This article has been
cited by other articles in ScienceCentral.
Abstract
Background
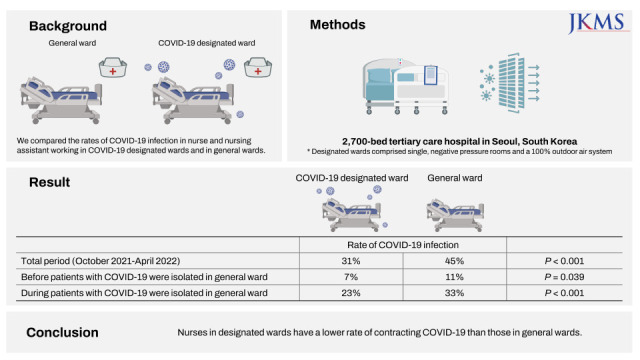
To evaluate the effects of isolating coronavirus disease 2019 (COVID-19) patients in general wards, we compared the rates of COVID-19 infection in nurses and nursing assistants working in COVID-19 designated wards and in general wards of our hospital from 1 October 2021 to 21 April 2022.
Methods
This study was conducted in a 2,700-bed tertiary care hospital in Seoul, Korea. Designated wards comprised single, negative pressure rooms and a 100% outdoor air system.
Results
During the study period, a total of 2,698 nurses and nursing assistants were employed at our hospital, of whom 310 (11%) were working in the designated wards, and the remaining 2,388 (89%) in the general wards, and among whom 1,158 (43%) were diagnosed with COVID-19. The healthcare workers (HCWs) in the designated wards were less frequently diagnosed with COVID-19 than those in the general wards (31% vs. 45%, P < 0.001). During the period before patients with COVID-19 were isolated in general wards, and during the period after these cases were isolated in general ward, HCWs in designated wards were less frequently infected with the virus than those in general wards (7% vs. 11%, P = 0.039; and 23% vs. 33%, P < 0.001, respectively).
Conclusion
HCWs in designated wards have a lower rate of contracting COVID-19 than those in general wards. A lack of exposure to undiagnosed cases and their caregivers, greater care with social distancing outside the hospital, higher rates of 3-dose vaccinations, and the use of isolation rooms with negative pressure may be associated with this finding.
Go to :

Graphical Abstract
Go to :

Keywords: COVID-19, SARS-CoV-2, Healthcare Workers, Isolation
INTRODUCTION
The emergence of the omicron variant of coronavirus disease 2019 (COVID-19) in January 2022 in Korea was associated with a surge of positive cases and shortage of beds for those who required hospitalization. In March 2022 therefore, the Korean government changed the policy from isolation these patients in designated wards to general ward isolation, especially for COVID-positive inpatients who had only mild illness during their hospitalization.
1 However, there have been concerns about this change in policy in terms of the potential for transmission to other patients in the same wards and to healthcare workers (HCWs).
To evaluate the effects of isolating COVID-19 patients in general wards, we compared the rates of COVID-19 infection in nurse and nursing assistant (HCWs) working in COVID-19 designated wards and in general wards of our hospital from 1 October 2021 to 21 April 2022. As COVID-19 patients began to be isolated in general wards since March 2022, we divided the study periods into those before and after this date in our analyses.
Go to :

METHODS
Settings and general infection control measures
This study was performed at Asan Medical Center, a 2,700-bed tertiary care hospital in Seoul, South Korea. All HCW subjects were required to notify to infection control team upon a positive COVID-19 test result, and we retrospectively reviewed their demographic data, vaccination histories, and day of diagnosis with this infection. We compared the rates of COVID-19 infection in the nurses and nursing assistants in COVID-19 designated wards and general wards from 1 October 2021 to 21 April 2022. The delta variant of this virus had been dominant in South Korea from July 2021 to January 2022, but the omicron variant became the dominant strain from the third week of January 2022.
2
From October 2021 to February 2022, all patients at our hospital were screened for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) using real-time polymerase chain reaction (PCR) at pre-admission, and then tested again during their stay (on days 4, 8, 14 and weekly thereafter) regardless of symptoms. In addition, resident caregivers were required to take routine SARS-CoV-2 tests before visiting the hospital (≤ 2 days prior), on days 4, 8, and 14 of their residency, and weekly thereafter. From March 2022, all patients and resident caregivers were tested for SARS-CoV-2 using real-time PCR at pre-admission, and on days 3 and 7 of hospitalization. The days on which testing was done were reduced due to the burden of the significantly increased numbers of cases in this period. In addition, all patients underwent SARS-CoV-2 testing if they showed any symptoms or signs of COVID-19. A universal mask-wearing policy was mandated in the hospital, with HCWs required to wear goggles and FFP2 equivalent masks (KF94 mask) when they encountered patients in the general ward. Close contact (exposure) was defined as follows: 1) being within 2 meters of a COVID-19 case for ≥ 3 minutes without an N95 respirator or FFP2 equivalent respirator (KF94 mask) and eye protection; or 2) not wearing appropriate PPE (gown, gloves, N95 respirator [or FFP2 equivalent respirator], and goggles or face shield) when performing an aerosol generating procedure. Exposed HCWs who had received a 3-dose vaccination could continue working were required to receive a PCR test immediately and at 5 days after the exposure. Those who did not receive a 3-dose vaccination were quarantined.
Settings in the designated wards
There were 109 beds available for COVID-19 patients in the designated wards at our hospital during the study period. Only confirmed COVID-19 patients were admitted to these bespoke facilities and entry by guardians or other family members was restricted. The transport and movement of patients outside of these rooms was allowed for medically essential purposes only. HCWs working in these designated wards were required to wear a gown, gloves, an N95 respirator, and goggles or a face shield when they care for COVID-19 patients. N95 respirators, or an FFP2 equivalent respirator (KF94 mask), were worn by staff at the nurse’s stations with or without goggles or a face shield. All of the rooms in the designated wards were airborne infection isolation rooms (single rooms or multi-patient rooms with negative pressure and a 100% outdoor air system). In the newly built designated wards, each room had anteroom and the whole building HVAC (heating, ventilation, and air conditioning) system in the patients’ area was set to −5.0 Pa pressure with 100% outdoor air and air exchange rate 10 per hour. In the remolded designated wards, communal anteroom in the hallway was built, and portable negative air pressure machines were installed. Pressure level was set to −2.5 Pa difference between patient room and anteroom, or between anteroom and nurse station. In addition, the nurse station and the hallway was separated by a wall in the designated wards.
Settings in the general wards
Since 5 March 2022, inpatients at Asan Medical Center who tested positive for COVID-19 during their hospitalization have been isolated in a single room with a dedicated bathroom, with or without negative pressure, in one of the general wards. The doors to these rooms have been kept closed at all times and transport of the patient out of the room was again only allowed for medically essential purposes. HCWs were required to wear a gown, gloves, N95 respirator, and goggles or a face shield when they entered these isolation rooms. These staff also frequently wore both an N95 respirator or FFP2 equivalent respirator (KF94 mask) and eye protection (goggles or face shield) at the nurse’s station to prevent possible exposure from unknown COVID-19 cases. HCWs cared not only COVID-19 patients but also other patients without COVID-19. A single caregiver or guardian with confirmed COVID-19 positive test was permitted to stay in the room with their patient only when medically indicated (i.e., if care was needed for that individual). All of the isolation rooms in the general ward had re-circulating air systems and an air change rate per hour of 7.
Statistical analysis
For comparisons of the rates of COVID-19 infection among HCWs in the designated and general wards of our hospital from 1 October 2021 to 21 April 2022, we divided this study timeline into period 1 from 1 October 2021 to 4 March 2022, during which time COVID-19 patients were only admitted to the designated wards; and period 2 from 5 March 2022 to 21 April 2022 when COVID-19 patients were also cared for in the general wards. Categorical variables were analyzed using the χ2 test or Fisher’s exact test, as appropriate. Continuous variables were analyzed using the Student’s t-test or Mann-Whitney U test, as appropriate. All tests of significance were two-tailed and P values < 0.05 were considered significant. Data were analyzed using SPSS Statistics for Windows, version 23.0 (IBM Corp., Armonk, NY, USA).
Ethics statement
The Institutional Review Board of Asan Medical Center evaluated and approved the medical, scientific, and ethical aspects of our study protocol (IRB No. 2021-0024) and the requirement for informed consent was waived by the Ethics Committee of Asan Medical Center.
Go to :

RESULTS
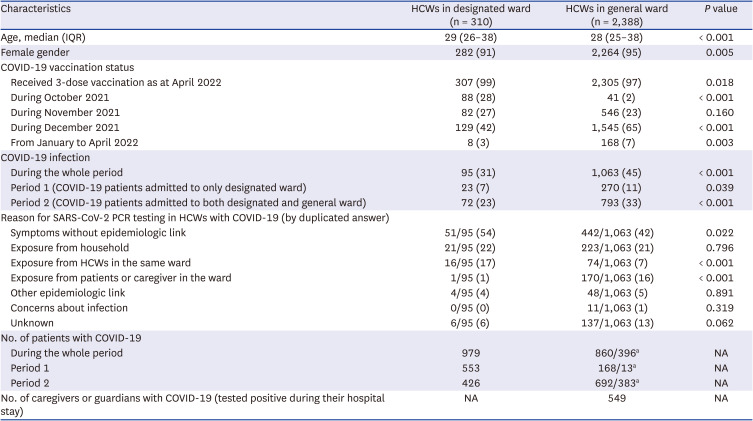
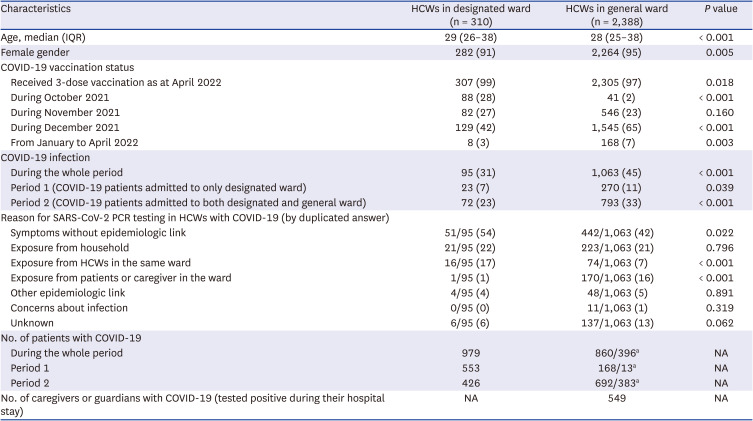
A total of 2,698 nurses and nursing assistants were included in these analyses, of whom 310 (11%) were working in designated wards, and the remaining 2,388 (89%) in general wards. The median ages of these HCWs in the designated and general wards were 29 (IQR, 26–38), and 28 (IQR, 25–38), respectively (
P < 0.001,
Table 1). Among the designated ward staff, the proportion of female HCWs was less than that in the general wards (91% vs. 95%,
P = 0.005), and more of the HCWs had received a 3-dose vaccination as at April 2022 (99% vs. 97%,
P = 0.02). During the study period also, the numbers of patients who were COVID-19 positive during their hospitalization and who were then isolated in general wards were 860 and 396, respectively. In addition, 549 caregivers or guardians tested positive for COVID-19 during their residency.
Table 1
Demographic information and the rates of COVID-19 infection of HCWs in the designated or general wards
|
Characteristics |
HCWs in designated ward (n = 310) |
HCWs in general ward (n = 2,388) |
P value |
|
Age, median (IQR) |
29 (26–38) |
28 (25–38) |
< 0.001 |
|
Female gender |
282 (91) |
2,264 (95) |
0.005 |
|
COVID-19 vaccination status |
|
|
|
|
Received 3-dose vaccination as at April 2022 |
307 (99) |
2,305 (97) |
0.018 |
|
During October 2021 |
88 (28) |
41 (2) |
< 0.001 |
|
During November 2021 |
82 (27) |
546 (23) |
0.160 |
|
During December 2021 |
129 (42) |
1,545 (65) |
< 0.001 |
|
From January to April 2022 |
8 (3) |
168 (7) |
0.003 |
|
COVID-19 infection |
|
|
|
|
During the whole period |
95 (31) |
1,063 (45) |
< 0.001 |
|
Period 1 (COVID-19 patients admitted to only designated ward) |
23 (7) |
270 (11) |
0.039 |
|
Period 2 (COVID-19 patients admitted to both designated and general ward) |
72 (23) |
793 (33) |
< 0.001 |
|
Reason for SARS-CoV-2 PCR testing in HCWs with COVID-19 (by duplicated answer) |
|
|
|
|
Symptoms without epidemiologic link |
51/95 (54) |
442/1,063 (42) |
0.022 |
|
Exposure from household |
21/95 (22) |
223/1,063 (21) |
0.796 |
|
Exposure from HCWs in the same ward |
16/95 (17) |
74/1,063 (7) |
< 0.001 |
|
Exposure from patients or caregiver in the ward |
1/95 (1) |
170/1,063 (16) |
< 0.001 |
|
Other epidemiologic link |
4/95 (4) |
48/1,063 (5) |
0.891 |
|
Concerns about infection |
0/95 (0) |
11/1,063 (1) |
0.319 |
|
Unknown |
6/95 (6) |
137/1,063 (13) |
0.062 |
|
No. of patients with COVID-19 |
|
|
|
|
During the whole period |
979 |
860/396a
|
NA |
|
Period 1 |
553 |
168/13a
|
NA |
|
Period 2 |
426 |
692/383a
|
NA |
|
No. of caregivers or guardians with COVID-19 (tested positive during their hospital stay) |
NA |
549 |
NA |

During the entire study period, 1,158 (43%) HCWs tested positive for COVID-19. The frequency of COVID-19 positivity among the HCWs was lower in the designated wards (31% vs. 45%;
P < 0.001;
Table 1). This was also found to be the case when stratified into periods 1 and 2 (7% vs. 11%,
P = 0.04 in period 1; 23% vs. 33%,
P < 0.001 in period 2). The reasons for SARS-CoV-2 testing were found to be significantly different, i.e., it was more commonly performed for HCWs in designated wards who displayed symptoms without an epidemiologic link (54% vs. 42%,
P = 0.02) and who were exposed to COVID-19 positive HCWs in the same ward (17% vs. 7%,
P < 0.001). These tests were less frequently undertaken for HCWs in the designated wards following exposure to patients or a caregiver who were positive for the virus (1% vs. 16%,
P < 0.001), compared to the general wards.
Go to :

DISCUSSION
Our present observations indicate that the COVID-19 infection rate among the HCWs working in the designated wards in our hospital to treat positive cases was significantly lower than in their counterparts in the general wards, regardless of whether they had been caring for COVID-19 patients in the general wards. The Infection Control Guidance from the Centers for Disease Control and Prevention (CDC) states that patients with a confirmed SARS-CoV-2 infection should be isolated in a single room with a dedicated bathroom, and with the door kept closed at all times.
3 These guidelines also recommend dedicated HCWs to treat these cases.
3 Notably however, few studies to date have compared the COVID-19 infection rates between HCWs working in designated COVID-19 wards and those staffing the general wards. Our findings in this regard may be explained by several factors. First, HCWs working in general wards could be exposed from patients and caregivers who were unaware that they were COVID-19 positive. HCWs in the general wards had higher chance for the exposure to the patients or caregivers with early period of SARS-CoV-2 infection without appropriate PPE than HCWs in the designated wards. Second, it is possible that the HCWs in the designated wards were more cautious and more careful to observe social distancing in the outside of the hospital (i.e., less likely to go to restaurant or other crowded public venues). However, the proportion of COVID-19 tests that were conducted due to household exposures, other epidemiologic links, or because of concerns about possible infection, were comparable between HCWs in the designated wards and those in the general wards. In contrast, the exposure from HCWs in the same ward was more common in HCWs in the designated wards than those in general wards (
Table 1). So, HCWs in the designated wards might pay less attention to social distancing in shared areas in the ward. It is worth to note that testing due to symptoms without any epidemiologic link was more common for the staff in the designated wards of our hospital in the study period. The reason for this finding is unclear, but it is possible that the HCWs in the designated wards more closely self-monitored for possible symptoms. Third, the HCWs in designated wards had higher 3-dose vaccination rate which is associated with lower infection rates.
45 However, 3rd dose vaccination campaign was conducted until the end of December 2021. So, we cannot evaluate the effect of 3rd dose vaccination on SARS-CoV-2 infection in HCWs before this period. Therefore, it is difficult to draw a firm conclusion on whether the vaccination status significantly confounded the difference in infection rate between the designated and general wards.
Finally, negative pressure and a ventilation system with 100% outdoor air and a more frequent air change rate in the designated wards will have contributed to the continuous removal of virus particles. Not all patients in the general wards were isolated in a negative pressure room, and unintended airflow from patient room to nursing stations could be occurred especially when the door opened, as previously reported.
6 Taken together, our data suggest that it is more desirable to place the patients with COVID-19 in designated ward with negative pressure room than in general ward. However, the negative pressure room isolation not only affect the patient safety, but also needs a large resources. In addition, our data could not evaluate the relative contribution of the negative pressure room and infection control program to protect HCWs from SARS-CoV-2 infection. That is, the strict compliance with infection control principles including the maintaining the up-to-date vaccine status in HCWs, appropriate screening strategy of asymptomatic or presymptomatic patients with SARS-CoV-2 infection, and the limitations of caregiver or visiting the patient may play important role in protecting HCWs from SARS-CoV-2 infection. Therefore, when the negative pressure room has some shortage due to resource limitations, balancing risk for appropriate COVID-19 patients isolation between negative pressure room isolation and non-negative pressure room isolation with strict infection control program are needed.
This study had several limitations of note. First, it was a single center study, and further research is needed to validate the wider applicability of our findings. Second, no adjustments were made for demographic factors including age and sex. Third, some may argue that the negative pressure isolation may not have a significant role in protecting HCWs entering the room from the infection source. However, the role of the negative pressure in protecting HCWs might depend on the infective dose of a given virus. If low infective dose is needed, the negative pressure may contribute to the inhalation of aerosol by HCWs especially not wearing appropriate personal protective equipment (i.e., unfitted N95 mask) in the room because the negative pressure continuously reduce the concentration of infective particles. Unfortunately, we do not exactly know the infective dose of SARS-CoV-2 infection. The recent health volunteer challenge study revealed that a low inoculum dose of 10 TCID50 was enough to infect about half of participants.
7 So, further studies are needed on the role of negative pressure room contributing to protecting HCWs entering the room in SARS-CoV-2 infection. Finally, we did not extensively investigate the infection sources of COVID-19 in the HCWs who tested positive. Hence, unmeasured confounders such as nosocomial or community outbreaks could have unevenly affected the infection rates between the two groups. Despite of limitations, our data provide important evidence not only to warrant the preparedness of negative pressure rooms for the upcoming pandemic, but also to reduce the HCWs’ concern and avoidance for caring patients with emerging infectious diseases in the designated area.
In conclusion, significantly fewer HCWs in the COVID-19 designated wards in our hospital contracted this virus compared with their colleagues working in the general wards. A clinical setting involving an isolation room with negative pressure, less contact with inpatients and caregivers who may be unaware that they are COVID-19 positive, higher rates of 3-dose vaccinations, and greater attention to social distancing, may be associated with this finding.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download