INTRODUCTION
Renal trauma is common in the urinary tract region. Renal trauma accounts for approximately 1–5% of all trauma cases, is accompanied by organ damage and can result in hemodynamic instability.
12 In the United States, renal trauma is reported to occur in approximately 4.9 cases per 100,000 people every year.
3 According to one study, it is more prevalent among males than females with most patients in their 20s.
3
Previously, renal trauma was managed with open surgical intervention, which often led to nephrectomy.
4 However, for the past several centuries, conservative management has been performed in patients with stable renal trauma.
5 Conservative management is suitable for patients with low-grade injuries, and recently, conservative management is being preferred for patients with high-grade injuries as well.
6 Due to the development of interventional radiological techniques, fewer complications have been reported in a case series in which trauma patients were managed using embolization for bleeding control.
78
However, there are few epidemiological studies on renal trauma in Asia, including Korea.
9 In addition, there are few studies that provide epidemiological data on treatment modalities for renal trauma; however, most of these studies have been limited to small case series. Therefore, we present epidemiological data on renal trauma using the National Health Insurance Service (NHIS) database.
RESULT
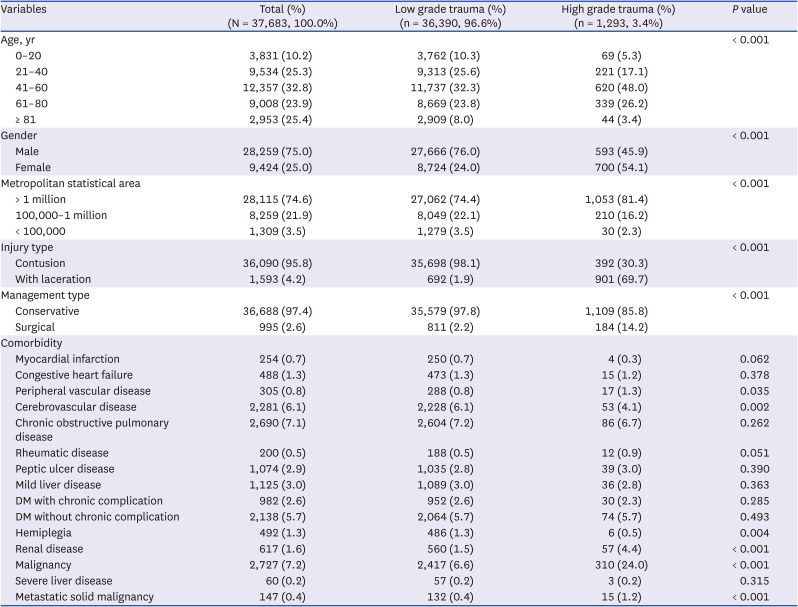
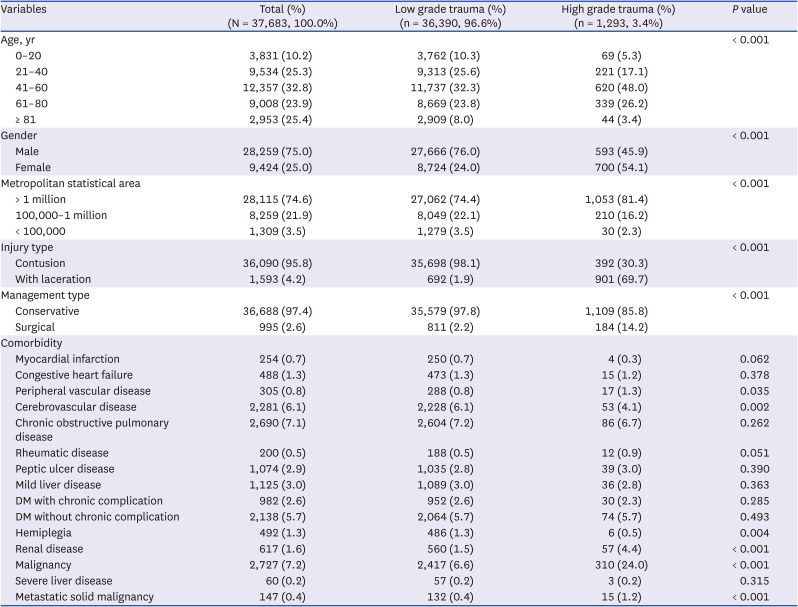
Table 1 shows the baseline characteristics of patients with renal trauma. Our final cohort comprised 37,683 individuals with renal trauma, including 1,293 patients (3.4%) diagnosed with high-grade renal trauma. Among all patients with renal trauma, surgical therapy was performed in 995 patients (2.6%), and among patients with high-grade renal trauma, surgery was performed in 184 patients (14.2%). Renal trauma occurred in all age groups (10.2–32.8%), and the ratio between men and women was approximately 3:1 (28,259 vs. 9,424). The injury mechanism was mostly contusion (95.8%) and conservative management was preferred for most patients (97.4%). There were significant differences in sex, hospital location, and method of management between the low-grade and high-grade trauma groups. In addition, individuals with high-grade renal trauma had a higher proportion of a history of PVD (0.8% vs. 1.3%,
P < 0.035), renal disease (1.5% vs. 4.4%,
P < 0.001), malignancy (6.6% vs. 24.0%,
P < 0.001), and metastatic solid tumors (0.4% vs. 1.2%,
P < 0.001). However, individuals with low-grade renal trauma had a higher incidence of cerebrovascular disease (6.1% vs. 4.1%,
P = 0.002) and hemiplegia (1.3% vs. 0.5%,
P = 0.004). There were no significant differences in the history of MI, CHF, COPD, rheumatic disease, peptic ulcer disease, mild or severe liver disease, and DM (with or without complications) between the two groups.
Table 1
Patient, hospital, and injury characteristics of patients with renal trauma
|
Variables |
Total (%) (N = 37,683, 100.0%) |
Low grade trauma (%) (n = 36,390, 96.6%) |
High grade trauma (%) (n = 1,293, 3.4%) |
P value |
|
Age, yr |
|
|
|
< 0.001 |
|
0–20 |
3,831 (10.2) |
3,762 (10.3) |
69 (5.3) |
|
21–40 |
9,534 (25.3) |
9,313 (25.6) |
221 (17.1) |
|
41–60 |
12,357 (32.8) |
11,737 (32.3) |
620 (48.0) |
|
61–80 |
9,008 (23.9) |
8,669 (23.8) |
339 (26.2) |
|
≥ 81 |
2,953 (25.4) |
2,909 (8.0) |
44 (3.4) |
|
Gender |
|
|
|
< 0.001 |
|
Male |
28,259 (75.0) |
27,666 (76.0) |
593 (45.9) |
|
Female |
9,424 (25.0) |
8,724 (24.0) |
700 (54.1) |
|
Metropolitan statistical area |
|
|
|
< 0.001 |
|
> 1 million |
28,115 (74.6) |
27,062 (74.4) |
1,053 (81.4) |
|
100,000–1 million |
8,259 (21.9) |
8,049 (22.1) |
210 (16.2) |
|
< 100,000 |
1,309 (3.5) |
1,279 (3.5) |
30 (2.3) |
|
Injury type |
|
|
|
< 0.001 |
|
Contusion |
36,090 (95.8) |
35,698 (98.1) |
392 (30.3) |
|
With laceration |
1,593 (4.2) |
692 (1.9) |
901 (69.7) |
|
Management type |
|
|
|
< 0.001 |
|
Conservative |
36,688 (97.4) |
35,579 (97.8) |
1,109 (85.8) |
|
Surgical |
995 (2.6) |
811 (2.2) |
184 (14.2) |
|
Comorbidity |
|
|
|
|
|
Myocardial infarction |
254 (0.7) |
250 (0.7) |
4 (0.3) |
0.062 |
|
Congestive heart failure |
488 (1.3) |
473 (1.3) |
15 (1.2) |
0.378 |
|
Peripheral vascular disease |
305 (0.8) |
288 (0.8) |
17 (1.3) |
0.035 |
|
Cerebrovascular disease |
2,281 (6.1) |
2,228 (6.1) |
53 (4.1) |
0.002 |
|
Chronic obstructive pulmonary disease |
2,690 (7.1) |
2,604 (7.2) |
86 (6.7) |
0.262 |
|
Rheumatic disease |
200 (0.5) |
188 (0.5) |
12 (0.9) |
0.051 |
|
Peptic ulcer disease |
1,074 (2.9) |
1,035 (2.8) |
39 (3.0) |
0.390 |
|
Mild liver disease |
1,125 (3.0) |
1,089 (3.0) |
36 (2.8) |
0.363 |
|
DM with chronic complication |
982 (2.6) |
952 (2.6) |
30 (2.3) |
0.285 |
|
DM without chronic complication |
2,138 (5.7) |
2,064 (5.7) |
74 (5.7) |
0.493 |
|
Hemiplegia |
492 (1.3) |
486 (1.3) |
6 (0.5) |
0.004 |
|
Renal disease |
617 (1.6) |
560 (1.5) |
57 (4.4) |
< 0.001 |
|
Malignancy |
2,727 (7.2) |
2,417 (6.6) |
310 (24.0) |
< 0.001 |
|
Severe liver disease |
60 (0.2) |
57 (0.2) |
3 (0.2) |
0.315 |
|
Metastatic solid malignancy |
147 (0.4) |
132 (0.4) |
15 (1.2) |
< 0.001 |

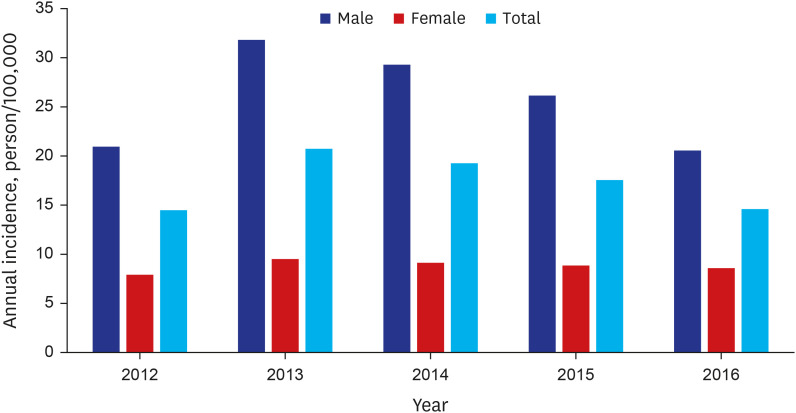
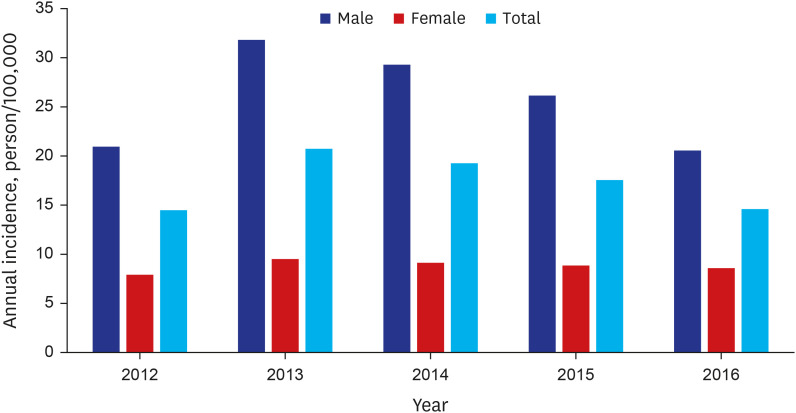
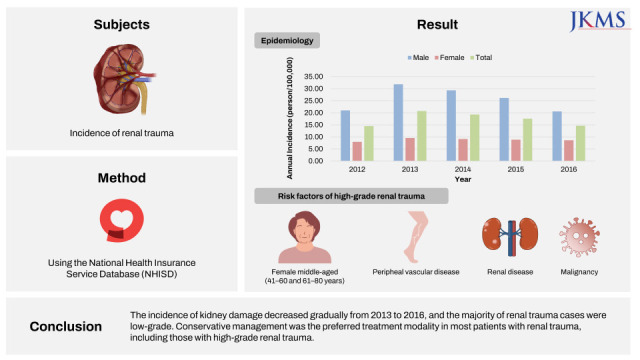
The annual incidence of renal trauma is shown in
Fig. 1. Annual incidence of renal trauma is 17.33 per 100,000 population from 2012 to 2016. The number of cases of renal trauma decreased from 2013 to 2016. Men and women experienced 8,000 (31.82/100,000) and 2,365 (9.52/100,000) renal injuries in 2013 (total: 10,365, 20.73/100,000), and 5,243 (20.56/100.000) and 2,168 (8.58/100,000) in 2016 (total: 7,411, 14.60/100,000), respectively. The annual incidence of renal trauma showed a decreasing trend (Poisson regression; hazard ratio [HR], 0.983; 95% confidence interval [CI], 0.976–0.989;
P < 0.001). In addition, the risk of renal trauma was higher in men than in women (Poisson regression; HR, 2.925; 95% CI, 2.862–2.989;
P < 0.001). The annual incidence of renal trauma in the ≥ 80 years age group was higher than that in any other age group (
Supplementary Table 2). The overall annual incidence of renal trauma tended to increase with age. In particular, men in the ≥ 80 years group had the highest annual incidence of renal trauma, and men showed a higher annual incidence than women across all age groups.
Fig. 1
Annual incidence of renal trauma of Korea. The annual incidence of renal trauma has a trend of decreasing (Poisson regression; HR, 0.983; 95% CI, 0.976–0.989; P < 0.001). Risk of renal trauma in men is higher than women (Poisson regression; HR, 2.925; 95% CI, 2.862–2.989; P < 0.001).
HR = hazard ratio, CI = confidence interval.

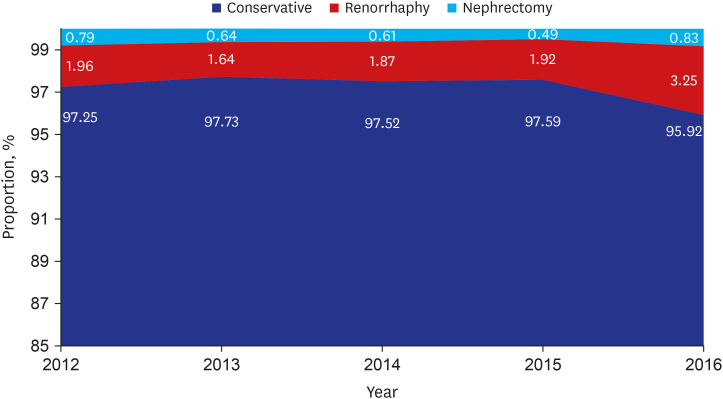
During the 5-year study period, more than 95% of the patients with renal trauma received conservative treatment (
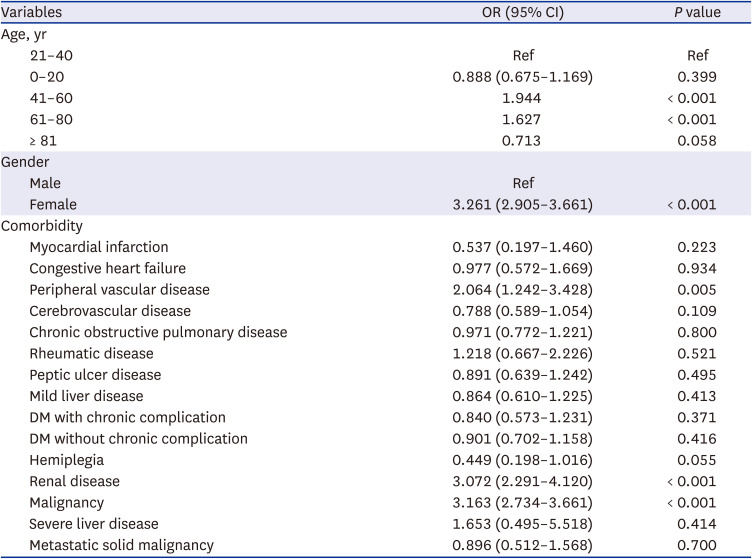
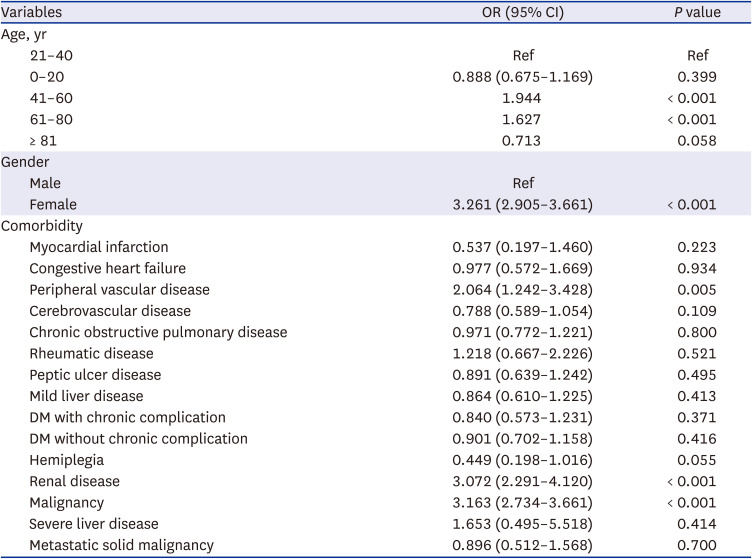
Fig. 2). Surgical management for renal trauma was preferred in less than 4% and open nephrectomy for less than 1%, during the study period. Logistic regression analysis was used to assess risk factors for high-grade renal trauma (
Table 2). Middle age groups (age; 41–60 and 61–80 years) were found to be risk factors for high-grade trauma. Female sex was also a significant risk factor for high-grade renal trauma (odds ratio, 3.261; 95% CI, 2.905–3.661). Comorbidities, such as PVD, RD, and malignancy, were also associated with high-grade renal trauma.
Fig. 2
Trends in the management of renal trauma between 2012 and 2016.
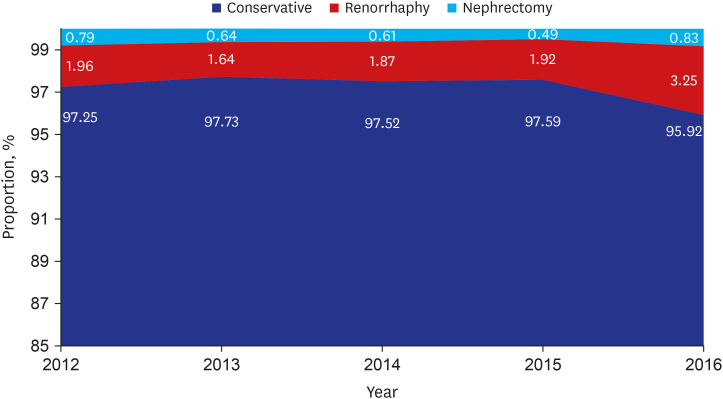

Table 2
Multivariable analysis of risk factors for high grade renal trauma
|
Variables |
OR (95% CI) |
P value |
|
Age, yr |
|
|
|
21–40 |
Ref |
Ref |
|
0–20 |
0.888 (0.675–1.169) |
0.399 |
|
41–60 |
1.944 |
< 0.001 |
|
61–80 |
1.627 |
< 0.001 |
|
≥ 81 |
0.713 |
0.058 |
|
Gender |
|
|
|
Male |
Ref |
|
|
Female |
3.261 (2.905–3.661) |
< 0.001 |
|
Comorbidity |
|
|
|
Myocardial infarction |
0.537 (0.197–1.460) |
0.223 |
|
Congestive heart failure |
0.977 (0.572–1.669) |
0.934 |
|
Peripheral vascular disease |
2.064 (1.242–3.428) |
0.005 |
|
Cerebrovascular disease |
0.788 (0.589–1.054) |
0.109 |
|
Chronic obstructive pulmonary disease |
0.971 (0.772–1.221) |
0.800 |
|
Rheumatic disease |
1.218 (0.667–2.226) |
0.521 |
|
Peptic ulcer disease |
0.891 (0.639–1.242) |
0.495 |
|
Mild liver disease |
0.864 (0.610–1.225) |
0.413 |
|
DM with chronic complication |
0.840 (0.573–1.231) |
0.371 |
|
DM without chronic complication |
0.901 (0.702–1.158) |
0.416 |
|
Hemiplegia |
0.449 (0.198–1.016) |
0.055 |
|
Renal disease |
3.072 (2.291–4.120) |
< 0.001 |
|
Malignancy |
3.163 (2.734–3.661) |
< 0.001 |
|
Severe liver disease |
1.653 (0.495–5.518) |
0.414 |
|
Metastatic solid malignancy |
0.896 (0.512–1.568) |
0.700 |

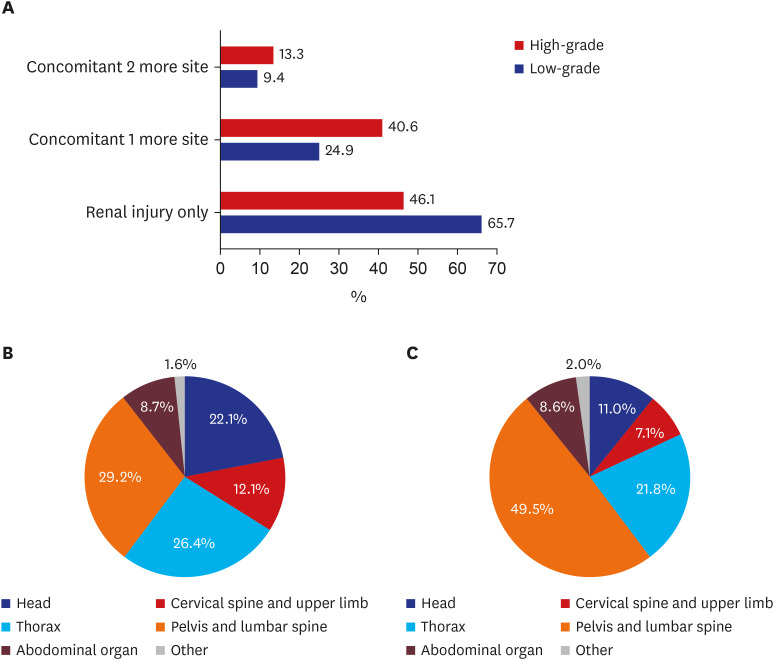
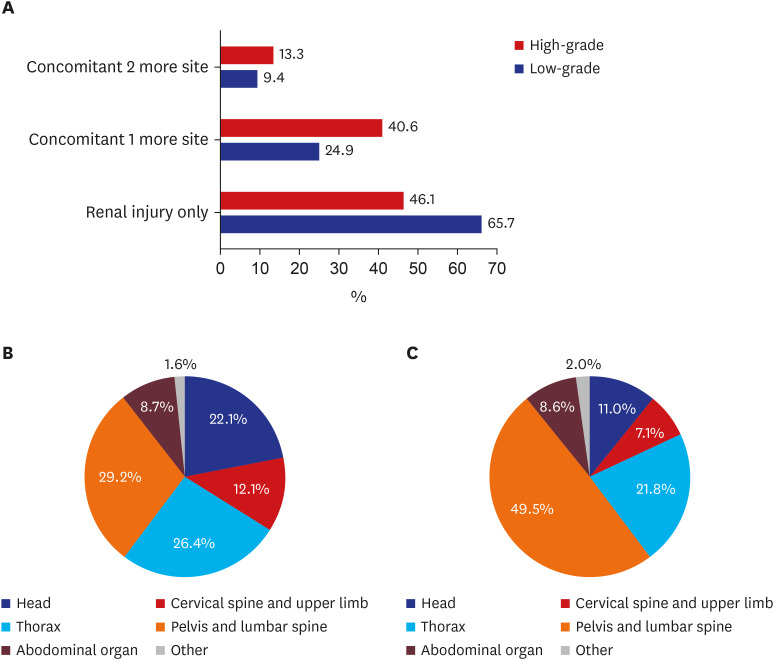
There was a higher incidence of concomitant other site injuries (high-grade 53.9% vs. low-grade 34.3%,
P < 0.001), especially in 13.3% of patients with concomitant injuries at ≥ 2 sites (
Fig. 3). In addition, among the patients with high-grade injuries, there was a difference between the most affected sites. Patients with high-grade injuries exhibited the most concomitant injuries in the pelvis and lumbar spine regions, whereas low-grade patients showed no significant difference in the proportion of affected organs, such as the pelvis, thorax, and head.
Fig. 3
Organs affected by trauma. (A) There was a higher incidence of concomitant other site injuries (high grade 53.9% vs low grade 34.3%, P < 0.001). (B) Proportion of concomitant other site injuries in low-grade renal trauma. (C) Proportion of concomitant other site injuries in high-grade renal trauma.

DISCUSSION
Most previous studies on renal trauma were retrospective studies with small sample sizes because renal trauma is not a frequent condition. There have been some nationwide studies in the United States, but no epidemiological differences were found in the country because no relevant studies have been conducted in other countries.
31213 In addition, the incidence and optimal treatment of renal injuries have not yet been established in population-based cross-sectional studies or prospective trials.
3
Using a population-based analysis, we reported the incidence of traumatic renal injuries in South Korea and found that a higher proportion of traumatized patients had kidney injuries than previously reported. In a previous nationwide study, the incidence of renal trauma was 4.9 per 100,000 people in the United States.
12 However, the incidence of renal trauma in our study (17.33 per 100,000 population) was higher than that reported in the previously mentioned study. This difference can be attributed to a few reasons. First, since the previous study was conducted 15 years ago, advances in diagnostic techniques may have increased the diagnostic rates of low-grade renal trauma. Second, physical or geographic differences between Westerners and Asians can validate this difference. Third, the previous study, based on the discharge database, included only those patients hospitalized for trauma; therefore, it did not include patients diagnosed with minor renal injuries and released.
12
The number and proportion of patients with renal trauma were highest for the 41–60 years group in our cohort; however, the annual incidence of renal trauma (per 100, 000 people) increases with age, and the oldest age group (≥ 80 years) exhibits the highest annual incidence of renal trauma. Most studies on renal trauma did not analyze annual incidence according to age group. To the best of our knowledge, this is the first study to evaluate and report the incidence of renal trauma per population by age. In the previous population-based study in the USA, 70–80% of renal injuries occurred in those aged < 44 years because renal injuries are more common in individuals with high-risk activities.
312 Although we found that renal trauma was relatively small in the older age group, the incidence per population was high. One possible explanation for this can be that older people are at a higher risk of falling, have more comorbidities, and have less muscle mass, making them vulnerable to trauma. However, the proportion of high-grade injuries in the elderly group was relatively low; thus, old age was not considered a risk factor for high-grade trauma in the multivariable analysis.
Children are at an increased risk of renal trauma owing to their unique anatomic differences compared to adults.
14 Grimsby et al.
15 reported that according to the American College of Surgeons National Trauma Data Bank, 25% of renal trauma in the pediatric population occurred in individuals younger than 19 years. In contrast, only 10.17% of the patients with renal trauma were younger than 20 years in this cohort. One possible explanation could be that, although the relatively high incidence of renal trauma in youth has been attributed to its involvement in high-risk activities,
16 most children and youth of present times show insufficient physical activity. Moreover, Korea’s 2018 Report Card stated that Korean children and youth continue to be physically inactive and sedentary, with an average overall grade of D+.
17 Sociocultural background may have affected the relative incidence of youth renal trauma in Korea. However, although the incidence of renal trauma in pediatric or young patients was lower than that in other ages in Korea, the incidence was similar to that reported in other nationwide studies.
12
The guidelines for the management of high-grade injuries have some discrepancies. The Société Internationale d'Urologie (SIU) recommends exploratory laparotomy for the treatment of high-grade renal injuries, while the European Association of Urology (EAU) only recommends renal exploration if the injury site is vascular.
316 The American Urologic Association (AUA) recommends observation for hemodynamically stable patients regardless of trauma grade, owing to clinician variability regarding the classification of grade 4 and 5 injuries.
18 In particular, the AUA and EAU guidelines recommend angioembolization as a first-line treatment strategy for patients with active bleeding, with no other indications, for immediate open surgery. However, conservative management is the preferred treatment strategy for patients with high-grade injuries, as indicated by other studies. Aldiwani et al.
19 demonstrated that only 4 of 36 patients with high-grade trauma underwent open nephrectomy due to hemodynamic instability. Lanchon et al.
20 also reported in their prospective study that 110 of 151 patients (89%) with high-grade injuries required only nonoperative management. Grimsby et al.
15 and Voelzke and Leddy
21 suggested, in a literature review, that 94% of renal trauma care was nonoperative. Similarly, in this cohort, more than 95% of renal trauma patients underwent conservative management regardless of the trauma grade, and 85.77% of patients with high-grade injuries underwent conservative management.
The specific contributions of this study are as follows: To our knowledge, this is the first epidemiological study of renal trauma in Asia. Unlike previous studies in Western countries, this study presents a somewhat different result for the first time. Unlike previous studies in the West, this study is the first to present a slightly different result, based on the influence of sociocultural background. Additionally, our study showed that female sex and some medical conditions were risk factors for high-grade renal trauma using multivariable analysis.
Despite the contributions of this study, some limitations should be addressed. First, this study had a retrospective observational design based on claims data, and our criteria for renal trauma were limited to diagnosis codes. In addition, current claims data did not include mortality data; therefore, these data may not be appropriate for the comparison of treatment modalities, outcomes, or quality of care. Second, the NHIS claims data have no information about the cause of the trauma; therefore, we could not analyze the common causes of renal trauma. Third, because the NHIS claims data provide fewer than 100 million clinical records per research project, we could only analyze five-year data, which could be a source of bias. Fourth, there is the possibility of coding errors in such a large database. Fifth, the NHIS claims data do not provide robotic surgery codes. Therefore, if a simple or partial nephrectomy using a robot was performed, it is possible that patients, who were treated with robotic surgery, were not included in the surgical treatment group. However, robotic surgery has not been widely used for patients with renal trauma who have a very high risk of bleeding, and only few related studies have been conducted to date.
In conclusion, after analyzing claims-based nationwide data, the annual incidence of renal trauma decreased from 2013 to 2016 (Poisson regression; HR, 0.983; 95% CI, 0.976–0.989; P < 0.001), and approximately 3% of patients were diagnosed with high-grade renal trauma. Conservative management was preferred for most patients with renal trauma (up to 97%), including those with high-grade renal trauma (up to 86%).




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download