1. National Institute of Dementia. National Institute of Dementia Annual Report 2017. Seongnam, Korea: National Institute of Dementia;2018.
2. Choi YJ, Kim S, Hwang YJ, Kim C. Prevalence of dementia in korea based on hospital utilization data from 2008 to 2016. Yonsei Med J. 2021; 62(10):948–953. PMID:
34558875.
3. Ministry of Health and Welfare. Nationwide Survey on the Dementia Epidemiology of Korea 2012. Seongnam, Korea: Seoul National University Bundang Hospital;2012.
4. Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020; 396(10248):413–446. PMID:
32738937.
5. Arntzen KA, Schirmer H, Wilsgaard T, Mathiesen EB. Impact of cardiovascular risk factors on cognitive function: the Tromsø study. Eur J Neurol. 2011; 18(5):737–743. PMID:
21143340.
6. Han JY, Han SH. Primary prevention of Alzheimer’s disease: is it an attainable goal? J Korean Med Sci. 2014; 29(7):886–892. PMID:
25045219.
7. Schofield JD, Liu Y, Rao-Balakrishna P, Malik RA, Soran H. Diabetes dyslipidemia. Diabetes Ther. 2016; 7(2):203–219. PMID:
27056202.
8. Dalal JJ, Padmanabhan TN, Jain P, Patil S, Vasnawala H, Gulati A. LIPITENSION: Interplay between dyslipidemia and hypertension. Indian J Endocrinol Metab. 2012; 16(2):240–245. PMID:
22470861.
9. Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998; 97(18):1837–1847. PMID:
9603539.
10. Song R, Xu H, Dintica CS, Pan KY, Qi X, Buchman AS, et al. Associations between cardiovascular risk, structural brain changes, and cognitive decline. J Am Coll Cardiol. 2020; 75(20):2525–2534. PMID:
32439001.
11. Zeki Al Hazzouri A, Haan MN, Neuhaus JM, Pletcher M, Peralta CA, López L, et al. Cardiovascular risk score, cognitive decline, and dementia in older Mexican Americans: the role of sex and education. J Am Heart Assoc. 2013; 2(2):e004978. PMID:
23608609.
12. Kaffashian S, Dugravot A, Nabi H, Batty GD, Brunner E, Kivimäki M, et al. Predictive utility of the Framingham general cardiovascular disease risk profile for cognitive function: evidence from the Whitehall II study. Eur Heart J. 2011; 32(18):2326–2332. PMID:
21606085.
13. Wang R, Fratiglioni L, Kalpouzos G, Lövdén M, Laukka EJ, Bronge L, et al. Mixed brain lesions mediate the association between cardiovascular risk burden and cognitive decline in old age: a population-based study. Alzheimers Dement. 2017; 13(3):247–256. PMID:
27521789.
14. Iadecola C, Parikh NS. Framingham general cardiovascular risk score and cognitive impairment: the power of foresight. J Am Coll Cardiol. 2020; 75(20):2535–2537. PMID:
32439002.
15. Kaffashian S, Dugravot A, Elbaz A, Shipley MJ, Sabia S, Kivimäki M, et al. Predicting cognitive decline: a dementia risk score vs. the Framingham vascular risk scores. Neurology. 2013; 80(14):1300–1306. PMID:
23547265.
16. Viticchi G, Falsetti L, Buratti L, Boria C, Luzzi S, Bartolini M, et al. Framingham risk score can predict cognitive decline progression in Alzheimer’s disease. Neurobiol Aging. 2015; 36(11):2940–2945. PMID:
26279114.
17. Viticchi G, Falsetti L, Buratti L, Sajeva G, Luzzi S, Bartolini M, et al. Framingham risk score and the risk of progression from mild cognitive impairment to dementia. J Alzheimers Dis. 2017; 59(1):67–75. PMID:
28582863.
18. Lee I, Kang H. Association of cardiovascular disease risk and physical fitness with cognitive impairment in Korean elderly women. Korean J Sports Med. 2021; 39(2):51–59.
19. D’Agostino RB Sr, Grundy S, Sullivan LM, Wilson P. CHD Risk Prediction Group. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001; 286(2):180–187. PMID:
11448281.
20. Ahn KA, Yun JE, Cho ER, Nam CM, Jang YS, Jee SH. Framingham equation model overestimates risk of ischemic heart disease in Korean men and women. Korean J Epidemiol. 2006; 28(2):162–170.
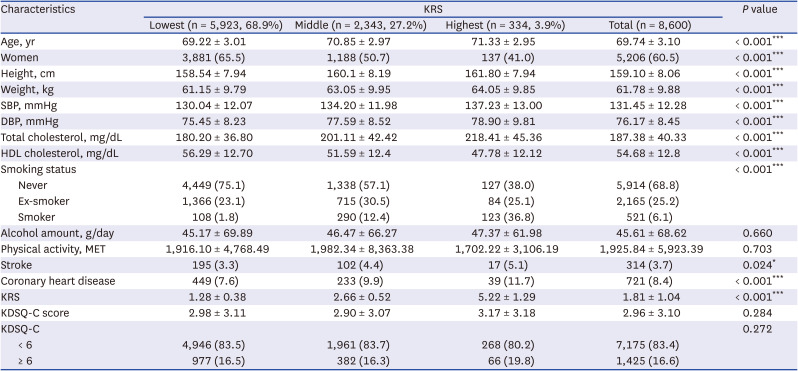
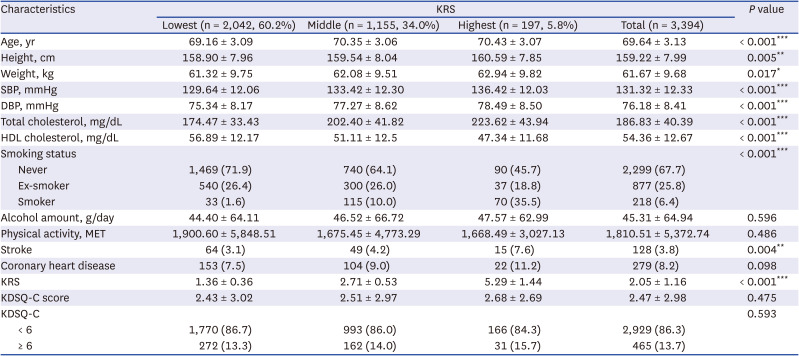
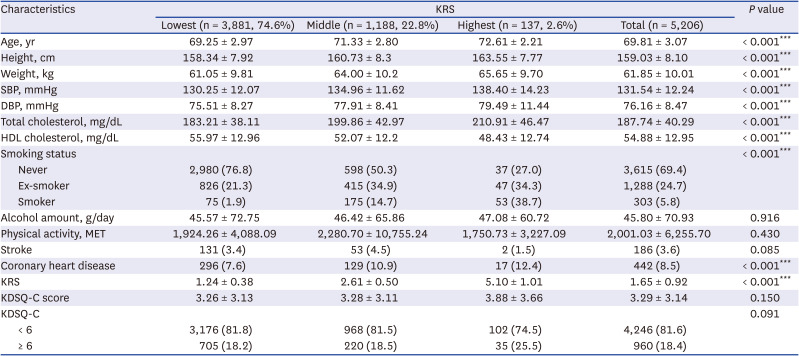
21. Jee SH, Jang Y, Oh DJ, Oh BH, Lee SH, Park SW, et al. A coronary heart disease prediction model: the Korean Heart Study. BMJ Open. 2014; 4(5):e005025.
22. World Health Organization (WHO). International Guide for Monitoring Alcohol Consumption and Related Harm. Geneva, Switzerland: WHO;2000.
23. Chun MY. Validity and reliability of Korean version of international physical activity questionnaire short form in the elderly. Korean J Fam Med. 2012; 33(3):144–151. PMID:
22787536.
24. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003; 42(6):1206–1252. PMID:
14656957.
25. Jee SH. Metabolic syndrome in women: what’s the difference between men and women. In : Proceedings of the Korean Cardiology-Related Societies Joint Scientific Session; 2010 Apr 16-17; Busan, Korea. Seoul, Korea: Korean Society of Cardiology;2010.
26. Kim A, Kim S, Park KW, Park KH, Youn YC, Lee DW, et al. A comparative evaluation of the KDSQ-C, AD8, and SMCQ as a cognitive screening test to be used in national medical check-ups in Korea. J Korean Med Sci. 2019; 34(14):e111. PMID:
30977313.
27. Yang DW, Cho B, Chey JY, Kim SY, Kim BS. The development and validation of Korean Dementia Screening Questionnaire (KDSQ). J Korean Neurol Assoc. 2002; 20(2):11–12.
28. Mitnitski A, Skoog I, Song X, Waern M, Ostling S, Sundh V, et al. A vascular risk factor index in relation to mortality and incident dementia. Eur J Neurol. 2006; 13(5):514–521. PMID:
16722978.
29. Oh HM, Kim SH, Kang SG, Park SJ, Song SW. The relationship between metabolic syndrome and cognitive function. Korean J Fam Med. 2011; 32(6):358–366. PMID:
22745874.
30. Mun SH, Oh HJ, Kim SH, Lee HR, Lee DC, Shim JY. Relationship between the Metabolic syndrome and cognitive function. Korean J Fam Med. 2006; 27(6):463–470.
31. Rabin JS, Schultz AP, Hedden T, Viswanathan A, Marshall GA, Kilpatrick E, et al. Interactive associations of vascular risk and β-amyloid burden with cognitive decline in clinically normal elderly individuals findings from the Harvard Aging Brain Study. JAMA Neurol. 2018; 75(9):1124–1131. PMID:
29799986.
32. Sisante JV, Vidoni ED, Kirkendoll K, Ward J, Liu Y, Kwapiszeski S, et al. Blunted cerebrovascular response is associated with elevated beta-amyloid. J Cereb Blood Flow Metab. 2019; 39(1):89–96. PMID:
28914134.
33. Qiu C, Fratiglioni L. A major role for cardiovascular burden in age-related cognitive decline. Nat Rev Cardiol. 2015; 12(5):267–277. PMID:
25583619.
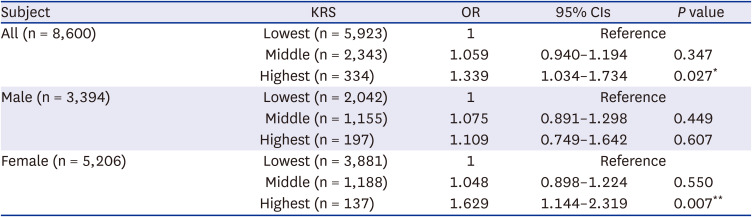
34. Laughlin GA, McEvoy LK, von Mühlen D, Daniels LB, Kritz-Silverstein D, Bergstrom J, et al. Sex differences in the association of Framingham Cardiac Risk Score with cognitive decline in community-dwelling elders without clinical heart disease. Psychosom Med. 2011; 73(8):683–689. PMID:
21949428.
35. Lyu J, Kim HY. Gender-specific incidence and predictors of cognitive impairment among older Koreans: findings from a 6-year prospective cohort study. Psychiatry Investig. 2016; 13(5):473–479.
36. Lee HJ, Joo YH, Han KD, Park KH. Association between hearing loss and cognitive disorder: a nationwide population-based study. Yonsei Med J. 2021; 62(5):446–452. PMID:
33908216.
37. Hua W, Hou J, Jiang T, Su B, Fu J, Sun R, et al. The longitudinal association between cardiovascular risk and cognitive function in middle-aged and older adults in China: a nationally representative cohort study. Front Cardiovasc Med. 2020; 7:560947. PMID:
33195454.
38. Zhou Z, Ryan J, Ernst ME, Zoungas S, Tonkin AM, Woods RL, et al. Effect of statin therapy on cognitive decline and incident dementia in older adults. J Am Coll Cardiol. 2021; 77(25):3145–3156. PMID:
34167639.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download