Abstract
Purpose
Acute appendicitis (AA) is one of the most frequent causes of abdominal surgery encountered in emergency rooms. However, reactive lymphoid hyperplasia (RLH) is one of the appendicular pathologies often misdiagnosed. It is quite challenging to distinguish between AA and RLH in terms of planning treatment in an emergency. Therefore, this retrospective study aimed to compare the histological and laboratory findings of AA and RLH.
Methods
The retrospective data included in the study were obtained from patients diagnosed with AA. Complete blood count (CBC) and C-reactive protein (CRP) levels of patients with AA and RLH were compared before the surgery based on the histological diagnosis of the patients.
Results
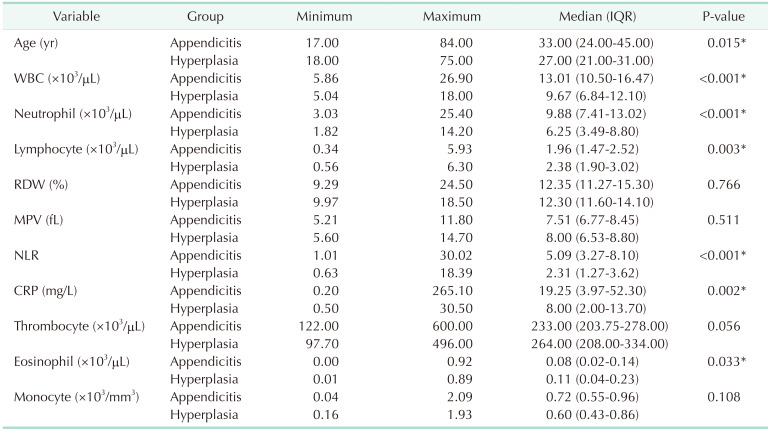
A total of 187 patients who previously underwent appendectomy were included in the study. Histopathological examination revealed that 152 patients (81.3%) were diagnosed with AA, and 35 (18.7%) with RLH. While white blood cell count (P < 0.001), neutrophil (P < 0.001), and neutrophil/lymphocyte ratio (P < 0.001) were found to be significantly higher in those with AA; lymphocyte (P = 0.003) and eosinophil counts (P = 0.033) were detected to be significantly higher in those with RLH. CRP level was also significantly higher in those with AA (P = 0.002)
Acute appendicitis (AA) is one of the most common causes of abdominal pain encountered in emergency rooms. Among the etiologies leading to abdominal pain, acute abdomen remains highest as the most common cause in all age groups. It is considered that a rapid and accurate diagnosis obtained through a detailed clinical evaluation and laboratory findings will significantly reduce the complications arising from acute abdomen [1]. To date, numerous studies have been carried out through such imaging techniques as multislice computed tomography and ultrasonography (USG), and easily accessible and applicable methods such as CRP, leukocyte count, neutrophil/lymphocyte ratio (NLR), and bilirubin to achieve a precise diagnosis before complications develop [2]. Despite the contributions from such methods, it is likely to be confused with other conditions mimicking AA in a significant number of patients, which may complicate accurate diagnosis. It can be difficult to diagnose, especially in children, premenopausal women, the elderly, and those with other inflammatory diseases. In previous studies, perforation in 20% of the patients and negative laparotomy at higher rates such as 20%–30% were reported after the diagnosis of AA performed with the help of physical examination and symptoms [3]. One of the most confusing conditions with AA during physical examination, abdominal USG, as well as intrasurgical interventions, is reactive lymphoid hyperplasia (RLH), a cellular response to viral infections as a common pathologic finding from fine-needle aspirates and core biopsies of peripheral lymph nodes from parenchymal lung and mediastinal lymph node biopsies. RLH can also develop in the appendix. When the lymph nodes in the appendix encounter viral agents, inflation begins in the region, and the lymph nodes enlarge in size. Such a situation can be confused with AA; and if it can be diagnosed at an early period, RLH is a condition that can be cured with medical treatment with no need for surgical interventions [45]. In the present study, we aimed to compare patients with histological diagnoses of AA and RLH, and who underwent surgery due to the diagnosis of AA in terms of the laboratory, clinical, and demographic characteristics.
This study was approved by the Ethics Committee of Baskent University Medical and Health Sciences Research Council (No. K15/288). The need for informed consent was waived due to the retrospective nature of the study. The principles set out in the 1964 Helsinki Declaration and its later amendments were followed.
The study designed retrospectively was conducted by scanning the hospital records of the patients undergoing appendectomy between 2015 and 2020. A total of 189 patients previously diagnosed with AA and operated on due to the findings on abdominal USG performed in the emergency department were included in the study. The pathology reports of the patients were scanned, and patients’ scores of age, sex, preoperative complete blood count (CBC) parameters, including WBC count, red cell distribution width (RDW), mean platelet volume (MPV), neutrophil (Neu), lymphocyte (Lym), monocyte (Mono), thrombocyte (Thromb), eosinophil, NLR, CRP, and appendiceal specimens diagnosed histopathologically were obtained from patients’ hospital records. After scanning the data, the patients were classified into 2 groups: 1 group diagnosed with appendicitis and the other with hyperplasia. Among our subjects, those using analgesic drugs, exposed to blood transfusion or other blood products, with uncontrolled hypertension, intracranial space-occupying lesion, treated due to anemia or polycythemia within the last year, those with a history of hemorrhages, hematologic disorders, chronic kidney or liver diseases, the history of pregnancy or fever in the last 1 month, any other disorders such as oncologic diseases, iron deficiency anemia, thalassemia, a metabolic disorder, and antiinflammatory bowel disease, and those undergoing operations during the last 6 months were excluded from the study.
All statistical analyses were implemented through the R statistical software ver. 4.0.4 (R Foundation for Statistical Computing, Vienna, Austria; https://www.r-project.org) [6]. The Kolmogorov-Smirnov and Shapiro-Wilk tests were used for evaluating the normal distribution of the data. The Levene test was utilized to check the variance homogeneity of the groups. The variables are presented as the median, range, and interquartile range, and the differences between the variables were evaluated by the Mann-Whitney U-test. Furthermore, the Spearman correlation analysis was conducted to examine the relationship between the variables. A P-value of <0.05 was considered statistically significant.
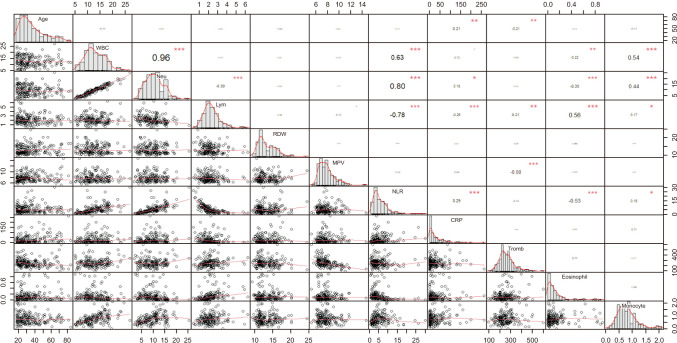
The present study was composed of a total of 187 patients (152 with appendicitis and 35 with hyperplasia) and consisted of 88 female patients (47.1%; 74 in the appendicitis group and 14 in the hyperplasia group) and 99 male patients (52.9%; 78 in appendicitis group and 21 in hyperplasia group) with a median 31 years of age (range, 17–84 years). The demographic and laboratory findings of the patients in each group are shown in Table 1 and Fig. 1. While the scores of age, WBC, Neu, NLR, and CRP were found to be significantly higher in the appendicitis group than those in the hyperplasia group, the rates of Lym and eosinophil were detected to be lower in the appendicitis group than that in the hyperplasia group (P < 0.05). On the other hand, no statistically significant difference was determined between appendicitis and hyperplasia groups in terms of the rates of RDW, MPV, Thromb, and Mono (P > 0.05). The Spearman correlation analysis was conducted to examine the relationships between the variables, and the findings are presented by the correlation matrix in Fig. 2. The correlation matrix reveals the distribution of each variable on the diagonal, and there are bivariate scatter plots with a fixed line on the bottom of the diagonal. The correlation values and significance levels as stars are above the diagonal. As seen in Fig. 2, there was a correlation of 21% between age and CRP, and an inverse correlation of 21% between age and Thromb; there were also correlations of 96%, 63%, and 54% between WBC and Neu, NLR, and Mono, respectively. On the other hand, an inverse correlation of 22% was detected between the scores of WBC and eosinophils; in addition, there were correlations of 80%, 18%, and 44% between the scores of neutral and NLR, CRP, and Mono, respectively. Even so, inverse correlations of 30% between neutral and Lym and 35% between neutral and eosinophils were detected. Moreover, inverse correlations of 78% and 26% were observed between Lym and NLR, and lymph and CRP, respectively. There were also correlations of 21%, 56%, and 17% between Lym and Thromb, eosinophils, and Mono, respectively. There was an inverse correlation of 50% between MPV and Thromb. The rates of the correlations between NLR and CRP, and NLR and Mono were detected as 29% and 18%, respectively. There was an inverse correlation of 53% between NLR and eosinophils.
Since AA is a common surgical emergency across the world, appendectomy is also one of the most frequently performed surgical procedures and imposes a significant burden on health systems around the world [67].
Luminal obstruction of the appendix progresses to suppurative inflammation, resulting in extensive peritonitis or abscess of appendicitis. Among the classical features, periumbilical pain progressing to the right iliac fossa, nausea, vomiting, fever, and tenderness in the right lower quadrant may be regarded [8]. In our study, the patients were detected to be admitted with such complaints as abdominal pain, periumbilical pain spreading to the right lower quadrant, nausea, and vomiting. The pathophysiology of AA is characterized by the obstruction of the lumen, by a fecalith, a foreign body, and parasites [9].
Lymphoid hyperplasia (LH) is a cellular reaction developing against viral infections anywhere in the body (i.e., the lymph nodes in the neck, abdomen, tonsils, and adenoids). Lymphoid tissue also is normally present in the appendix [5]. For the first time, clinicians recognized LH of the appendix as a clinical entity in the early 20th century. LH may result in a noncompressible appendix with a diameter of 6–8 mm and be misdiagnosed as appendicitis in pediatric patients. True-positive diagnoses of appendicitis can be accurately performed through the existence of at least 2 additional findings from the group of periappendiceal fluid, hyperechoic periappendiceal fat, and mural hyperemia. Identifying the characteristic sonographic appearance of LH may help prevent the false-positive misdiagnoses of appendicitis [10].
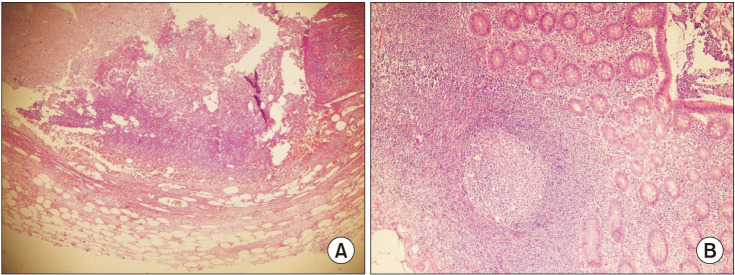
LH of the appendix is typically associated with inflammatory conditions such as viral gastroenteritis and mesenteric adenitis and is often seen in the pediatric age group [11]. In the USG of RLH involving the appendix, false-positive findings that will cause the outer diameter to enlarge by 6 cm or more are encountered, and such findings may be confused with AA [1012]. Therefore, many patients diagnosed with RLH may undergo appendectomy, raising in turn the rate of appendectomy negatively. The fact that many patients with RLH undergo appendectomy is a reason for increasing the rate of negative appendectomy [13]. It is very important to distinguish between these 2 conditions before appendectomy to avoid unnecessary surgical interventions and ease the financial burden on countries’ health budgets. In the literature, several studies have been carried out so far to enlighten the issue. In one of those studies where USG images and histopathological findings were compared, it was concluded that the USG findings alone would not be effective, but would be more meaningful together with clinical and laboratory findings [4]. The histopathological appearances of AA and LH have determined that they are different from each other in previous studies, and it has been observed that there is dominance of neutrophils in the microscopic appearance of AA [14]. In our study, the histopathological appearances of AA and LH were also different (Fig. 3). LH of the appendix is most commonly identified in pediatric patients and is typically associated with inflammatory conditions, such as viral gastroenteritis and mesenteric adenitis [11]. In a study in which the age rates of AA and LH patients were compared, it was seen that there was no difference between the 2 groups [13]. In our study, however, the mean age of the patients with RLH was found to be lower than those with AA, and the difference was considered statistically significant. Based on the literature, the number of studies comparing age rates is limited, and this is a feature that makes our study intriguing. Based on the literature, the number of studies comparing the laboratory markers between the AA and LH patients was seen to be insufficient. In one study, it was determined that the leukocyte and Neu counts were higher in the patients with AA, compared to those with LH, and Lym count was higher in the LH group [4]. In another study, while the WBC and Neu counts were determined to be higher in the patient with AA than in the LH group, Lym count was found to be lower. In the same study, NLR was also stated to be higher in patients with AA [13]. As consistent with the findings in the literature, it was also found in our study that the rates of WBC, Neu, and NLR were higher in the AA patient group than those with RLH. Lym count was found to be higher in the group with LH, however. In our study, it was determined that the number of eosinophils was higher in the patients with RLH, and the difference was considered statistically significant. To the best of our knowledge, the present study is the first to compare AA with RLH in the context of eosinophils alone. There are many studies in the literature investigating the course of NLR in AA. NLR has been investigated further among all blood markers in recent years, and NLR is likely to be a better marker for AA, compared with leukocytes and Neu counts. In numerous studies, it has been determined that NLR is increased in AA [151617]. In our study, the rate of NLR was also witnessed to be increased among the patients in the appendicitis group. In light of the literature, only 1 study was current, evaluating the changes of NLR in the patients with LH and AA; in the study, NLR was determined to be lower in the LH group than in those with AA [13]. In our study, the NLR value was found to be higher in the AA group than those in the RLH group. CRP is a sensitive acute phase reactant and appears as an increased marker in acute inflammatory processes. It is known that the level of CRP increases in proportion to the severity and duration of the inflammation. Based on the literature, several studies are revealing the importance of the CRP level in the diagnosis and prognosis of AA [1819]. In a previous study, the level of CRP was also detected to be significant in determining the duration of AA symptoms and surgery [20]. There are no studies investigating CRP values by comparing LH and AA patients. In our study, the CRP levels were found to be significantly higher in the group AA, compared to those in the RLH group. However, there are some limitations of the present study, such as the retrospective design and the small number of study participants.
In conclusion, the pathogenesis of AA and RLH are 2 different conditions, and thus it is of vital importance to make a differential diagnosis of both diseases before any surgical intervention. We consider that CBC and CRP can be a guide in distinguishing between both diseases, and that more comprehensive randomized studies including larger populations may provide more detailed and clearer evidence to elucidate each entity.
References
1. Andersson RE. Meta-analysis of the clinical and laboratory diagnosis of appendicitis. Br J Surg. 2004; 91:28–37. PMID: 14716790.

2. McGowan DR, Sims HM, Zia K, Uheba M, Shaikh IA. The value of biochemical markers in predicting a perforation in acute appendicitis. ANZ J Surg. 2013; 83:79–83. PMID: 23231057.

3. Sengupta A, Bax G, Paterson-Brown S. White cell count and C-reactive protein measurement in patients with possible appendicitis. Ann R Coll Surg Engl. 2009; 91:113–115. PMID: 19102827.

4. Sheridan AD, Ehrlich L, Morotti RA, Goodman TR. Sonographic distinction between acute suppurative appendicitis and viral appendiceal lymphoid hyperplasia (“pink appendix”) with pathological correlation. Ultrasound Q. 2015; 31:95–98. PMID: 25945725.

5. Swischuk LE, Chung DH, Hawkins HK, Jadhav SP, Radhakrishnan R. Non-fecalith-induced appendicitis: etiology, imaging, and pathology. Emerg Radiol. 2015; 22:643–649. PMID: 26293120.

6. Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015; 386:1278–1287. PMID: 26460662.

7. Stewart B, Khanduri P, McCord C, Ohene-Yeboah M, Uranues S, Vega Rivera F, et al. Global disease burden of conditions requiring emergency surgery. Br J Surg. 2014; 101:e9–e22. PMID: 24272924.

10. Xu Y, Jeffrey RB, DiMaio MA, Olcott EW. Lymphoid hyperplasia of the appendix: a potential pitfall in the sonographic diagnosis of appendicitis. AJR Am J Roentgenol. 2016; 206:189–194. PMID: 26700351.

11. Rabah R. Pathology of the appendix in children: an institutional experience and review of the literature. Pediatr Radiol. 2007; 37:15–20. PMID: 17031635.

12. Goldin AB, Khanna P, Thapa M, McBroom JA, Garrison MM, Parisi MT. Revised ultrasound criteria for appendicitis in children improve diagnostic accuracy. Pediatr Radiol. 2011; 41:993–999. PMID: 21409546.

13. Kaya A, Karaman K, Aziret M, Ercan M, Köse E, Kahraman YS, et al. The role of hematological parameters in distinguishing acute appendicitis from lymphoid hyperplasia. Ulus Travma Acil Cerrahi Derg. 2022; 28:434–439. PMID: 35485518.

14. Yilmaz M, Akbulut S, Kutluturk K, Sahin N, Arabaci E, Ara C, et al. Unusual histopathological findings in appendectomy specimens from patients with suspected acute appendicitis. World J Gastroenterol. 2013; 19:4015–4022. PMID: 23840147.

15. Markar SR, Karthikesalingam A, Falzon A, Kan Y. The diagnostic value of neutrophil: lymphocyte ratio in adults with suspected acute appendicitis. Acta Chir Belg. 2010; 110:543–547. PMID: 21158332.

16. Kahramanca S, Ozgehan G, Seker D, Gökce EI, Seker G, Tunç G, et al. Neutrophil-to-lymphocyte ratio as a predictor of acute appendicitis. Ulus Travma Acil Cerrahi Derg. 2014; 20:19–22. PMID: 24639310.

17. Goodman DA, Goodman CB, Monk JS. Use of the neutrophil:lymphocyte ratio in the diagnosis of appendicitis. Am Surg. 1995; 61:257–259. PMID: 7887542.
18. Hallan S, Asberg A, Edna TH. Additional value of biochemical tests in suspected acute appendicitis. Eur J Surg. 1997; 163:533–538. PMID: 9248988.
19. Narci H, Turk E, Karagulle E, Togan T, Karabulut K. The role of red cell distribution width in the diagnosis of acute appendicitis: a retrospective case-controlled study. World J Emerg Surg. 2013; 8:46. PMID: 24216220.

20. Cho J, Lee D, Sung K, Baek J, Lee J. Clinical implication of discrepancies between surgical and pathologic diagnoses of acute appendicitis. Ann Surg Treat Res. 2017; 93:43–49. PMID: 28706890.

Fig. 1
Comparison of groups according to the demographic and laboratory findings (patients with appendicitis and hyperplasia). Neu, neutrophil; Lym, lymphocyte; RDW, red cell distribution width; MPV, mean platelet volume; NLR, neutrophil/lymphocyte ratio.
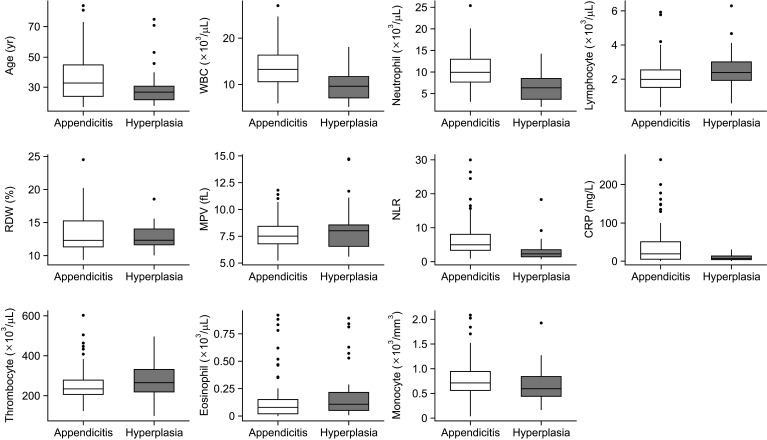
Fig. 2
The correlation matrix. Neu, neutrophil; Lym, lymphocyte; RDW, red cell distribution width; MPV, mean platelet volume; NLR, neutrophil/lymphocyte ratio; Tromb, thrombocyte. *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download