Abstract
Purpose
Sacrococcygeal pilonidal disease is a chronic inflammatory condition with an incidence of 26:100,000 in the United States. However, its etiology and optimal treatment remain controversial.
Methods
We included 129 and 74 patients with simple and complex sacrococcygeal pilonidal disease, respectively. The primary outcome was pilonidal sinus recurrence after unroofing curettage. Secondary outcomes were pain scores, time to return to work/school, and time to complete recovery.
Results
At a median follow-up of 53 months, the recurrence rate was 4.9% in all patients, not significantly higher in subjects with the complex disease. Duration of surgery (15.4 minutes vs. 12.2 minutes), time to return to school/work (9.8 days vs. 7.7 days), and complete healing time (44 days vs. 36 days) were longer in patients with the complex disease. Postoperative complication rates, pain scores, and quality of life scores between the 2 groups did not differ.
Go to : 
Sacrococcygeal pilonidal disease (SPD) is a well-recognized chronic inflammatory condition that affects young adults; its estimated incidence in the United States is 26 per 100,000 population. The etiology and optimal treatment of this disease, which is commonly encountered in clinical practice, have been controversial since Mayo first described it in 1833 [12]. SPD is an umbrella term for different disease stages ranging from asymptomatic simple midline pits or sinus orifices to complex chronically inflamed cavities with multiple fistula tracts to treatment failure [3]. Different stages of the disease may be appropriate for different treatment modalities [4].
Currently, there are numerous treatment options ranging from non-surgical methods to extensive flap procedures [2]. However, overly elaborate treatment strategies may turn this easily treatable disease into a long-term surgical ordeal, causing worse complications than the primary disease itself [45]. The most likely and expected outcome is an early discharge from hospital after surgery, a prompt return to school or work, and a low probability of recurrence.
The most important long-term cause for concern when treating SPD is recurrence, and previous evidence suggests that unroofing curettage (UC) is associated with a low recurrence rate in patients with SPD despite this procedure’s average recovery period of 7 weeks [36]. However, while UC is considered safe and effective for treating simple SPD, its suitability for treating complex SPD remains undermined and controversial.
This study aimed to investigate the outcomes of patients who underwent UC as the primary intervention for simple or complex SPD. To the best of our knowledge, this study is the first to determine and compare the efficacies and outcomes post-UC in patients categorized into simple versus complex SPD groups.
Go to : 
We performed a prospective observational study conducted at the Department of Surgery of the Diskapi Training and Research Hospital in Ankara, Turkey. The local ethics committee of the institution approved the study protocol (No. 27/02, dated March 22, 2016), and written informed consent was obtained from all participants. The trial was registered with ClinicalTrials.gov (NCT05339828). The study protocol was devised according to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines [7]. The study was performed in accordance with the ethical standards laid down in the Declaration of Helsinki.
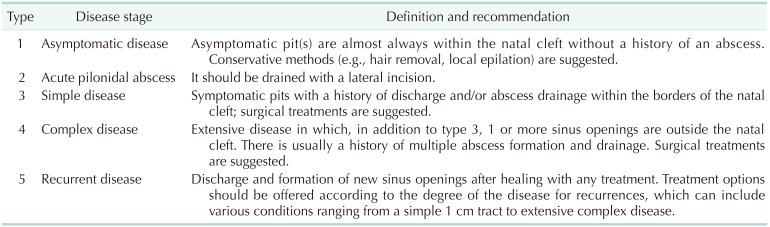
Consecutive patients aged 18 years or older who applied for simple and complex SPD treatment between April 2016 and September 2018 and preferred the UC surgery from among the treatment options (e.g., phenol application, open healing modalities, midline, and off-midline closure methods) offered by the physician blind to research, were considered eligible. There is no universally accepted classification system for the different stages of SPD [3]. This study used Tezel’s classification system for patient selection and enrollment, which covers all stages of the disease (Table 1) [8]. Accordingly, simple SPD was defined as symptomatic sinus orifice(s) within the natal cleft boundaries. Complex SPD was defined as multiple pits and multiple fistula tracts on and outside the natal cleft. Asymptomatic SPD patients were recommended conservative methods (e.g., hair removal, local epilation) and excluded from the study. Recurrences, including various conditions ranging from a simple 1-cm tract to extensive complex disease, were excluded because they were in a different category. In addition, patients with acute pilonidal abscess, uncontrolled diabetes mellitus, immunosuppressive or coagulation disorders, pregnancy and/or lactation, and/or other acute surgical diseases were excluded.
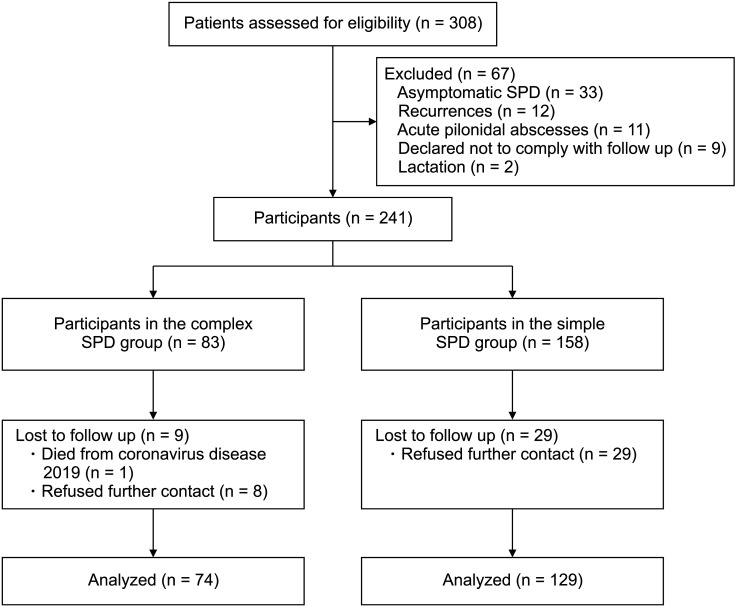
There was no sample size evaluation based on power analysis. Rather, we evaluated all patients diagnosed with SPD at an outpatient clinic for potential enrollment during the study period. Of the 308 consecutive patients assessed for eligibility, 241 met the inclusion criteria. After 38 of these patients were lost to follow-up, data from 203 individuals were analyzed; their details are shown in Fig. 1.
Each participant underwent detailed clinical history documentation and was subjected to a thorough physical examination. The following demographic and clinical data were recorded on the patient follow-up form: age, sex, body mass index (BMI), smoking status, comorbidities (diabetes mellitus, hypertension, coronary artery disease, chronic obstructive lung disease, renal failure, and autoimmune diseases), previous abscess drainage, number of primary and secondary sinus orifices, widest diameter of the sinus, preoperative visual analog scale (VAS) pain score, and duration of surgery.
The primary outcome measure of the study was recurrence, while the secondary outcome measures were the VAS scores for pain, time to return to work or school, and complete healing time.
All procedures comprised outpatient surgeries, and antibiotic prophylaxis was not administered. Surgery was performed with the patient lying in the prone position under local anesthesia. The nursing team shaved the surgical site; thereafter, adhesive tapes were used to pull the buttocks apart laterally and expose the intergluteal sulcus. A povidone-iodine solution was used for surgical site disinfection. Next, a local anesthetic agent comprising a solution of lidocaine (20 mg/mL) and adrenaline (Jetokain, 0.0125 mg/mL; Adeka İlaç Sanayii, Istanbul, Turkey) was diluted with distilled water in a 1:2 ratio and injected. The tract was identified by passing small artery forceps along its length and was then opened by cutting directly down onto the forceps. The sinus and all its tracts were completely unroofed, and the base was curetted to remove all necrotic content, hair, and granulation tissue using a dry gauze. The fibrotic back wall was left as intact as possible to avoid delayed healing. Hemostasis was achieved using diathermy with no drainage needed. The open wound was covered with a simple dressing comprising gauze soaked to saturation with 0.9% sodium chloride [9].
Unlike some other surgeries, our UC method did not include marsupialization and excision of the wound edges, as these would prolong surgery and increase postoperative pain. Moreover, marsupialization sutures can be spontaneously pulled after surgery. We did not cut the wound edges to prevent early bridging (as some surgeons do) because frequent dressing of the wound is sufficient to prevent premature bridging [6].
The surgeon who performed the UC procedure was excluded from data collection. Additionally, the researcher evaluating the postoperative follow-up and outcomes was blind to patient enrollment. All patients were discharged on the same day as the procedure and were prescribed an analgesic containing diclofenac sodium (50 mg, twice a day) within safe dosing limits if they experienced pain. The physician changed the dressings in the outpatient clinic for the first 3 days, during which the dressing technique was taught to the patients’ relatives, who would then perform daily dressings at home. After irrigation with 10 mL of 0.9% sodium chloride once a day, the end of dry gauze was packed inside the wound, and the dressing was changed. Thereafter, the physician checked the wound during weekly visits to the outpatient clinic, whereupon the early skin bridges were separated and dressed. The gluteal area was kept devoid of hair during the first year with home use of a depilatory cream by the patients.
The extent of pain was evaluated by determining the VAS score at 24 and 48 hours after surgery. The patients maintained a diary in which any pain experienced with each dressing was scored (VAS, 0–100 mm). After completing recovery, the mean VAS score was recorded in each patient’s follow-up record.
Due to the lack of regular dressing, the formation of epithelial bridges between the wound edges while the cavity is empty before complete healing was defined as early bridging. Healing time was calculated as the interval between surgery and complete epithelialization and wound closure. Patients were summoned to the hospital in the second month to document time to pain-free walking, time to pain-free sitting, and the time to return to work or school using a specially designed questionnaire. The Short Form-36 Health Survey (SF-36) was also administered during this visit to assess the quality of life (QoL).
Subsequent follow-ups were performed at 3, 6, 12, 24, 36, 48, and 60 months after surgery. Additionally, the patients were told to contact us in the event of any new symptoms related to their wounds. After healing was complete, any new sinus orifice or discharge from the wound was defined as disease recurrence.
IBM SPSS Statistics for Windows ver. 22.0 (IBM Corp, Armonk, NY, USA) was used for statistical analysis. The Mann-Whitney U-test was used to compare measured variables between groups. The chi-square and Fisher exact tests were used to analyze the relationships between categorical variables or differences between groups. Qualitative variables are presented as frequencies (percentages), while quantitative variables are presented as means (±standard deviations) or medians (minimum-to-maximum). The relationship between VAS pain scores and QoL was examined using the Spearman rank correlation test. Univariate logistic regression analysis was performed to identify risk factors for recurrence. Accordingly, variables with a significance level of 0.25 or lower were subjected to multivariate logistic regression analysis, in which the associated odds ratio, 95% confidence intervals, and P-values were calculated. A P-value of <0.05 was considered statistically significant.
Go to : 
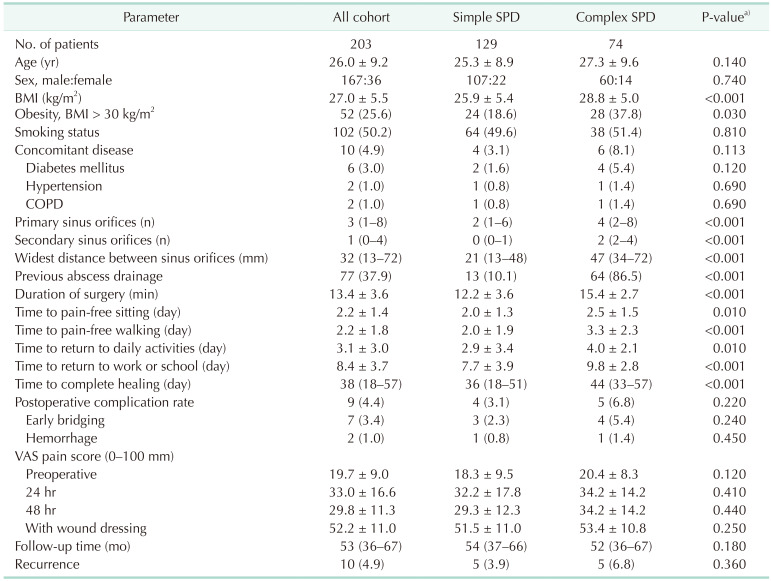
The mean age of the patients was 26 ± 9.2 years, and 82.3% of the patients were male. The mean BMI was 27 ± 5.5 kg/m2, and 25.6% of the patients were obese (BMI of >30 kg/m2). Moreover, 50.2% of the patients were current smokers, and 4.9% had a concomitant disease, as shown in Table 2. The number of patients with simple and complex SPD was 129 and 74, respectively (10:6 ratio). Other clinical features are presented in Table 2.
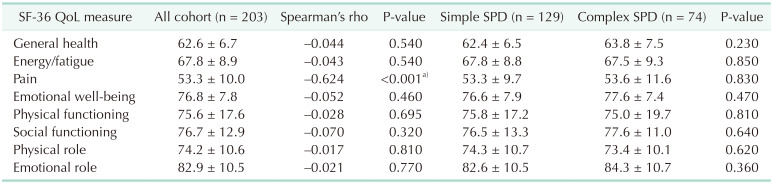
The mean duration of surgery was 13.4 ± 3.6 minutes, whereas the mean durations to pain-free sitting, pain-free walking, return to daily activities, and return to work or school were 2.2 ± 1.4 days, 2.2 ± 1.8 days, 3.1 ± 3 days, and 8.4 ± 3.7 days, respectively. The rate of postoperative complications (none of which required hospitalization) was 4.4%. Of the 9 patients with complications, 2 had a hemorrhage in the first 24 hours postoperatively, were taken back to the operating room, and treated with hemostasis and dressing, while 7 experienced early bridging and were treated with wound debridement and dressing at the outpatient clinic. The time to complete healing was 38 days (Table 2). There was a significant negative correlation between the VAS pain scores with dressing and the QoL scores for pain at the end of 2 months per the Spearman rank correlation test; although the VAS pain score with dressing was also negatively correlated with other QoL indicators, none of these associations were significant (Table 3). The median follow-up time was 53 months (range, 36–67 months), during which time 10 patients (4.9%) experienced recurrence (Table 2). Seven recurrences were detected between 18 and 36 months and 3 between 40 and 57 months. Among them, 5 patients were treated with UC, 3 with Limberg flap, and 2 with crystallized phenol. During the follow-up period, none of the patients in the study group had a persistent (non-healing) pilonidal disease.
The comparisons of the outcomes of patients with simple versus complex SPD are presented in Table 2. Obesity (i.e., BMI of >30 kg/m2), number of primary and secondary sinus orifices, the widest distance between sinus orifices, and previous abscess drainage rate were significantly higher among patients with complex SPD than among those with simple SPD. Moreover, the duration of surgery, the durations to pain-free sitting, pain-free walking, return to daily activities, and return to work or school and complete healing time were significantly longer among patients with complex SPD. There were no significant differences in postoperative complication rates and VAS pain scores between patients with simple versus complex SPD; the rate of recurrence was higher in the latter group, albeit not significantly (6.8% vs. 3.9%, P = 0.360) (Table 2). Six of 10 recurrences had early bridging in the healing process. No recurrence was observed in 1 patient who had early epithelial bridges cleaned by the physician and had regular dressing in the next follow-up period. Comparative QoL scores of patients with simple versus complex SPD 2 months after surgery were similar (Table 3).
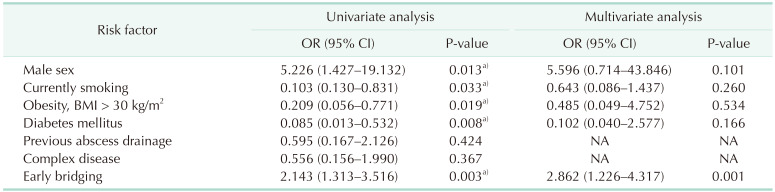
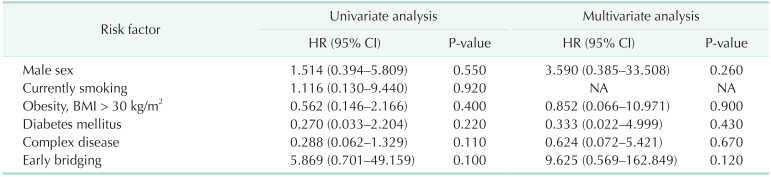
On univariate logistic regression analysis of UC in patients with simple versus complex SPD, obesity (i.e., BMI of >30 kg/m2), diabetes mellitus, and early bridging were found to be risk factors for recurrence. However, only early bridging was significant in multivariate analysis (Table 4). There was no statistical significance in the Cox proportional hazards model used to define the factors related to the recurrence time (Table 5).
Go to : 
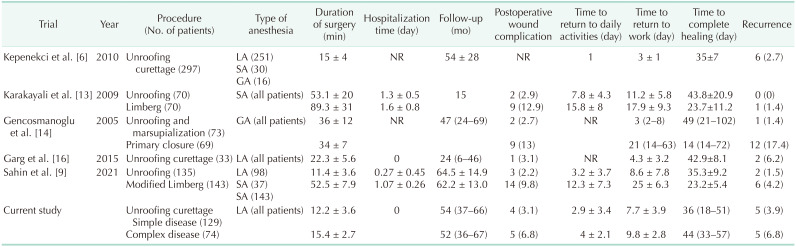
Young and otherwise healthy patients who are made to undergo surgical procedures that may result in significant morbidity for SPD can experience a heavy socioeconomic burden as a result [10]. The ideal surgical method should be simple, short, cause minimal pain, require short or no hospitalization, involve effortless after surgical care, allow a prompt return to work and daily activities, not significantly affect QoL, have a low recurrence rate, and be cost-effective [10]. UC meets most of the aforementioned criteria. Various cohort and comparative studies that support this opinion and demonstrate the effectiveness of UC are listed in Table 6.
Our prospective observational study analyzed data from a cohort of 203 patients who underwent UC for the surgical treatment of simple and complex SPD. Although flap methods are associated with lower recurrence rates than primary closure, open healing techniques are routinely used in our practice [11]. Additionally, a systematic review by McCallum et al. [12] found that the recurrence rate with open healing was 58% lower than that following primary closure.
The median complete healing time in our cohort was 38 days; this period ranged from 35 to 49 days in previous prospective trials [61314], and Garg et al. [15] revealed complete healing times of 21–72 days in their meta-analysis. In our study, the mean duration of surgery (13.4 minutes) was shorter than the 15–53 minutes duration range in previous trials [6131416]. Since we did not add procedures such as marsupialization and excision of the wound edges to UC, we attribute that to shorter surgical time. Previous trials also revealed postoperative complication rates between 0% and 2.9% [61314], but this rate was 4.4% in the present study. Garg et al.’s [15] meta-analysis found these rates to be between 0% and 5.6%.
Our study also showed improved outcomes after UC, including no hospitalization, shorter operation time, and earlier return to daily activities. The VAS pain scores were low at 24 and 48 hours postoperatively, although they were high for dressing changes (illustrating one of the disadvantages of UC). Per the SF-36 QoL questionnaire conducted 2 months after surgery, patients who underwent UC reported more pain due to dressing changes, but their social and physical functions were not affected.
Comparing patient outcomes was important for demonstrating the usefulness of UC for treating simple and complex SPD. Our data showed that the mean operative time (15.4 minutes vs. 12.2 minutes), time taken to pain-free sitting (2.5 days vs. 2 days), time taken to pain-free walking (3.3 days vs. 2 days), time taken to return to work (9.8 days vs. 7.7 days), and complete healing time (44 days vs. 36 days) were significantly longer in patients with complex SPD than in those with simple SPD. However, compared with the current evidence, these durations were acceptable for both groups (Table 6). Additionally, the VAS pain and QoL scores in the 2 groups were similar. While the recurrence rate was 4.9% among all cohort patients, it tended to be higher among those with complex SPD than among their counterparts with simple SPD, although the difference was not significant (6.8% vs. 3.9%, P = 0.360). Previous studies revealed recurrence rates between 0% and 2.4% following UC [61314], while Garg et al.’s [15] meta-analysis found these rates to be between 0% and 10%. Our results are consistent with their data; however, our findings that the healing time was longer for patients with complex SPD and that the recurrence rate was higher comprise novel information in the field of UC. Our multivariate analysis revealed that the risk factor for recurrence was early bridging (Table 4). The leading cause of recurrence, early skin bridging, can be prevented with regular dressings at weekly physician visits [6]. Six of 10 recurrence patients were patients with early bridging because they did not have regular dressings. In our study, early bridging was an independent risk factor for recurrence; before the healing was completed, the early epithelial bridges formed when the cavity was empty thereby were forming new pilonidal sinus cavities. In the Cox proportional hazards model, the correlation between the recurrence time and the male sex and early bridging was not statistically significant (Table 5).
According to our data, the UC procedure had a success rate of 95.1% in all patients, including 96.1% in those with simple SPD and 93.2% in those with complex SPD. Thanks to the UC method, none of the SPD patients, mostly young and active, had to take a 1-week antibiotic treatment and rest for 2–3 weeks, away from work and school [17]. Wide local excision and flap procedures have high morbidity and long operation time, hospital stay, and time to return to work, school, and daily activities (Table 6) [18]. UC is a simple and straightforward procedure, and based on our findings, may be a good first-choice surgical option for simple SPD. Conversely, flap-based methods may be preferred for patients with complex chronic pilonidal diseases and those who experience multiple recurrences after other techniques have failed. Our data support a “strong recommendation” based on moderate-quality evidence 1B in terms of the grade of recommendation [2]. Patients with complex SPD can also undergo UC as their initial surgical treatment if both the patient and physician concur. Based on the aforementioned recommendation level, flap-based methods may be preferable if the SPD recurs after UC in patients with complex SPD [2].
Published studies on the outcomes of patients with complex SPD as a separate group were unidentified prior to investigation. To the best of our knowledge, our study is the first to determine the efficacy and outcomes of UC in patients with simple and complex SPD separately.
Our study had some limitations, including the fact that our patients were not randomized. Moreover, patients with simple SPD outnumbered those with complex SPD (129 vs. 74). Future prospective randomized studies comparing UC with other open healing modalities in treating simple and complex SPD may contribute to further research on optimal surgical techniques.
In conclusion, the promising outcomes of the patients in our study who underwent UC indicate that this procedure could potentially be a first-choice treatment option for both simple and complex SPD.
Go to : 
References
1. Mayo OH. Observations on injuries and diseases of the rectum. London: Burgess and Hill;1883. p. 45–46.
2. Steele SR, Perry WB, Mills S, Buie WD. Standards Practice Task Force of the American Society of Colon and Rectal Surgeons. Practice parameters for the management of pilonidal disease. Dis Colon Rectum. 2013; 56:1021–1027. PMID: 23929010.

3. Beal EM, Lee MJ, Hind D, Wysocki AP, Yang F, Brown SR. A systematic review of classification systems for pilonidal sinus. Tech Coloproctol. 2019; 23:435–443. PMID: 31098861.

4. Gecim IE, Goktug UU, Celasin H. Endoscopic pilonidal sinus treatment combined with crystalized phenol application may prevent recurrence. Dis Colon Rectum. 2017; 60:405–407. PMID: 28267008.

5. Harries RL, Alqallaf A, Torkington J, Harding KG. Management of sacrococcygeal pilonidal sinus disease. Int Wound J. 2019; 16:370–378. PMID: 30440104.

6. Kepenekci I, Demirkan A, Celasin H, Gecim IE. Unroofing and curettage for the treatment of acute and chronic pilonidal disease. World J Surg. 2010; 34:153–157. PMID: 19820992.

7. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007; 370:1453–1457. PMID: 18064739.

8. Tezel E. A new classification according to navicular area concept for sacrococcygeal pilonidal disease. Colorectal Dis. 2007; 9:575–576. PMID: 17573759.

9. Sahin A, Simsek G, Arslan K. Unroofing curettage versus modified limberg flap in pilonidal disease: a retrospective cohort study. Dis Colon Rectum. 2022; 65:1241–1250. PMID: 34840296.

10. Calikoglu I, Gulpinar K, Oztuna D, Elhan AH, Dogru O, Akyol C, et al. Phenol injection versus excision with open healing in pilonidal disease: a prospective randomized trial. Dis Colon Rectum. 2017; 60:161–169. PMID: 28059912.

11. Stauffer VK, Luedi MM, Kauf P, Schmid M, Diekmann M, Wieferich K, et al. Common surgical procedures in pilonidal sinus disease: a meta-analysis, merged data analysis, and comprehensive study on recurrence. Sci Rep. 2018; 8:3058. PMID: 29449548.

12. McCallum IJ, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ. 2008; 336:868–871. PMID: 18390914.

13. Karakayali F, Karagulle E, Karabulut Z, Oksuz E, Moray G, Haberal M. Unroofing and marsupialization vs. rhomboid excision and Limberg flap in pilonidal disease: a prospective, randomized, clinical trial. Dis Colon Rectum. 2009; 52:496–502. PMID: 19333052.

14. Gencosmanoglu R, Inceoglu R. Modified lay-open (incision, curettage, partial lateral wall excision and marsupialization) versus total excision with primary closure in the treatment of chronic sacrococcygeal pilonidal sinus: a prospective, randomized clinical trial with a complete two-year follow-up. Int J Colorectal Dis. 2005; 20:415–422. PMID: 15714292.

15. Garg P, Menon GR, Gupta V. Laying open (deroofing) and curettage of sinus as treatment of pilonidal disease: a systematic review and meta-analysis. ANZ J Surg. 2016; 86:27–33. PMID: 26612320.

16. Garg P, Garg M, Gupta V, Mehta SK, Lakhtaria P. Laying open (deroofing) and curettage under local anesthesia for pilonidal disease: an outpatient procedure. World J Gastrointest Surg. 2015; 7:214–218. PMID: 26425271.

17. Abbas MA, Tejerian T. Unroofing and marsupialization should be the first procedure of choice for most pilonidal disease. Dis Colon Rectum. 2006; 49:1242. PMID: 16826329.
18. Dogan S, Cetin F, Gurleyik E. Inverse ‘D’ incision technique in treatment of pilonidal sinus disease; excision with minimal tissue loss, closure without tension and lateral location of the suture line. Ann Surg Treat Res. 2019; 97:261–265. PMID: 31742211.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download