMID: 19654942.
6. Park HY, Kang D, Shin SH, Yoo KH, Rhee CK, Suh GY, et al. Chronic obstructive pulmonary disease and lung cancer incidence in never smokers: a cohort study. Thorax. 2020; 75(6):506–509. PMID: 32241883.
7. Lee HW, Sim YS, Jung JY, Seo H, Park JW, Min KH, et al. A multicenter study to identify the respiratory pathogens associated with exacerbation of chronic obstructive pulmonary disease in Korea. Tuberc Respir Dis. 2022; 85(1):37–46.
8. Martinez FJ, Han MK, Allinson JP, Barr RG, Boucher RC, Calverley PM, et al. At the root: defining and halting progression of early chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018; 197(12):1540–1551. PMID: 29406779.
9. Çolak Y, Afzal S, Nordestgaard BG, Lange P, Vestbo J. Importance of early COPD in young adults for development of clinical COPD: findings from the Copenhagen General Population Study. Am J Respir Crit Care Med. 2021; 203(10):1245–1256. PMID: 33142077.
10. Lee HW, Lee HJ, Lee JK, Park TY, Heo EY, Kim DK. Rapid FEV1 decline and lung cancer incidence in South Korea. Chest. 2022; 162(2):466–474. PMID: 35318007.
11. Yang YJ. An overview of current physical activity recommendations in primary care. Korean J Fam Med. 2019; 40(3):135–142. PMID: 31122003.
12. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for prevention, diagnosis and management of COPD. Updated 2021. Accessed December 20, 2021.
https://goldcopd.org/2022-gold-reports/
.
13. Papi A, Beghé B, Fabbri LM. Rate of decline of FEV1 as a biomarker of survival? Am J Respir Crit Care Med. 2021; 203(6):663–665. PMID: 33095996.
14. Garcia-Aymerich J, Lange P, Benet M, Schnohr P, Antó JM. Regular physical activity modifies smoking-related lung function decline and reduces risk of chronic obstructive pulmonary disease: a population-based cohort study. Am J Respir Crit Care Med. 2007; 175(5):458–463. PMID: 17158282.
15. Spruit MA, Pitta F, McAuley E, ZuWallack RL, Nici L. Pulmonary rehabilitation and physical activity in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015; 192(8):924–933. PMID: 26161676.
16. Rehman AU, Shah S, Abbas G, Harun SN, Shakeel S, Hussain R, et al. Assessment of risk factors responsible for rapid deterioration of lung function over a period of one year in patients with chronic obstructive pulmonary disease. Sci Rep. 2021; 11(1):13578. PMID: 34193949.
17. Brown LK, Miller A. Spirometric indices of early airflow impairment in individuals at risk of developing COPD: spirometry beyond FEV1/FVC. Respir Med. 2021; 176:105921. PMID: 33589144.
18. Çolak Y, Afzal S, Nordestgaard BG, Vestbo J, Lange P. Prevalence, characteristics, and prognosis of early chronic obstructive pulmonary disease. The Copenhagen General Population Study. Am J Respir Crit Care Med. 2020; 201(6):671–680. PMID: 31770495.
Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download