1. Cheon CK, Jin HS, Kang EK, Kim HB, Kim BJ, Yu J, et al. Epidemic acute interstitial pneumonia in children occurred during the early 2006s. Korean J Pediatr. 2008; 51(4):383–390.
2. Kim BJ, Kim HA, Song YH, Yu J, Kim S, Park SJ, et al. Nationwide surveillance of acute interstitial pneumonia in Korea. Korean J Pediatr. 2009; 52(3):324–329.
3. Kim HJ, Lee MS, Hong SB, Huh JW, Do KH, Jang SJ, et al. A cluster of lung injury cases associated with home humidifier use: an epidemiological investigation. Thorax. 2014; 69(8):703–708. PMID:
24488371.
4. Hong SB, Kim HJ, Huh JW, Do KH, Jang SJ, Song JS, et al. A cluster of lung injury associated with home humidifier use: clinical, radiological and pathological description of a new syndrome. Thorax. 2014; 69(8):694–702. PMID:
24473332.
5. Paek D, Koh Y, Park DU, Cheong HK, Do KH, Lim CM, et al. Nationwide study of humidifier disinfectant lung injury in South Korea, 1994-2011. Incidence and dose-response relationships. Ann Am Thorac Soc. 2015; 12(12):1813–1821. PMID:
26653190.
6. Kim WY, Hong SB. Humidifier disinfectant-associated lung injury: six years after the tragic event. Tuberc Respir Dis (Seoul). 2017; 80(4):351–357. PMID:
28905528.
7. Yon DK, Lee SW, Woo A, Koh HY, Jee HM, Ha EK, et al. Exposure to humidifier disinfectants is associated with upper and lower airway diseases. Pediatr Allergy Immunol. 2020; 31(5):578–582. PMID:
32068913.
8. Leem JH, Lee JH. Humidifier disinfectant-associated specific diseases should be called together as “humidifier disinfectant syndrome”. Environ Health Toxicol. 2017; 32:e2017017. PMID:
29026061.
9. Choi Y, Paek D. Humidifier disinfectants, unfinished stories. Environ Health Toxicol. 2016; 31:e2016004. PMID:
26987713.
10. Yoon J, Lee SY, Lee SH, Kim EM, Jung S, Cho HJ, et al. Exposure to humidifier disinfectants increases the risk for asthma in children. Am J Respir Crit Care Med. 2018; 198(12):1583–1586. PMID:
30192634.
12. Vandenplas O, Wiszniewska M, Raulf M, de Blay F, Gerth van Wijk R, Moscato G, et al. EAACI position paper: irritant-induced asthma. Allergy. 2014; 69(9):1141–1153. PMID:
24854136.
13. Tarlo SM. Irritant-induced asthma in the workplace. Curr Allergy Asthma Rep. 2014; 14(1):406. PMID:
24343122.
14. Kim KW, Ahn K, Yang HJ, Lee S, Park JD, Kim WK, et al. Humidifier disinfectant-associated children’s interstitial lung disease. Am J Respir Crit Care Med. 2014; 189(1):48–56. PMID:
24199596.
15. Kim BK, Kim JY, Kang MK, Yang MS, Park HW, Min KU, et al. Allergies are still on the rise? A 6-year nationwide population-based study in Korea. Allergol Int. 2016; 65(2):186–191. PMID:
26666496.
16. Huh JW, Hong SB, Do KH, Koo HJ, Jang SJ, Lee MS, et al. Inhalation lung injury associated with humidifier disinfectants in adults. J Korean Med Sci. 2016; 31(12):1857–1862. PMID:
27822921.
18. Graham BL, Brusasco V, Burgos F, Cooper BG, Jensen R, Kendrick A, et al. 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur Respir J. 2017; 49(1):1600016. PMID:
28049168.
19. Yoo S, Sim M, Choi J, Jeon K, Shin J, Chung S, et al. Psychological responses among humidifier disinfectant disaster victims and their families. J Korean Med Sci. 2019; 34(4):e29. PMID:
30686951.
20. Sterk PJ, Fabbri LM, Quanjer PH, Cockcroft DW, O’Byrne PM, Anderson SD, et al. Airway responsiveness. Standardized challenge testing with pharmacological, physical and sensitizing stimuli in adults. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Eur Respir J Suppl. 1993; 16:53–83. PMID:
8499055.
21. Anderson SD, Charlton B, Weiler JM, Nichols S, Spector SL, Pearlman DS, et al. Comparison of mannitol and methacholine to predict exercise-induced bronchoconstriction and a clinical diagnosis of asthma. Respir Res. 2009; 10(1):4. PMID:
19161635.
22. Coates AL, Wanger J, Cockcroft DW, Culver BH, Diamant Z, et al. Bronchoprovocation Testing Task Force: Kai-Håkon Carlsen. ERS technical standard on bronchial challenge testing: general considerations and performance of methacholine challenge tests. Eur Respir J. 2017; 49(5):1601526. PMID:
28461290.
23. Park JO, Choi IS, Park KO. Normal predicted values of single-breath diffusing capacity of the lung in healthy nonsmoking adults. Korean J Intern Med. 1986; 1(2):178–184. PMID:
3154613.
24. Song EH, Oh YM, Hong SB, Shim TS, Lim CM, Lee SD, et al. Selection of reference equations for lung volumes and diffusing capacity in Korea. Tuberc Respir Dis (Seoul). 2006; 61(3):218.
25. Ra SW, Park TS, Hong Y, Hong SB, Shim TS, Lim CM, et al. Clinical usefulness and the accuracy of Korean reference equation for diffusing capacity. Tuberc Respir Dis (Seoul). 2008; 64(2):80–86.
26. Choi JK, Paek D, Lee JO. Normal predictive values of spirometry in Korean population. Tuberc Respir Dis (Seoul). 2005; 58(3):230–242.
27. Quanjer PH. Standardized lung function testing. Report working party. Bull Eur Physiopathol Respir. 1983; 19(Suppl 5):1–95. PMID:
6616097.
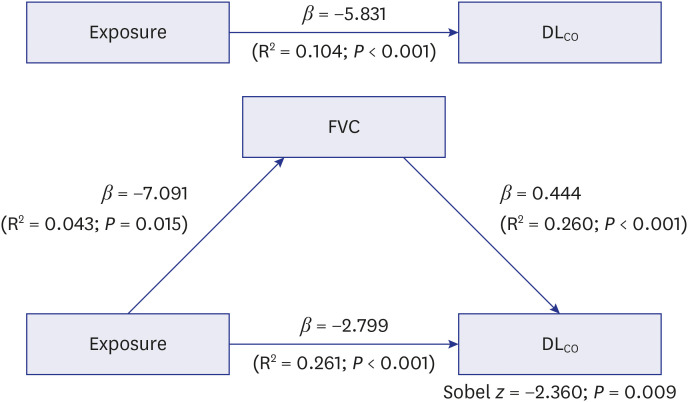
28. Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol. 1982; 13:290–312.
29. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986; 51(6):1173–1182. PMID:
3806354.
30. Ditlevsen S, Christensen U, Lynch J, Damsgaard MT, Keiding N. The mediation proportion: a structural equation approach for estimating the proportion of exposure effect on outcome explained by an intermediate variable. Epidemiology. 2005; 16(1):114–120. PMID:
15613954.
31. Morrison NJ, Abboud RT, Ramadan F, Miller RR, Gibson NN, Evans KG, et al. Comparison of single breath carbon monoxide diffusing capacity and pressure-volume curves in detecting emphysema. Am Rev Respir Dis. 1989; 139(5):1179–1187. PMID:
2712446.
32. Wang JS. Relationship of carbon monoxide pulmonary diffusing capacity to postoperative cardiopulmonary complications in patients undergoing pneumonectomy. Kaohsiung J Med Sci. 2003; 19(9):437–446. PMID:
14604318.
33. do Pico GA, Wiley AL Jr, Rao P, Dickie HA. Pulmonary reaction to upper mantle radiation therapy for Hodgkin’s disease. Chest. 1979; 75(6):688–692. PMID:
436520.
34. Theuws JC, Muller SH, Seppenwoolde Y, Kwa SL, Boersma LJ, Hart GA, et al. Effect of radiotherapy and chemotherapy on pulmonary function after treatment for breast cancer and lymphoma: a follow-up study. J Clin Oncol. 1999; 17(10):3091–3100. PMID:
10506604.
35. Espiritu JD, Ruppel G, Shrestha Y, Kleinhenz ME. The diffusing capacity in adult cystic fibrosis. Respir Med. 2003; 97(6):606–611. PMID:
12814143.
36. Sansores RH, Pare PD, Abboud RT. Acute effect of cigarette smoking on the carbon monoxide diffusing capacity of the lung. Am Rev Respir Dis. 1992; 146(4):951–958. PMID:
1416424.
37. Graham BL, Mink JT, Cotton DJ. Effects of increasing carboxyhemoglobin on the single breath carbon monoxide diffusing capacity. Am J Respir Crit Care Med. 2002; 165(11):1504–1510. PMID:
12045124.
38. Lee SY, Ahn HS, Kim EM, Kim KK, Kang MJ, Park MJ, et al. Different characteristics of childhood asthma related to Polyhexamethylene guanidine exposure. Ann Am Thorac Soc. 2021; 18(9):1523–1532. PMID:
33561373.
39. Song MK, Kim DI, Lee K. Causal relationship between humidifier disinfectant exposure and Th17-mediated airway inflammation and hyperresponsiveness. Toxicology. 2021; 454:152739. PMID:
33640443.
40. Lee SH, Ahn JR, Go HN, Lee SY, Park MJ, Song KB, et al. Exposure to Polyhexamethylene guanidine exacerbates bronchial hyperresponsiveness and lung inflammation in a mouse model of ovalbumin-induced asthma. Allergy Asthma Immunol Res. 2021; 13(4):655–664. PMID:
34212551.
41. Cho HJ, Park DU, Yoon J, Lee E, Yang SI, Kim YH, et al. Effects of a mixture of chloromethylisothiazolinone and methylisothiazolinone on peripheral airway dysfunction in children. PLoS One. 2017; 12(4):e0176083. PMID:
28453578.
42. Lugogo N, Que LG, Gilstrap DL, Kraft M. Asthma: Clinical diagnosis and management. Broaddus VC, editor. Murray & Nadel’s Textbook of Respiratory Medicine. 6th ed. Philadelphia, PA, USA: Elsevier Saunders;2016. p. 731–750.
43. Saydain G, Beck KC, Decker PA, Cowl CT, Scanlon PD. Clinical significance of elevated diffusing capacity. Chest. 2004; 125(2):446–452. PMID:
14769723.
44. Collard P, Njinou B, Nejadnik B, Keyeux A, Frans A. Single breath diffusing capacity for carbon monoxide in stable asthma. Chest. 1994; 105(5):1426–1429. PMID:
8181330.
45. Pinkerton KE, Green FH, Saiki C, Vallyathan V, Plopper CG, Gopal V, et al. Distribution of particulate matter and tissue remodeling in the human lung. Environ Health Perspect. 2000; 108(11):1063–1069. PMID:
11102298.
46. Green FH, Churg A. Occupational asthma, byssinosis, extrinsic allergic alveolitis and related conditions. Churg A, Green FHY, editors. Pathology of Occupational Lung Disease. 2nd ed. Baltimore, MD, USA: Williams & Wilkins;1998. p. 403–450.
47. Pietropaoli AP, Frampton MW, Hyde RW, Morrow PE, Oberdörster G, Cox C, et al. Pulmonary function, diffusing capacity, and inflammation in healthy and asthmatic subjects exposed to ultrafine particles. Inhal Toxicol. 2004; 16(Suppl 1):59–72. PMID:
15204794.
48. Lee JH, Yu IJ. Human exposure to polyhexamethylene guanidine phosphate from humidifiers in residential settings: cause of serious lung disease. Toxicol Ind Health. 2017; 33(11):835–842. PMID:
28992790.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download