1. World Health Organization. Guidelines for Trauma Quality Improvement Programmes. Geneva, Switzerland: WHO Press;2009.
2. World Health Organization. The Global Burden of Disease. Geneva, Switzerland: WHO Press;2008.
4. Korean Statistical Information Service. Leading Causes of Death Reports 1983–2019. Seoul, Korea: Korean Statistical Information Service;2020.
5. Coccolini F, Kluger Y, Moore EE, Maier RV, Coimbra R, Ordoñez C, et al. Trauma quality indicators: internationally approved core factors for trauma management quality evaluation. World J Emerg Surg. 2021; 16(1):6. PMID:
33622373.
6. Cales RH, Trunkey DD. Preventable trauma deaths. A review of trauma care systems development. JAMA. 1985; 254(8):1059–1063. PMID:
3894708.
7. MacKenzie EJ. Review of evidence regarding trauma system effectiveness resulting from panel studies. J Trauma. 1999; 47(3):Suppl. S34–S41. PMID:
10496608.
8. Jung KY, Kim JS, Kim Y. Problems in trauma care and preventable deaths. J Korean Soc Emerg Med. 2001; 12(1):45–56.
9. Kim H, Jung KY, Kim SP, Kim SH, Noh H, Jang HY, et al. Changes in preventable death rates and traumatic care systems in Korea. J Korean Soc Emerg Med. 2012; 23(2):189–197.
10. Yoon HD. Background and progress of regional trauma center development. J Korean Med Assoc. 2016; 59(12):919–922.
11. Park DJ, Park CY, Cho HM, Lee KH, Han H. Current status and future prospects of trauma centers in Korea. J Korean Med Assoc. 2017; 60(7):530–532.
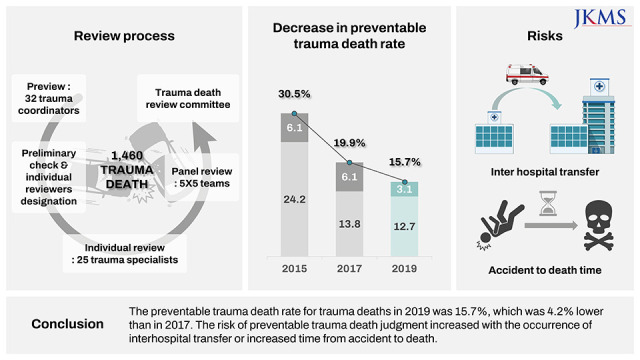
12. Jung K, Kim I, Park SK, Cho H, Park CY, Yun JH, et al. Preventable trauma death rate after establishing a national trauma system in Korea. J Korean Med Sci. 2019; 34(8):e65. PMID:
30833882.
13. Kim Y, Jung KY, Cho KH, Kim H, Ahn HC, Oh SH, et al. Preventable trauma deaths rates and management errors in emergency medical system in Korea. J Korean Soc Emerg Med. 2006; 17(5):385–394.
14. Jung K, Kwon J, Huh Y, Moon J, Hwang K, Cho HM, et al. National trauma system establishment based on implementation of regional trauma centers improves outcomes of trauma care: a follow-up observational study in South Korea. PLOS Glob Public Health. 2022; 2(1):e0000162.
17. Sanddal TL, Esposito TJ, Whitney JR, Hartford D, Taillac PP, Mann NC, et al. Analysis of preventable trauma deaths and opportunities for trauma care improvement in utah. J Trauma. 2011; 70(4):970–977. PMID:
21206286.
18. Teixeira PG, Inaba K, Hadjizacharia P, Brown C, Salim A, Rhee P, et al. Preventable or potentially preventable mortality at a mature trauma center. J Trauma. 2007; 63(6):1338–1346. PMID:
18212658.
19. National Academies of Sciences, Engineering, and Medicine. A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury. Washington, D.C., USA: National Academies Press;2016.
20. Pigula FA, Wald SL, Shackford SR, Vane DW. The effect of hypotension and hypoxia on children with severe head injuries. J Pediatr Surg. 1993; 28(3):310–314. PMID:
8468638.
21. Sampalis JS, Denis R, Fréchette P, Brown R, Fleiszer D, Mulder D. Direct transport to tertiary trauma centers versus transfer from lower level facilities: impact on mortality and morbidity among patients with major trauma. J Trauma. 1997; 43(2):288–295. PMID:
9291375.
22. Young JS, Bassam D, Cephas GA, Brady WJ, Butler K, Pomphrey M. Interhospital versus direct scene transfer of major trauma patients in a rural trauma system. Am Surg. 1998; 64(1):88–91. PMID:
9457044.
23. Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, et al. Guidelines for the management of severe traumatic brain injury. VIII. Intracranial pressure thresholds. J Neurotrauma. 2007; 24(Suppl 1):S55–S58. PMID:
17511546.
24. Huh Y, Kwon J, Moon J, Kang BH, Kim S, Yoo J, et al. An evaluation of the effect of performance improvement and patient safety program implemented in a new regional trauma center of Korea. J Korean Med Sci. 2021; 36(22):e149. PMID:
34100561.
25. Kwon J, Lee JH, Hwang K, Heo Y, Cho HJ, Lee JC, et al. Systematic preventable trauma death rate survey to establish the region-based inclusive trauma system in a representative province of Korea. J Korean Med Sci. 2020; 35(50):e417–e420. PMID:
33372420.
26. MacKenzie EJ. Review of evidence regarding trauma system effectiveness resulting from panel studies. J Trauma. 1999; 47(3):Suppl. S34–S41. PMID:
10496608.
27. West JG. Validation of autopsy method for evaluating trauma care. Arch Surg. 1982; 117(8):1033–1035. PMID:
7103721.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download