This article has been
cited by other articles in ScienceCentral.
Author's summary
Further research is required to understand the relationship between coronavirus disease 2019 (COVID-19) and the risk of cardiovascular disease. Risks based on specific genetic predispositions, host factors such as underlying diseases, or virus characteristics such as the type of variant still need to be clarified. Furthermore, it is necessary to monitor the duration of the effects of long-COVID. Finally, it is necessary to explore whether such acceptable alternatives that can reduce this risk exist.
Go to :

Abstract
Studies showing that coronavirus disease 2019 (COVID-19) is associated with an increased risk of cardiovascular disease continue to be published. However, studies on how long the overall cardiovascular risk increases after COVID-19 and the magnitude of its long-term effects have only been confirmed recently. This is partly because the distinction between cardiovascular risk as an acute complication of COVID-19 or post-acute cardiovascular manifestations is ambiguous. Long-COVID has arisen as an important topic in the second half of the pandemic. This term indicates that symptoms persist for more than two 2 months; following three months of SARS-CoV-2 infection and cannot be explained by other medical conditions. Despite the agreement of these international organizations and experts, it is difficult to define whether there is sufficient medical evidence to prove the existence of long-COVID. However, the Korean government and Korea Disease Control and Prevention Agency (KDCA) are preparing a new platform to assess the long-term impact of COVID-19. Using this data, a prospective cohort of 10,000 confirmed COVID-19 cases will be established. This cohort will be linked with claims data from the National Health Insurance Services (NHIS) and it is expected that increased real-world evidence of long-COVID will be accumulated.
Go to :

Keywords: COVID-19, Long-COVID, COVID-19 vaccination, Cardiovascular risk
RESPIRATORY INFECTIONS AS RISK FACTORS FOR CARDIOVASCULAR DISEASE
Acute myocardial infarction (AMI) and stroke are serious cardiovascular events with substantial morbidity and mortality. While these diseases are closely associated with chronic underlying conditions and behavioral risk factors, acute infections, such as influenza and pneumonia, are also known to increase the risk of AMI and stroke.
1)
A self-controlled case series study conducted in Ontario
1) concisely demonstrated the effects of respiratory viral infections, particularly influenza, on AMI. This study showed that in laboratory-confirmed influenza infection, the incidence of AMI increased 6.05-fold (95% confidence interval [CI], 3.86–9.50) for 1 week from the date of sample collection compared to that in the control period. This study was designed to minimize the effects of other confounding variables, providing high-level evidence from real-world data.
This association has also been supported by a meta-analysis of case-control studies. This meta-analysis was performed on a total of 10 studies in 2015,
2) confirming that recent influenza infection or influenza-like illness was more frequent in AMI cases than the general population, with a pooled odds ratio (OR) of 2.01 (95% CI, 1.47–2.76). Although this study design did not show the extent to which influenza acts as a risk factor, it nevertheless suggested that there is already consistent evidence to support that respiratory viral infections such as influenza can be considered a cardiovascular risk.
Go to :

CORONAVIRUS DISEASE 2019 AS A RISK FACTOR FOR CARDIOVASCULAR DISEASES
Studies showing that coronavirus disease 2019 (COVID-19) is associated with an increased risk of AMI or stroke continue to be published. The earliest data suggesting COVID-19 as a cardiovascular risk factor was provided by a retrospective cohort study conducted in New York City.
3) In the first half of 2020, about 1.6% of emergency room visits or hospitalizations after COVID-19 infection experienced an ischemic stroke, which showed an adjusted OR of 7.6 (95% CI, 2.3–25.2) compared to that of the control group, which was influenza-infected. This indicates that the risk of thrombotic events after COVID-19 infection may be very high, even when compared to other respiratory viral infections.
However, studies on how long the overall cardiovascular risk increases after COVID-19 and the magnitude of its long-term effects have only been confirmed recently. This is partly because the distinction between cardiovascular risk as an acute complication of COVID-19 or post-acute cardiovascular manifestations is ambiguous. In addition, clarification of long-term effects requires tracking of a large population; however, active follow up is challenging because of the impact of the pandemic.
The United States Department of Veterans Affairs established a large post-COVID-19 follow-up database and compared the results with contemporary and historical controls to track cardiovascular outcomes over one year. The results showed that the risk increased in most areas, including cerebrovascular disorders, dysrhythmia, inflammatory heart diseases, and thrombotic disorders, even if they were excluded within 30 days after infection. In particular, a significant increase in disease burden was observed with a hazard ratio of 1.55 (95% CI, 1.50–1.60) in major adverse cardiovascular events (a composite of myocardial infarction, stroke, and all-cause mortality). These results indicate that the effects of COVID-19 on the cardiovascular system are maintained for at least one year, and that active interventions are required to reduce this risk.
Go to :

INCREASED CARDIOVASCULAR RISK AND LONG-CORONAVIRUS DISEASE
Long-COVID has arisen as an important topic in the second half of the pandemic. This condition has been reported empirically in people infected with COVID-19, and the United Kingdom (UK) National Institute for Health and Care Excellence guideline
4) defines long-COVID as a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection with persistent symptoms continuing for more than 4 weeks. Subsequently, the World Health Organization established a comprehensive definition of long-COVID as a “Post-COVID-19 condition.” This term indicates that symptoms persist for more than 2 months; following three months of SARS-CoV-2 infection and cannot be explained by other medical conditions.
5)
Despite the agreement of these international organizations and experts, it is difficult to define whether there is sufficient medical evidence to prove the existence of long-COVID. First, the disease groups and symptoms are widely dispersed, pathophysiological mechanisms have not been fully elucidated, and it is unclear whether this condition is a common symptom after all infections, or a psychological condition caused by a shock of the pandemic. Finally, sufficient evidence has not been accumulated regarding the extent to which these conditions differ from the baseline incidence rate without exposure to infection.
However, the long-term risk of COVID-19 to the cardiovascular system is a topic that could be investigated as a potential scientific and specific explanation of long-COVID. Accumulating evidence suggests that infection may act as an additional cardiovascular risk factor, along with chronic conditions and lifestyle; there is also evidence to suggest that the risk increases with COVID-19. Therefore, interventions that can reduce the cardiovascular risk of COVID-19 may be helpful in the fight against long-COVID.
Go to :

ASSOCIATION OF VACCINATION AND REDUCTION OF CARDIOVASCULAR RISK IN RESPIRATORY VIRAL INFECTIONS
As an association between influenza and cardiovascular disease has already been definitively established, careful evaluations have also been made to determine whether vaccination can reduce this risk. In a meta-analysis of eight case-control studies,
2) influenza vaccination was found to be significantly associated with AMI (pooled OR, 0.71; 95% CI, 0.56–0.91). Furthermore, in a meta-analysis of three endpoints in 2 clinical trials,
6) influenza vaccination was found to lower the relative risk of cardiovascular death to 0.39 (95% CI, 0.20–0.77) in a Mantel-Haenszel fixed-effect model. This indicates that vaccination of high-risk populations against seasonal influenza has additional health benefits along with a direct vaccine effect, and this may explain why vaccination should be continued despite continuous attacks on seasonal national immunization programs.
7)
Evidence has also been published to suggest an association between the COVID-19 vaccine and cardiovascular risk.
8) One study using data from the Korean nationwide COVID-19 database compared the incidence rates of AMI and ischemic stroke between 30 and 120 days after infection in breakthrough infected individuals who had received two vaccinations, and group of non-vaccinated people. The fully vaccinated group was significantly older than the unvaccinated group and had a higher prevalence of diabetes, hypertension, and dyslipidemia; however, the risk of AMI and stroke was significantly lower. This study suggests that the vaccine may have the same effect as influenza in the increased cardiovascular risk associated with COVID-19 infection, which further re-emphasizes the importance of vaccination in the population at high-risk of cardiovascular disease.
Go to :

PITFALLS OF THE ASSOCIATION ASSESSMENT AMONG RESPIRATORY VIRAL INFECTION, VACCINATION, AND CARDIOVASCULAR RISK
Despite the various studies mentioned above, it is difficult to determine whether this evidence has a high level of causality. First, although there are insufficient mechanisms to fully explain the role of vaccines in reducing cardiovascular risk of respiratory viral infections, a sufficient pathophysiological mechanism to explain this relationship has not yet been elucidated. Second, mediations must also be considered. Unlike confounding factors, mediation has not yet received sufficient attention in the evaluation of real-world evidence. Mediation refers to the third hypothetical variable that can explain or confirm the observed relationship between independent and dependent variables. For example, in the association between COVID-19 vaccination and cardiovascular risk, there is varying evidence to suggest that intensive care unit admission for severe COVID-19 may be a strong risk factor for cardiovascular disease. This could therefore be considered a short-term complication rather than a long-term effect of COVID-19. If the association between COVID-19 vaccination and the risk of cardiovascular disease is due to vaccination-induced reduced severity, the effectiveness of severe COVID-19 prevention may mediate this causal flow. Fortunately, studies in South Korea have shown consistent results, even when excluding severe COVID-19, which is not likely to be a mediator. However, there is always the possibility of hidden mediation and confounding unless a clear pathophysiological mechanism can be revealed.
Third, the real-world study design has an inherent limitation. Because exposure to SARS-CoV-2 cannot be randomized, long-COVID studies should mainly rely on an observational design, and selection of a control group is important. Most studies used historic controls (patients treated prior to the COVID-19 pandemic) or selected contemporary controls (such as those with influenza-like illnesses). However, the use of these controls may not be sufficient to address differences in underlying characteristics, changes in time, and over-/under-reporting. Some studies have attempted to overcome this problem by using self-controlled designs. However, it is difficult to evaluate intervention compared to exposure; if one of the baseline properties changes depending on the intention to intervene, such as vaccination, the same problem as seen in other study designs is repeated.
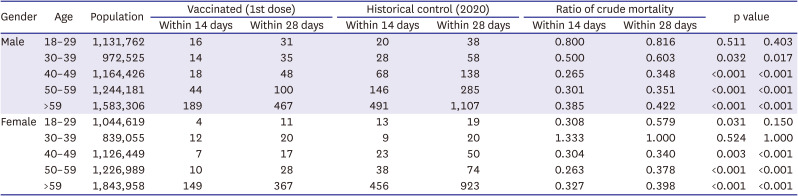
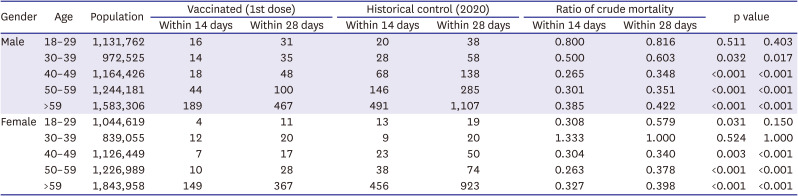
The last factor is the effect of a healthy vaccine. To evaluate the real-world evidence that occurs after vaccination, this confounding factor must be considered. This effect is frequently observed in evaluations of vaccine safety and effectiveness. Additionally, in crude mortality assessment based on the vaccination status for COVID-19 (
Table 1),
9) the crude mortality rate of vaccinated people is lower than that of unvaccinated people in most age groups in Korea. This succinctly shows how far reaching the vaccine effect can be, even in healthy individuals.
Table 1
Comparison of crude mortality after 2021 COVID-19 vaccination versus 2020 historical control
|
Gender |
Age |
Population |
Vaccinated (1st dose) |
Historical control (2020) |
Ratio of crude mortality |
p value |
|
Within 14 days |
Within 28 days |
Within 14 days |
Within 28 days |
Within 14 days |
Within 28 days |
|
Male |
18–29 |
1,131,762 |
16 |
31 |
20 |
38 |
0.800 |
0.816 |
0.511 |
0.403 |
|
30–39 |
972,525 |
14 |
35 |
28 |
58 |
0.500 |
0.603 |
0.032 |
0.017 |
|
40–49 |
1,164,426 |
18 |
48 |
68 |
138 |
0.265 |
0.348 |
<0.001 |
<0.001 |
|
50–59 |
1,244,181 |
44 |
100 |
146 |
285 |
0.301 |
0.351 |
<0.001 |
<0.001 |
|
>59 |
1,583,306 |
189 |
467 |
491 |
1,107 |
0.385 |
0.422 |
<0.001 |
<0.001 |
|
Female |
18–29 |
1,044,619 |
4 |
11 |
13 |
19 |
0.308 |
0.579 |
0.031 |
0.150 |
|
30–39 |
839,055 |
12 |
20 |
9 |
20 |
1.333 |
1.000 |
0.524 |
1.000 |
|
40–49 |
1,126,449 |
7 |
17 |
23 |
50 |
0.304 |
0.340 |
0.003 |
<0.001 |
|
50–59 |
1,226,989 |
10 |
28 |
38 |
74 |
0.263 |
0.378 |
<0.001 |
<0.001 |
|
>59 |
1,843,958 |
149 |
367 |
456 |
923 |
0.327 |
0.398 |
<0.001 |
<0.001 |

Go to :

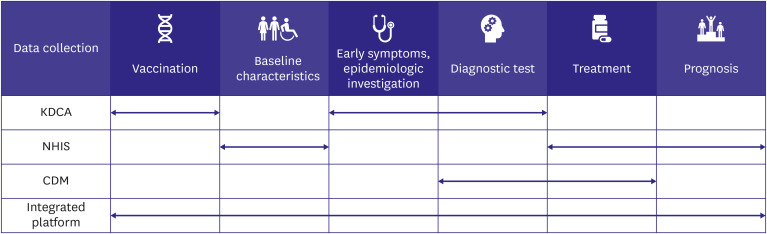
KOREA’S PREPARATIONS TO ASSESS CORONAVIRUS DISEASE 2019 AND LONG-TERM CARDIOVASCULAR RISK
The Korean government and Korea Disease Control and Prevention Agency (KDCA) are preparing a new platform to assess the long-term impact of COVID-19. Using this data, a prospective cohort of 10,000 confirmed COVID-19 cases will be established. The registry collects comprehensive long-COVID data through questionnaires, blood tests, symptom monitoring, radiology tests, and translational approaches for confirmed COVID-19 cases. This cohort will be linked with claims data from the National Health Insurance Services (NHIS) and will be tracked for more than four years. Authorities are also merging a comprehensive big-data platform for COVID-19. Data such as confirmatory PCR test results, vaccination history, variant surveillance data, and reports of vaccine adverse events from the KDCA were combined with claims data collected by the NHIS. A database including more than a dozen topics has already been constructed, and it is expected that increased real-world evidence of long-COVID will be accumulated (
Figure 1).
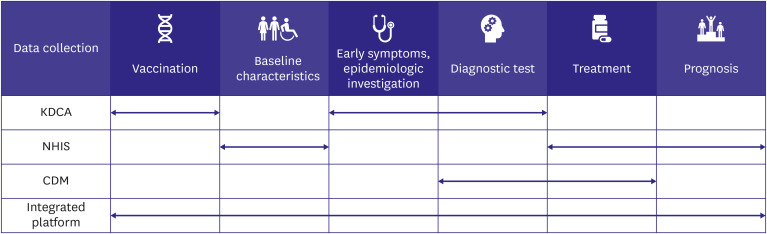 | Figure 1
The concept of Korean COVID-19 big-data platform.
CDM = Common Data Model; COVID-19 = coronavirus disease 2019; KDCA = Korea Disease Control and Prevention Agency; NHIS = National Health Insurance Services.

|
Further research is essential to understand the relationship between COVID-19 and the risk of CVD. First, it is necessary to evaluate the risks regarding specific genetic predispositions, host factors such as underlying diseases, or virus characteristics such as the type of variant. These data will help select risk groups and focus on interventions. Second, it is necessary to monitor the duration of the effects of long-COVID. There is evidence to suggest that COVID-19, unlike influenza, can have a relatively long-lasting effect. However, long-term follow-up is needed to closely evaluate the duration of these effects. Finally, it is necessary to explore whether acceptable alternatives can reduce this risk. A Korean
8) study provided low-quality evidence to indicate that a 2-dose vaccination regimen could reduce cardiovascular risk. If this is true, it will be necessary to further determine whether third/fourth doses or oral treatment can lead to further risk reduction.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download