INTRODUCTION
The burden of cardiovascular diseases (CVDs) has remained the leading cause of global deaths and disability despite the considerable effort of mitigation.
1) Sustainable Development Goals from the United Nation aimed to reduce premature deaths from non-communicable diseases including CVDs by 2030, and CVD mortality rates had substantially decreased over the past decades.
2) Population aging and growth, however, have offset these improvements as age is highly associated with a greater incidence and fatality of CVDs.
3)4) The mortality appears to be stagnant or slightly increased in recent years.
5)6)
This static global rate masked wide regional variation of CVD incidence and mortality.
2)7) The CVD mortality in Africa was lower than in other regions and continued to decrease. On the contrary, the figures in Europe and America had been the most significant and increased again following the substantial reduction until the early 2010s. The burden in the Asia region was aggravated from 175.49 deaths per 100,000 population in 1990 to 237.85 per 100,000 in 2019.
7) These different trends reflect changes in its underlying causes in regions such as the prevalence of CVD risk factors and access to health care along with population structure.
5)8)
Geographical variations in CVD mortality have also been reported within a country
9): for instance, notable differences in deaths from CVDs were observed between counties in the United States while presenting a higher burden in certain regions.
10) China showed a concentrated CVD mortality in the northern part (Beijing) compared to the southern part (Shanghai and Guangzhou).
9)11) Likewise, northern England and southeastern Spain showed higher death rates from CVDs than other regions in each country.
12)13)
In Korea, the CVD burden is still high: heart diseases and cerebrovascular diseases had accounted for most of the deaths following cancer.
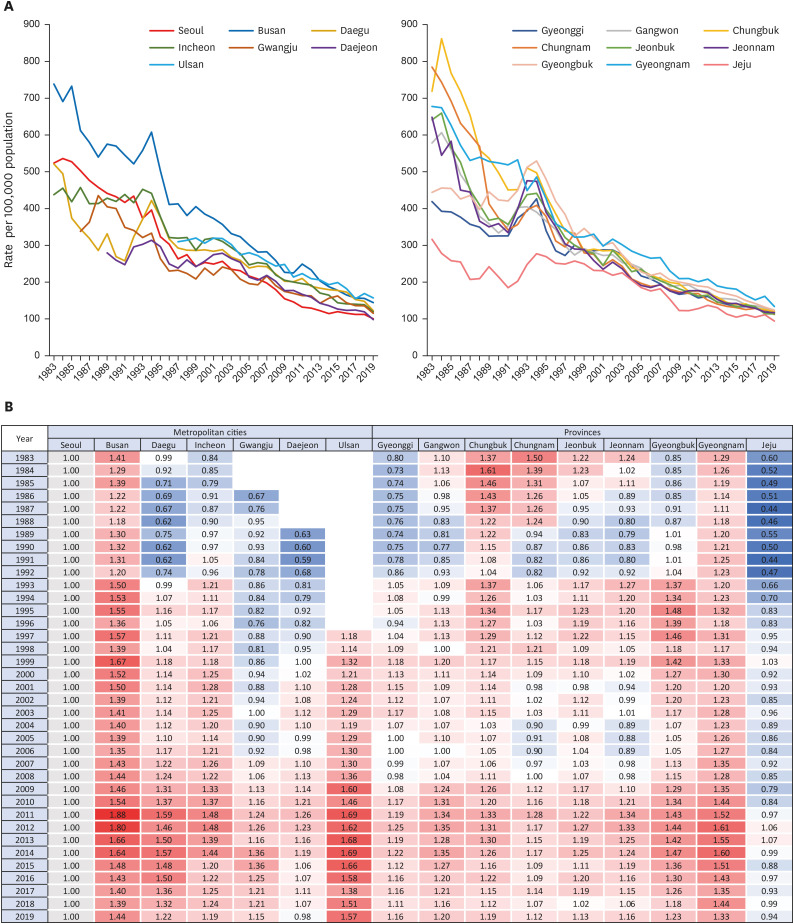
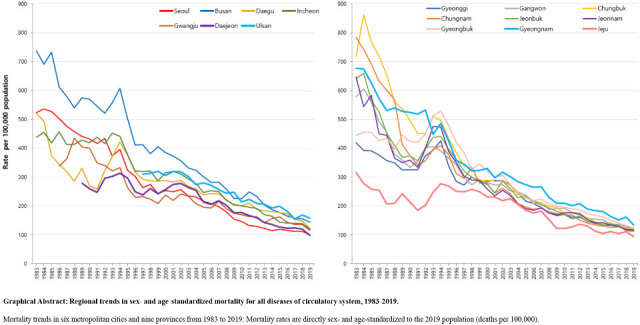
14) A previous study illustrated the 36-year trend of CVD death rates. Between 1983 and 2019, CVD mortality in Korea had remarkably improved, but continuous monitoring of the trends is still needed to reduce the health burden.
15) However, little research has focused on regional disparity in CVD mortality, and no study, to our knowledge, has illustrated its spatiotemporal trends. Although one study showed the cross-sectional geographic variation in CVD deaths in Korea, it was conducted using the combined data from 2011 to 2015.
16)
This study aimed to investigate the trends of CVD mortality according to the different regions in Korea from 1983 to 2019.
DISCUSSION
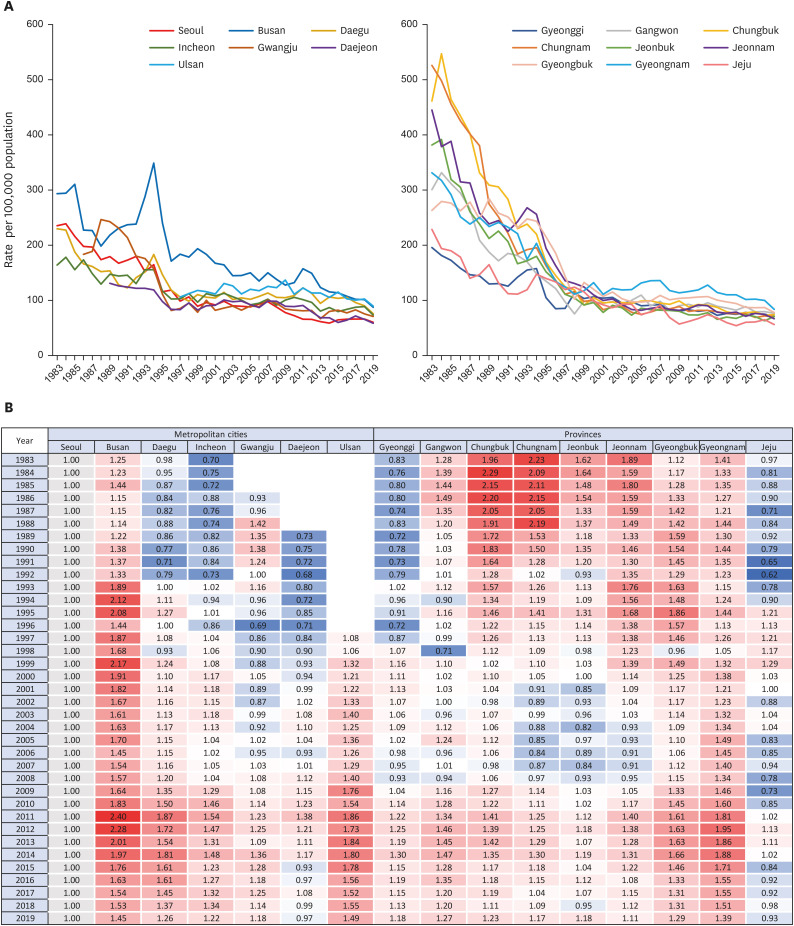
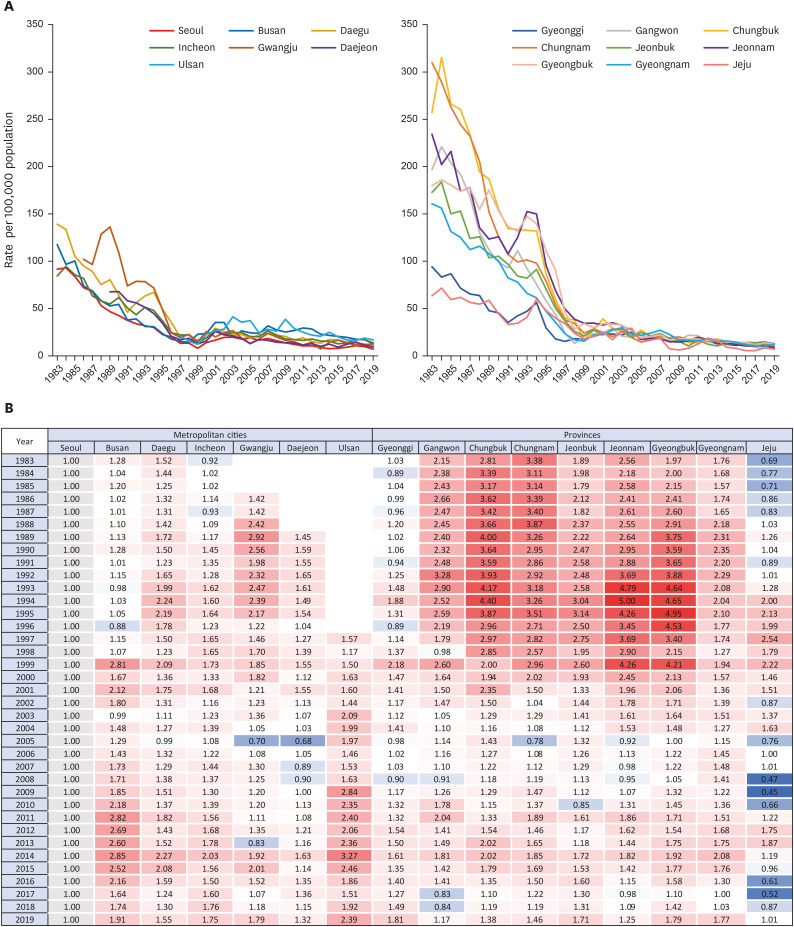
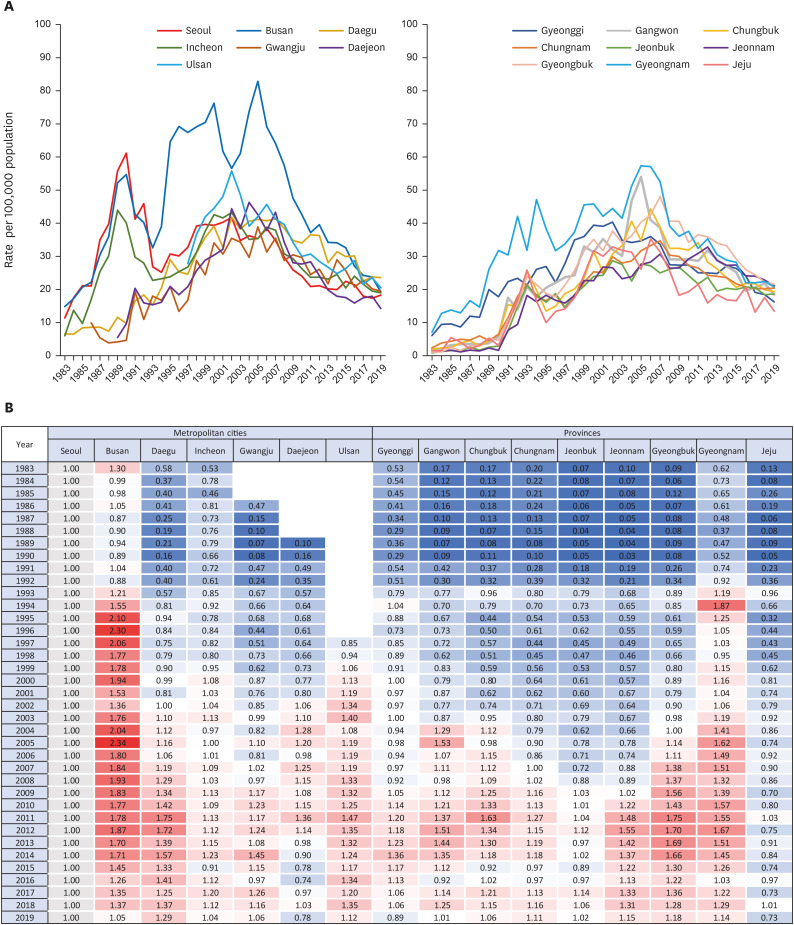
The overall trend of mortality from each CVD was similar across all regions. Mortality of HF increased across all regions; other CVD death rates showed a decreasing trend nationwide. Regional disparity in mortality was substantial in the early 1980s but converged over time. In all types of cardiovascular mortality, Busan, Ulsan and Gyeongnam remained at the top of the 17 regions, although they showed a downward trend like others. On the other hand, Jeju continued to have a relatively low CVD mortality rate while gradually closing the gap with other regions. Mortality in Seoul and other regions fluctuated and steadily converged. In most CVD-related deaths, other regions showed lower or similar rates than Seoul at the beginning of the observation but surpassed Seoul over time. Mortality from hypertensive heart diseases in other regions was much higher than in Seoul and Jeju at first. Despite the narrowing gap, rates in other regions remained higher. Both trends resulted in relatively lower burdens of deaths from the circulatory system in Seoul and Jeju in recent data.
There is little research on geographic variation in cardiovascular health or death in Korea. They have focused on the associations between CVD-related outcomes and regional characteristics such as urbanization and community economic status, rather than the region itself.
20) Ro and colleagues
21) analyzed the survival rate and the distribution of risk factors of out-of-hospital cardiac arrest according to urbanization. The rates for return of spontaneous circulation and survival were higher in metropolitan, urban, and rural areas in that order, whereas the age- and sex-adjusted incidence rates were higher in rural areas. The risk factors aggravating the survival rate were also greater in rural areas: no bystander cardiopulmonary resuscitation, longer medians of the response interval, and transportation to a lower-level emergency department.
21) Another study also identified rural disadvantages in the treatment and fatality rate of acute MI. Compared to Seoul, the odds ratio of receiving higher-quality medical management and invasive procedures in patients hospitalized with acute MI was estimated lower in other cities and rural areas in that order.
22)
The socioeconomic level of a community appears to have an impact on cardiovascular health-related mortality.
23)24) One study found that regions with a large number of basic livelihood recipients per 100,000 persons had a significant positive association with the standardized mortality from hypertensive disease.
25) Furthermore, populations in districts with a higher supply of health care resources, for instance, hospital beds, computed tomography scanners, and magnetic resonance imaging units, and greater utilization of local healthcare services had higher hospital admissions for CVD.
16) Given the different patterns in a correlation between CVD morbidity and mortality by 245 local districts, it implies that health care resources and utilization may affect the regional disparity in leading CVD morbidity to mortality.
While considering these implications of urbanization and community economic level for cardiovascular health, it is crucial to investigate the disparity in mortality by the administrative district as a target unit for national policymaking and intervention development. This analysis reveals varying degrees of CVD burden by region that were not observed when deaths in all regions were taken together. In particular, Busan, Ulsan, and Gyeongnam showed high mortality rates for all types of CVDs. This is consistent with a study showing regionally biased CVD mortality in certain regions of the United States: deaths from CVDs, IHD, hypertensive heart diseases, and cerebrovascular diseases were concentrated in Southeastern Oklahoma and Eastern Kentucky.
10) A range of possible causes was suggested including environmental exposures related to coal and metal mining, housing density, and access to health care.
10) Also, one study linked data from the surveillance system of behavioral risk factors and state-level coronary heart disease and stroke mortality data. They found significant state-level variation in the prevalence of poor cardiovascular health. It was partly attributable to median household income, taxes on soda drinks and cigarettes, and food and physical activity environments in a region.
26)
However, there is a considerable knowledge gap to fully explain the higher rates in Busan, Ulsan, and Gyeongnam or the relatively lower rate in Seoul and Jeju. Most regions in Korea are a combination of urban and rural areas and cannot be simply defined by community economic level. Each province has unique region-specific characteristics such as environment, lifestyle, and medical resources.
27) A Korean study suggested that regional disparity of CVD mortality results from the differences in the determinants such as regional socioeconomic level, physical environment, and health-related resources.
27) These factors may affect the CVD incidence and lead to a concentrated burden in Busan, Ulsan, and Gyeongnam. Previous studies reported that Busan had a high age-standardized incidence rate of acute MI.
28) CVD incidence, however, is not necessarily related to higher mortality. For instance, the incidence rate in Jeju was greater than in Busan, but the mortality rate was reversed showing a lower figure in Jeju.
28) This inconsistency may result from regional differences in risk-modifying factors linking incidence to mortality. In addition, misclassification when reporting the CVD diagnosis or the cause of death should be taken into consideration. With a thorough examination of the surveillance system especially in southeastern regions, further study can help us understand mortality disparity by regions in Korea. It needs to elucidate (1) exposure to metabolic, behavioral, and environmental risks, (2) delivery of interventions to modify CVD risk factors, and (3) access or utilization of high-quality medical care to improve outcomes when a CVD event occurs.
10)
Also, our study found that Busan showed multiple extreme surges in mortality. Except deaths from hypertensive heart disease and cerebrovascular disease, CVD-related mortality in Busan sharply increased and then decreased, particularly spikes in HF were noteworthy. A possible explanation for the surges is the misclassification of the cause of death. As mentioned, the mortality was higher than the incidence in Busan, and the death rates were extreme in the mid-1990s and the mid-2000s.
28) Given that, it is highly likely that there was misclassification in the diagnosis or coding system. To clarify the cause of the higher CVD burden in Busan, Ulsan, and Gyeongnam, the surveillance system on CVD should be strengthened at the local government and national levels in addition to the academic effort to determine risk factors in these regions.
Our study is the first study, to our knowledge, to examine long-term changes in the geographical variation of CVD mortality for the long period, of 36 years. The scope of previous studies investigating regional disparity was focused on regional characteristics or had a shorter period. Several limitations should also be considered. First, temporal analysis of mortality statistics based on death certificates is vulnerable to misclassification or diagnosis accuracy. During the study period, the KCD was revised 5 times.
17) Major revision in the coding system may have affected the mortality rate for each disease. Furthermore, since the cause of CVD death is mostly recorded by doctors, it may affect overreport or underreport according to doctors’ coding patterns, especially in rural regions where the number of hospitals is limited.
29) For instance, a study compared the causes of death in medical records with those in death certificates issued by a university hospital in 2003, and an accuracy of 61% was reported.
30) However, since the issued death certificate was supplemented and corrected by a standardized method, the accuracy rate of the cause of death in the published death statistics increased to 92%.
30) With the development and diagnostic tools over time, diseases that were previously difficult to be detected are properly classified, which may have affected the trends. Second, the limitation of analysis based on administrative divisions should be taken into account. It is not necessarily classified on the basis of population size or urbanization. For instance, Sejong city was designated as a metropolitan city in 2012 to ease the congestion of the capital. Also, null data were observed before 1986 for Gwangju, 1989 for Daejeon, and 1997 for Ulsan when they were subordinate to Jeonnam, Chungnam, and Gyeongnam, correspondingly.
In conclusion, a decline in cardiovascular mortality was experienced across all regions in Korea for 36 years. The regional disparity had substantially decreased compared to the 1980s. However, the relatively high burden of Busan, Ulsan, and Gyeongnam has not been resolved. To reduce premature CVD deaths, these regions call for action in terms of prevention and management of CVD, while facilitating the reduction of death rates in other regions.






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download