1. Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41. PMID:
7678184.

2. Hart RG, Diener HC, Coutts SB, et al. Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol. 2014; 13:429–438. PMID:
24646875.

3. Cohnheim J. Thrombosis and embolism. Lectures on General Pathology: A Handbook for Physicians and Students. Berlin: August Hirschwald;1877. p. 134.
4. Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984; 59:17–20. PMID:
6694427.

5. Elgendy AY, Saver JL, Amin Z, et al. Proposal for updated nomenclature and classification of potential causative mechanism in patent foramen ovale–associated stroke. JAMA Neurol. 2020; 77:878–886. PMID:
32282016.

6. Kim BJ, Sohn H, Sun BJ, et al. Imaging characteristics of ischemic strokes related to patent foramen ovale. Stroke. 2013; 44:3350–3356. PMID:
24072002.

7. Koutroulou I, Tsivgoulis G, Tsalikakis D, Karacostas D, Grigoriadis N, Karapanayiotides T. Epidemiology of patent foramen ovale in general population and in stroke patients: a narrative review. Front Neurol. 2020; 11:281. PMID:
32411074.

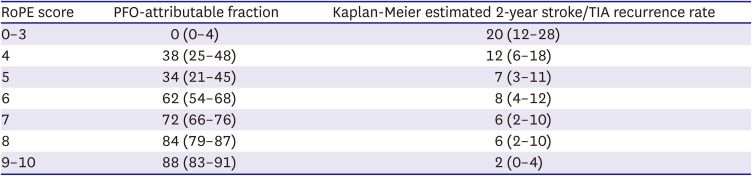
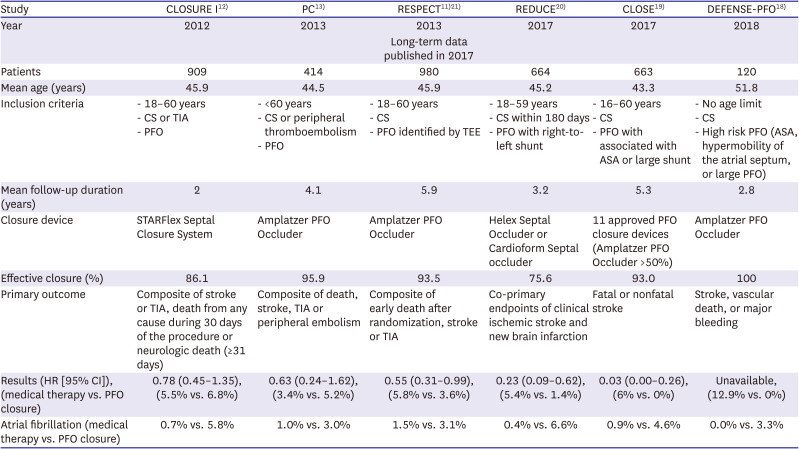
8. Kent DM, Ruthazer R, Weimar C, et al. An index to identify stroke-related vs incidental patent foramen ovale in cryptogenic stroke. Neurology. 2013; 81:619–625. PMID:
23864310.

9. Kent DM, Saver JL, Kasner SE, et al. Heterogeneity of treatment effects in an analysis of pooled individual patient data from randomized trials of device closure of patent foramen ovale after stroke. JAMA. 2021; 326:2277–2286. PMID:
34905030.
10. Alperi A, Guedeney P, Horlick E, et al. Transcatheter closure of patent foramen ovale in older patients with cryptogenic thromboembolic events. Circ Cardiovasc Interv. 2022; 15:e011652. PMID:
35735021.

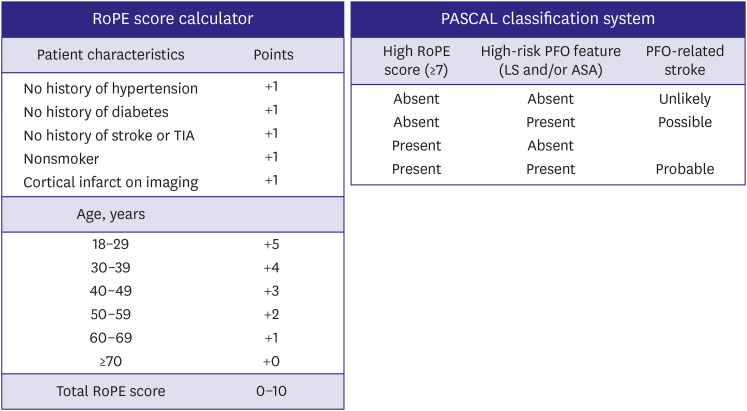
11. Carroll JD, Saver JL, Thaler DE, et al. Closure of patent foramen ovale versus medical therapy after cryptogenic stroke. N Engl J Med. 2013; 368:1092–1100. PMID:
23514286.

12. Furlan AJ, Reisman M, Massaro J, et al. Closure or medical therapy for cryptogenic stroke with patent foramen ovale. N Engl J Med. 2012; 366:991–999. PMID:
22417252.

13. Meier B, Kalesan B, Mattle HP, et al. Percutaneous closure of patent foramen ovale in cryptogenic embolism. N Engl J Med. 2013; 368:1083–1091. PMID:
23514285.

14. Spencer FA, Lopes LC, Kennedy SA, Guyatt G. Systematic review of percutaneous closure versus medical therapy in patients with cryptogenic stroke and patent foramen ovale. BMJ Open. 2014; 4:e004282.

15. Kent DM, Dahabreh IJ, Ruthazer R, et al. Device closure of patent foramen ovale after stroke: pooled analysis of completed randomized trials. J Am Coll Cardiol. 2016; 67:907–917. PMID:
26916479.
16. Khan AR, Bin Abdulhak AA, Sheikh MA, et al. Device closure of patent foramen ovale versus medical therapy in cryptogenic stroke: a systematic review and meta-analysis. JACC Cardiovasc Interv. 2013; 6:1316–1323. PMID:
24139929.

17. Rengifo-Moreno P, Palacios IF, Junpaparp P, Witzke CF, Morris DL, Romero-Corral A. Patent foramen ovale transcatheter closure vs. medical therapy on recurrent vascular events: a systematic review and meta-analysis of randomized controlled trials. Eur Heart J. 2013; 34:3342–3352. PMID:
23847132.

18. Lee PH, Song JK, Kim JS, et al. Cryptogenic stroke and high-risk patent foramen ovale: the DEFENSE-PFO trial. J. J Am Coll Cardiol. 2018; 71:2335–2342. PMID:
29544871.
19. Mas JL, Derumeaux G, Guillon B, et al. Patent foramen ovale closure or anticoagulation vs. antiplatelets after stroke. N Engl J Med. 2017; 377:1011–1021. PMID:
28902593.

20. Søndergaard L, Kasner SE, Rhodes JF, et al. Patent foramen ovale closure or antiplatelet therapy for cryptogenic stroke. N Engl J Med. 2017; 377:1033–1042. PMID:
28902580.

21. Saver JL, Carroll JD, Thaler DE, et al. Long-term outcomes of patent foramen ovale closure or medical therapy after stroke. N Engl J Med. 2017; 377:1022–1032. PMID:
28902590.

22. Hart RG, Sharma M, Mundl H, et al. Rivaroxaban for stroke prevention after embolic stroke of undetermined source. N Engl J Med. 2018; 378:2191–2201. PMID:
29766772.

23. Diener HC, Sacco RL, Easton JD, et al. Dabigatran for prevention of stroke after embolic stroke of undetermined source. N Engl J Med. 2019; 380:1906–1917. PMID:
31091372.

24. Kim HK, Tantry US, Park HW, et al. Ethnic difference of thrombogenicity in patients with cardiovascular disease: a pandora box to explain prognostic differences. Korean Circ J. 2021; 51:202–221. PMID:
33655720.

25. Cho H, Kang J, Kim HS, Park KW. Ethnic differences in oral antithrombotic therapy. Korean Circ J. 2020; 50:645–657. PMID:
32725974.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download