It is well documented that the third-dose coronavirus disease 2019 (COVID-19) vaccination effectively reduces the incidence, hospitalization rates, and fatality rates.
123 While most studies focus on the effectiveness of vaccines at the individual level, this study focuses on the ecological association between regional case fatality rates (CFRs) and COVID-19 vaccination coverage, especially after the third-dose was administered in South Korea.
South Korea had successfully contained the earlier COVID-19 waves via the control measures, including the Test, Trace/isolate, Treat (3T) strategy and social distancing until it reached a high vaccination rate.
4 A total of 96.4% of the adult population (≥ 18 years of age) completed primary doses, and 74.1% of those completed a booster dose by April 20, 2022.
5 One booster via either mRNA vaccine, BNT162 or mRNA-1273, has been available to all adults since December 4, 2021 (information on vaccine products offered is available in
Supplementary Table 1).
The omicron variant of SARS-CoV-2 became dominant in mid-January 2022 in South Korea. The cumulative number of confirmed COVID-19 individuals increased from approximately 0.7 million as of mid-January 2022 to 16.5 million as of mid-April 2022, accounting for 1.3% and 31.9% of the total population, respectively.
6 Despite the surge of omicron variant, South Korea’s cumulative CFR remained as low as 0.13%, which is far below that of the United States (1.23%), India (1.21%), the United Kingdom (0.78%), or Germany (0.56%).
7 Since the infected population by earlier variants had been small (< 2%), the low CFR in Korea would be largely explained by vaccine-induced immunity against omicron rather than natural immunity.
In this paper, we evaluated the population-level impact of third-dose vaccination coverage by documenting the association between CFRs and vaccination rates in 244 counties (si/gun/gu) of South Korea. This activity was reviewed by Centers for Disease Control and Prevention (CDC) and was conducted consistent with applicable federal law and CDC policy (45 Code of Federal Regulations [C.F.R.] part 46, 21 C.F.R. part 56; 42 United States Code [U.S.C.] Sect. 241[d]; 5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.). The main empirical specification of our multivariate regression analyses is as below:
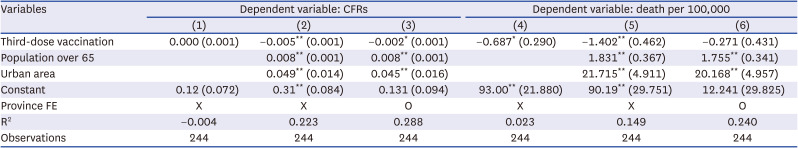
The dependent variable, county-level CFRs (
CFRc), were calculated using cumulative confirmed cases and deaths reported by each county. The CFRs vary between 0.01% and 0.69% by county (
Fig. 1A). The third-dose vaccination rates among the population aged ≥ 12 years (
Vc) were included as a main explanatory variable. County-level vaccination rates range from 60% to 92% (
Fig. 1B). The share of the population aged ≥ 65 years (
Sc) is included as another explanatory variable. The county with a higher proportion of the elderly may have higher CFRs than others because age is one of the strongest predictors of COVID-19 mortality. By including
Sc in the regression, we could check whether the booster dose still reduces CFRs after controlling for the age distribution. In addition, city dummy (
Cc) is included to see whether there are urban-rural disparities in CFRs. As urban areas tend to have better access to medical services in South Korea, they may have lower CFRs than rural areas.
8
α is a constant,
β and
γ are regression coefficients and
εc is an error term. Descriptive statistics for all variables can be found in
Supplementary Table 2.
Fig. 1
The county-level case fatality rates (A) and third-dose vaccination coverage (B) for COVID-19 in South Korea.

Additionally, the province fixed effects (
p: FEs) were included to capture the characteristics of 17 provinces (s
i/
do; upper administrative division of county) that may explain the variations in county-level CFRs. For example, COVID-19 mortality could be alleviated if a region has better medical capacity, such as more beds or medical staff per capita and proximity to intensive care units (ICU) specializing in infectious respiratory diseases.
9 In Korea, differences in medical capacity are often determined at the province level rather than the county level.
1011 Also, mortality would decrease if the incidence itself is lowered by non-pharmaceutical interventions (NPIs), which have been differently applied and complied by province in Korea.
1213 On July 15, 2021, for example, the strictest social distancing (Level 4) was applied to Seoul, Gyeonggi, and Incheon, but the levels varied in other provinces: Level 3 for 1 province; Level 3 for 9 provinces; Level 1 for 4 provinces.
14 Thus, the outcome in a county is affected by the capability of the province it belongs to, which would be captured by province FEs. Province fixed effects were inserted in the form of province dummies, with Daejeon, which has a median CFR, as a reference.
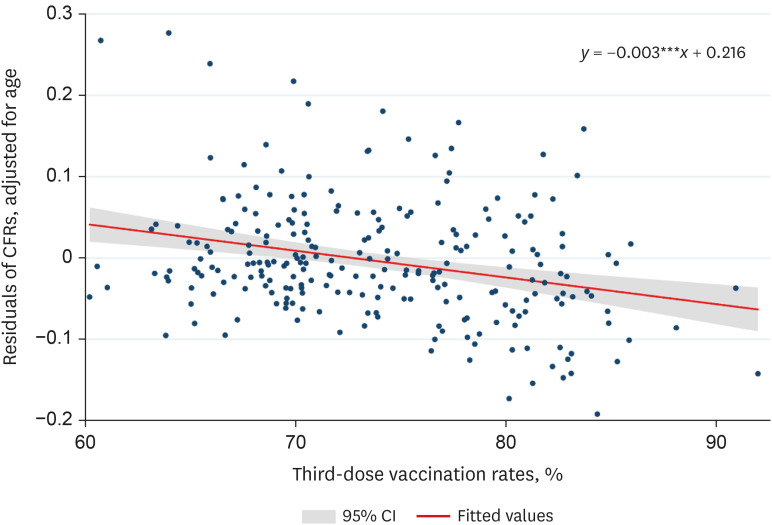
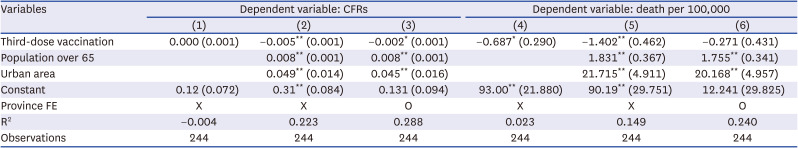
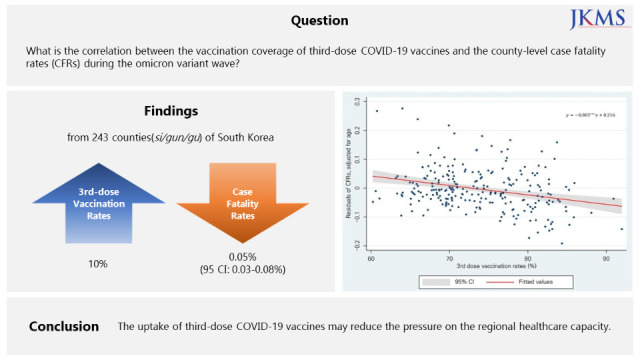
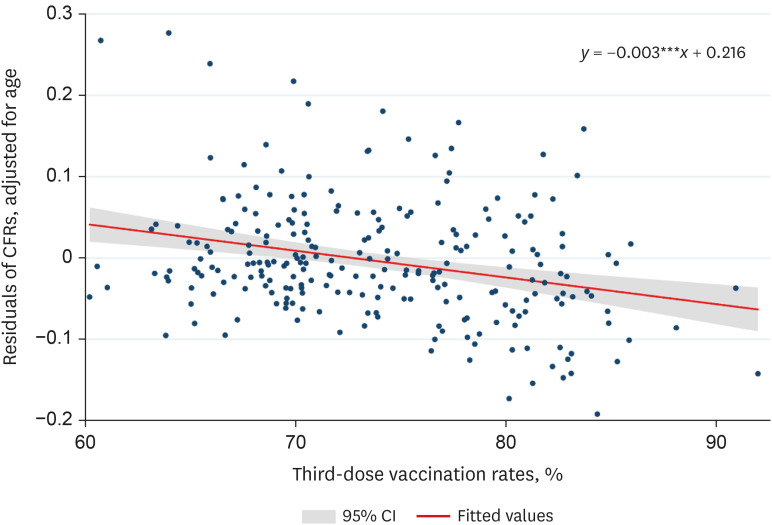
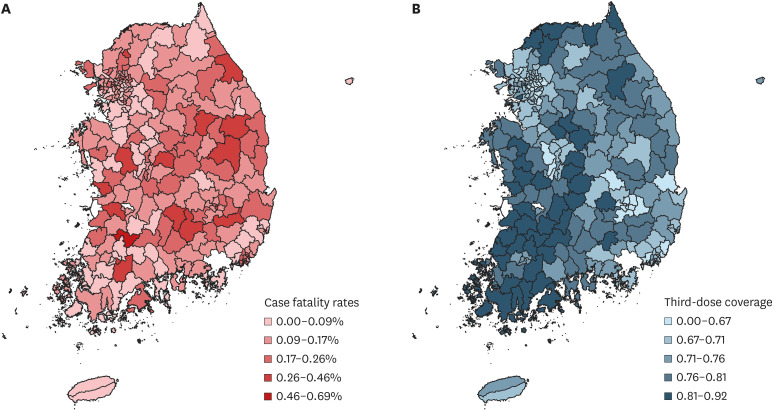
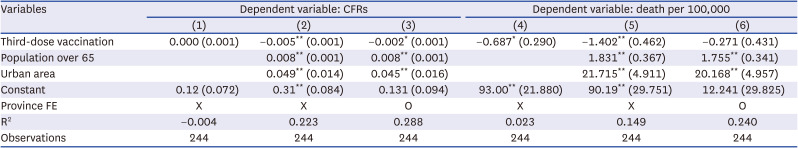
Columns 1, 2, and 3 of
Table 1 report the regression coefficients and robust standard error. The third-dose vaccination rates were not significant when included alone (column 1). This result seems intuitive as booster doses were mainly administered to the elderly population, and higher rates of third-dose vaccination meant that the share of the elderly was also high. When controlling for age, however, the regression coefficient of vaccination rates turned significant and negative, indicating that the higher third-dose vaccination rate was correlated with lower regional CFRs (column 2). For example, if the third-dose vaccination rate of a county is higher by 10%, it would have a CFR lower by 0.05% (95% confidence interval, 0.03–0.08%). As the number of cumulative confirmed cases in South Korea was 16,353,495 as of April 20, 2022, a lower CFR by 0.03–0.08% is equivalent to 4,394–12,448 lives (8.6–24.4 per 100,000) spared. This correlation is also shown in
Fig. 2. In addition, city dummy has a positive and significant coefficient, which implies that urban areas had lower CFRs than rural areas, as predicted. When the province FEs are included, the coefficient on the third-dose vaccination is still negative and significant (column 3). The magnitudes of coefficient and significance decrease by a small margin, which indicates that CFRs are likely affected by province-level characteristics such as medical capacity.
Fig. 2
Correlation between CFRs (age distribution controlled) and the third-dose vaccination rates during omicron wave in South Korea.
CFR = case fatality rate.
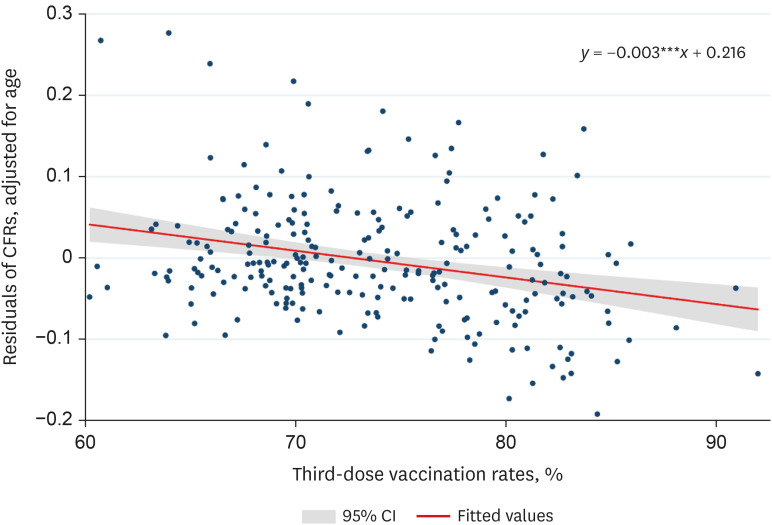

Table 1
Main regression results: third-dose vaccination and COVID-19 mortality
|
Variables |
Dependent variable: CFRs |
Dependent variable: death per 100,000 |
|
(1) |
(2) |
(3) |
(4) |
(5) |
(6) |
|
Third-dose vaccination |
0.000 (0.001) |
−0.005** (0.001) |
−0.002* (0.001) |
−0.687* (0.290) |
−1.402** (0.462) |
−0.271 (0.431) |
|
Population over 65 |
|
0.008** (0.001) |
0.008** (0.001) |
|
1.831** (0.367) |
1.755** (0.341) |
|
Urban area |
|
0.049** (0.014) |
0.045** (0.016) |
|
21.715** (4.911) |
20.168** (4.957) |
|
Constant |
0.12 (0.072) |
0.31** (0.084) |
0.131 (0.094) |
93.00** (21.880) |
90.19** (29.751) |
12.241 (29.825) |
|
Province FE |
X |
X |
O |
X |
X |
O |
|
R2
|
−0.004 |
0.223 |
0.288 |
0.023 |
0.149 |
0.240 |
|
Observations |
244 |
244 |
244 |
244 |
244 |
244 |

For a brief robustness check, the dependent variable was replaced with deaths per 100,000 (columns 4, 5, and 6 of
Table 1). Vaccination rates are still associated with reduced mortality after controlling for age (column 5), but province-specific characteristics seemed to override the effect of booster dose uptake (column 6). This is potentially because COVID-19 mortality rates, unlike CFRs, increase along with the incidence rates of a county, which is influenced by province-specific characteristics such as variations in NPIs.
For another robustness check, the main independent variable, third-dose vaccine uptake, is replaced with the share of those who are fully vaccinated by two doses (
Supplementary Table 3). Coefficients on full vaccination are negative and significant in most of the specifications, but the magnitude and significance of regression coefficients reduced compared to third-dose vaccination. This means that two-dose primary vaccination may have alleviated the burden on the local healthcare system to some extent, but not as much as the booster dose did.
Our findings indicate that the uptake of third-dose COVID-19 vaccines is negatively correlated with CFRs during the period of the omicron wave in South Korea. Exploring regional variations in third-dose vaccination coverage and CFRs of South Korea has several merits as 1) immunity by natural infection was negligibly low (< 2%), 2) primary and booster vaccination rates became substantially high before the omicron surge, and 3) it has a centralized system for diagnosis, treatment, and data collection, which leaves little margin of error for regional comparison. Based on this unique setting, our study not only highlights the effectiveness of third-dose vaccination as previous studies did,
12315 but also provides a rough estimate of the spared lives associated with vaccines.
The present study is subject to some limitations. First, we did not establish a causal link between booster dose and CFRs. There is a possibility of reverse causality, as people would be more willing to get vaccinated when they see increasing death by COVID-19 in their neighborhood. Second, our results may be subject to some unobserved variables affecting both vaccine uptake and COVID-19 mortality, such as compliance with government policies. The province FEs may correct this biasedness to some extent, but relatively low R2’s (0.24–0.29) indicate some variables could have been omitted. Third, we did not consider the effect of treatments such as Paxlovid (Pfizer Inc., New York, NY, USA) and Lagevrio (MSD, Kenilworth, NJ, USA), which have been prescribed since mid-January and mid-March 2022, respectively, in South Korea. As the availability of effective treatments enhances the chance of surviving for COVID-19 patients, their allocation mechanism may affect regional outcome.
Despite these limitations, our ecological study demonstrated the extent of the regional variations in COVID-19 fatality associated with vaccination coverage. It also shows the possibility that the vaccine effect interacts with other county-specific characteristics including ICU availability and NPIs, as well as the share of the elderly population, which needs further investigation in the future.
Ethics statement
The datasets used in the study were de-identified and fully anonymized in advance, and the analysis of publicly available data without identity information does not require ethical approval.